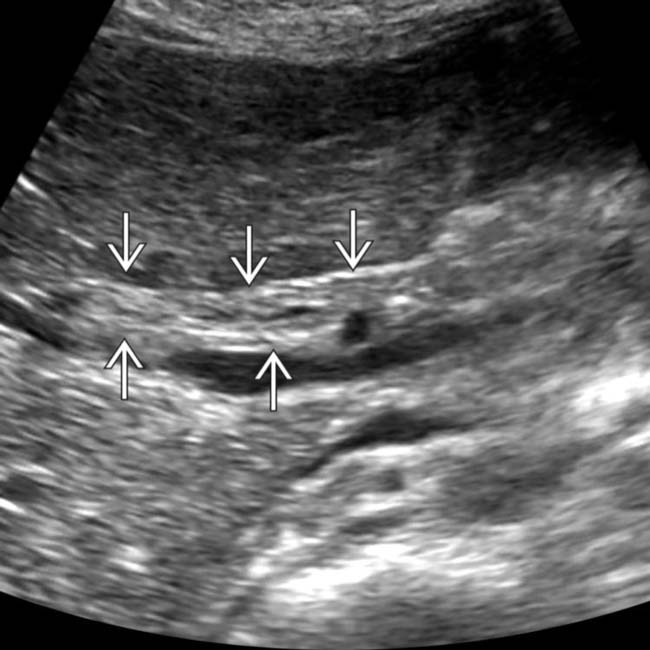
Dilation of intrahepatic ± extrahepatic ducts with abrupt cut off at site of obstruction

 and adjacent free fluid
and adjacent free fluid  , characteristic of ascending cholangitis.
, characteristic of ascending cholangitis.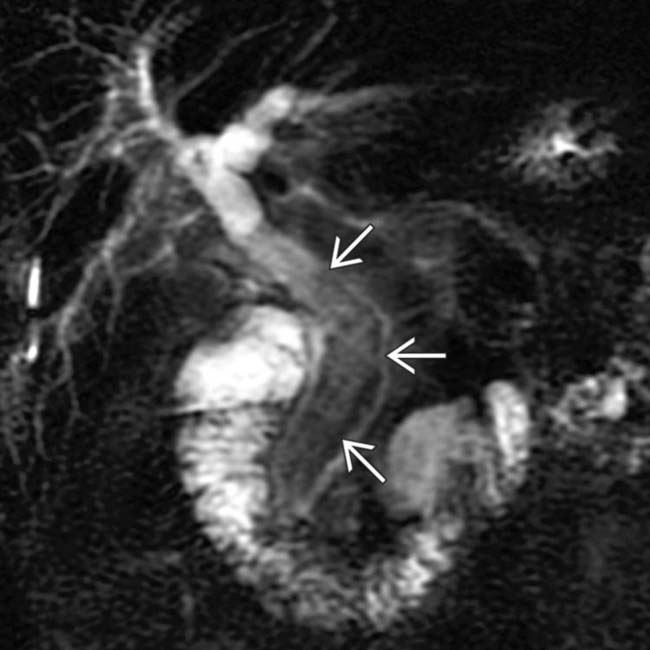
 .
.
 with a small amount of adjacent fluid
with a small amount of adjacent fluid  , suggesting ascending cholangitis.
, suggesting ascending cholangitis.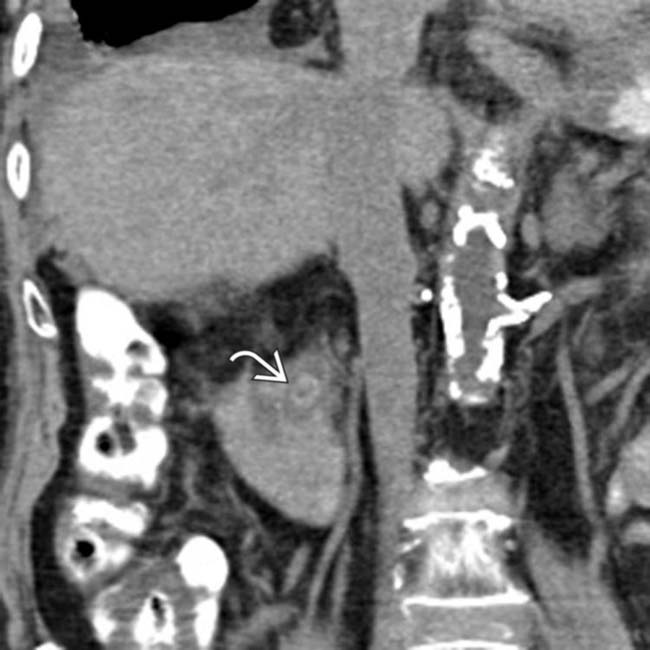
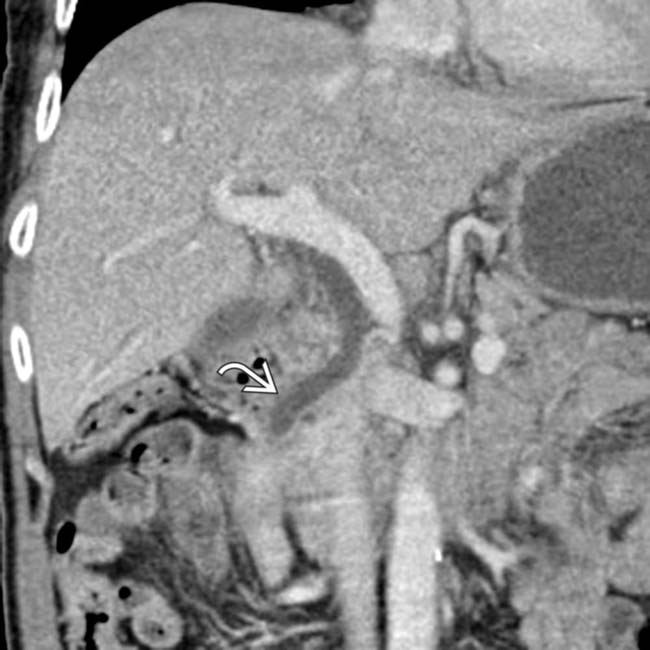
 as the cause of the patient’s cholangitis.
as the cause of the patient’s cholangitis.IMAGING
General Features
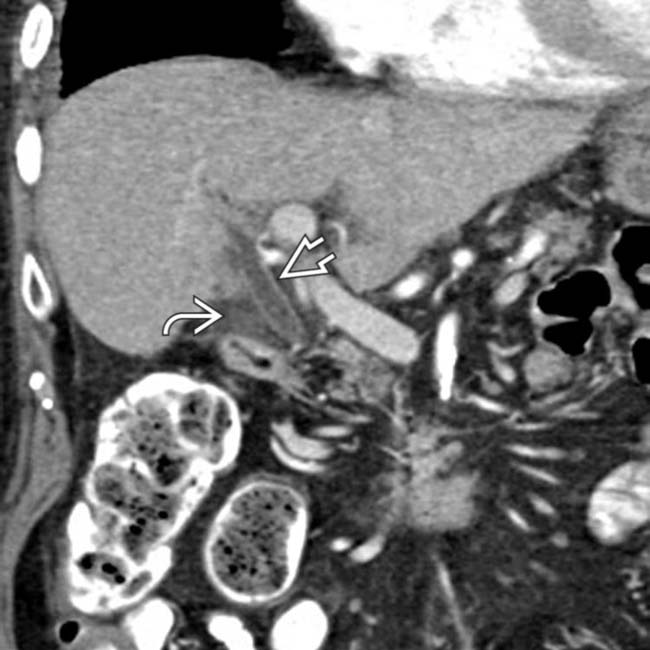
CT Findings
• Dilation of intrahepatic ± extrahepatic ducts (depending on level of obstruction) with abrupt “cut-off” at site of obstruction
MR Findings
• Intrahepatic biliary dilatation almost always present ± extrahepatic ductal dilatation
• Presence of intermediate to low T2WI and intermediate T1WI signal purulent material (pus) within bile ducts
• Bile duct walls appear thickened on T1WI and T2WI with progressive hyperenhancement of duct walls on T1WI C+
PATHOLOGY
General Features
• Etiology
 Pathogenesis
Pathogenesis
 Pathogenesis
Pathogenesis
– Stone/stricture → obstruction → bile stasis → ↑ biliary pressure → infection
 Biliary tree normally sterile due to bacteriostatic bile salts, mechanical barrier of sphincter of Oddi, and hepatocyte tight junctions
Biliary tree normally sterile due to bacteriostatic bile salts, mechanical barrier of sphincter of Oddi, and hepatocyte tight junctions
 Biliary tree normally sterile due to bacteriostatic bile salts, mechanical barrier of sphincter of Oddi, and hepatocyte tight junctions
Biliary tree normally sterile due to bacteriostatic bile salts, mechanical barrier of sphincter of Oddi, and hepatocyte tight junctionsCLINICAL ISSUES
Presentation
 , suggestive of cholangitis.
, suggestive of cholangitis.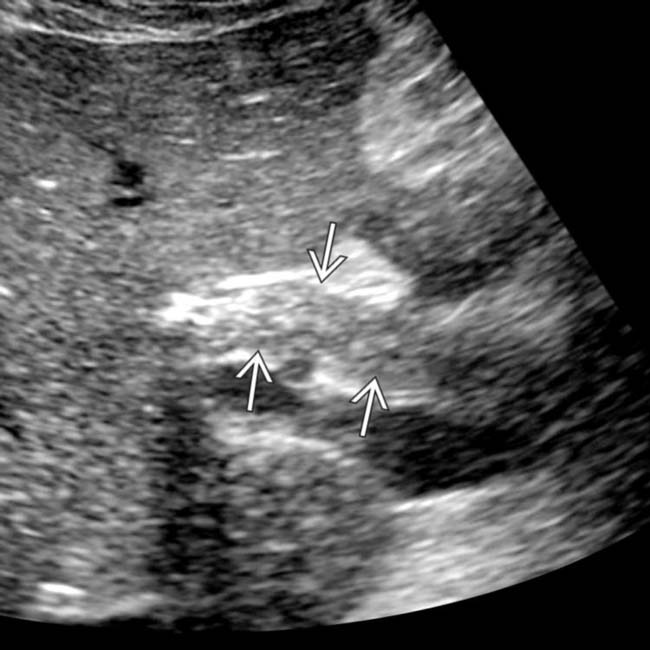
 . An obstructing distal stone and abundant pus were identified at ERCP, compatible with cholangitis.
. An obstructing distal stone and abundant pus were identified at ERCP, compatible with cholangitis.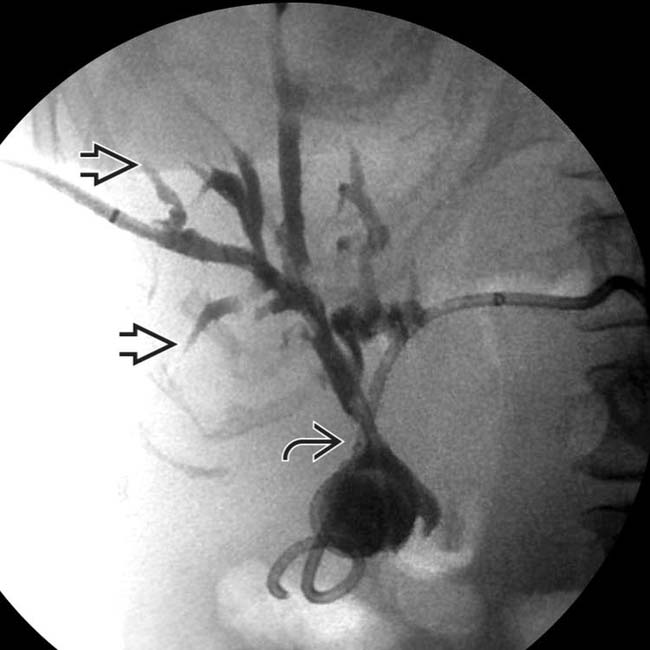
 and proximal ductal dilation. Note the irregular arborization of the ducts and the abrupt “arrowhead” terminations
and proximal ductal dilation. Note the irregular arborization of the ducts and the abrupt “arrowhead” terminations  , characteristic of cholangitis.
, characteristic of cholangitis.
 . This narrowing is likely due to inflammatory wall thickening associated with bacterial infection.
. This narrowing is likely due to inflammatory wall thickening associated with bacterial infection.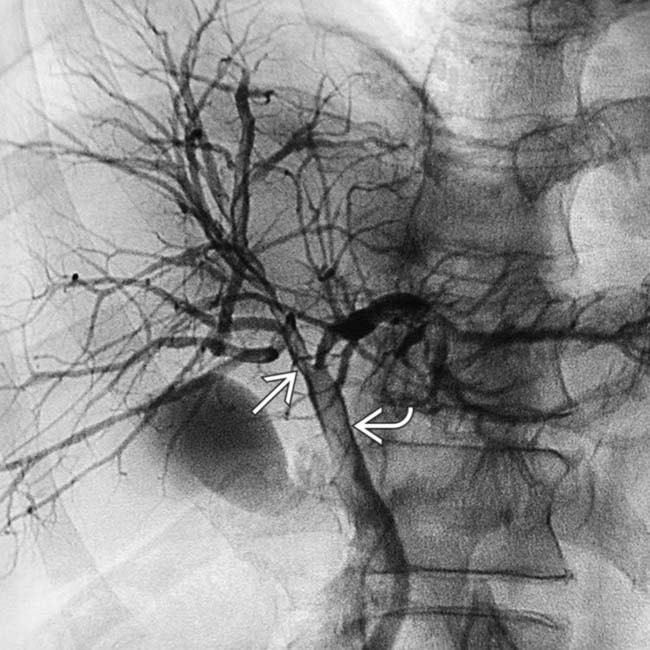
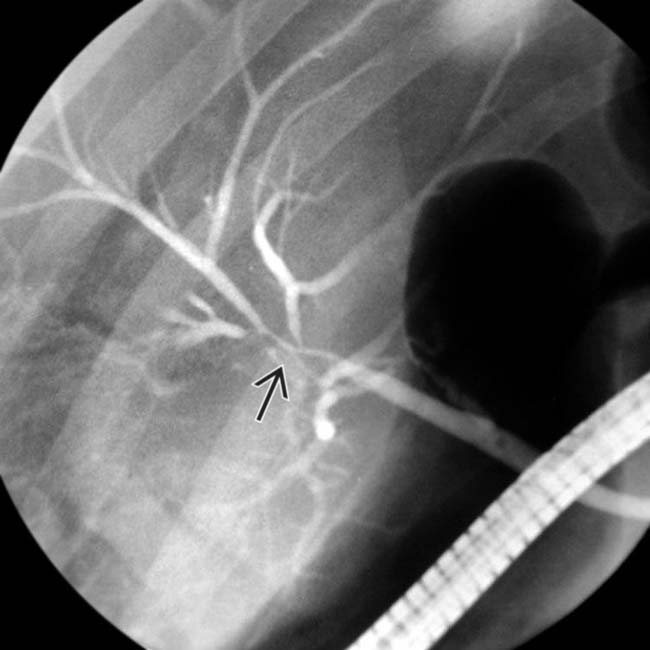
 . The filling defect
. The filling defect  within the CBD is a blood clot attributable to the imaging procedure.
within the CBD is a blood clot attributable to the imaging procedure.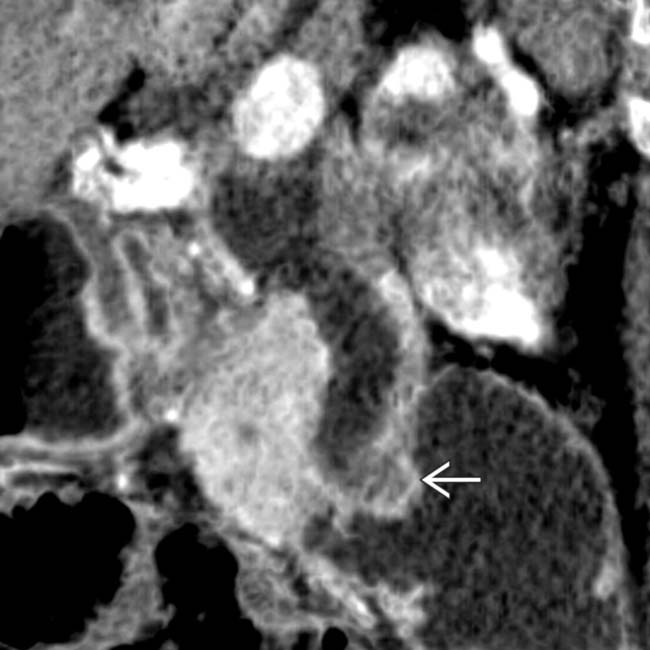
 .
.






















































 with subtle thickening and enhancement of the bile duct wall, suggesting ascending cholangitis. While not visible on CT, multiple stones were found at ERCP.
with subtle thickening and enhancement of the bile duct wall, suggesting ascending cholangitis. While not visible on CT, multiple stones were found at ERCP.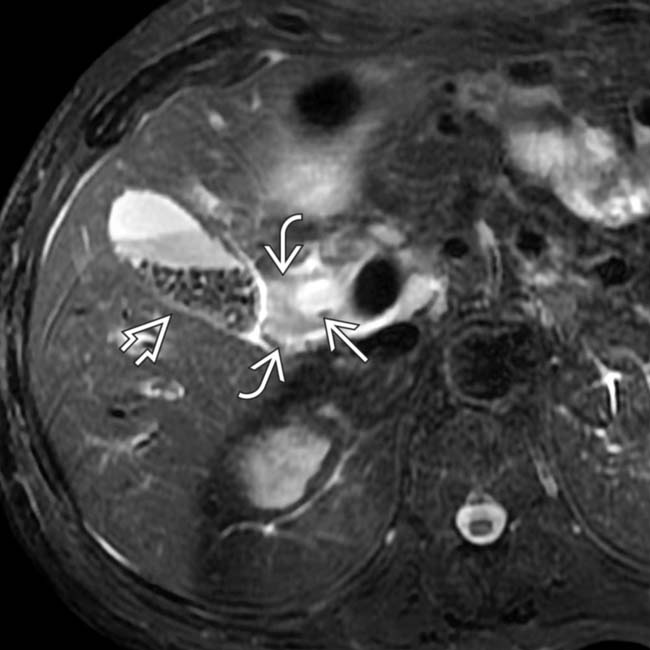
 , periductal edema
, periductal edema  , and multiple gallstones
, and multiple gallstones  .
.


