CHAPTER 49 Articular Injuries in the Athlete
INTRODUCTION
Activities such as throwing, lifting, and gymnastics cause large stresses across the elbow joint, which can result in a multitude of pathologies.16,21,90 In skeletally immature athletes, these stresses, combined with the developing bony anatomy and unique physeal biomechanics, lead to distinct injury patterns. In the past, macrotrauma, such as fractures and dislocations, were common in this age group; but recently, there has been a paradigm shift. As more children have begun participating in organized athletics at younger ages, and, as sport specialization with a year-round focus has become more common, repetitive microtrauma is causing a prevalence of overuse injuries. These include syndromes affecting the ligaments, capsule, muscles, and articular surfaces of the joint.2,17 Additionally, osseous manifestations may occur, such as stress fractures, osteophytes, loose bodies, osteochondral lesions and epiphyseal or apophyseal hypertrophy, and avulsion, or fragmentation.44 To better understand the injuries suffered in youth athletes, a thorough understanding of the bone and cartilage anatomy and knowledge of the forces associated with different overhead activities is required.
Adult throwers may present with loose bodies and stress fractures as well. However, more commonly, patients in this age group present with symptoms consistent with chronic valgus insufficiency, such as valgus extension overload, lateral compression injuries, and medial tension injuries.4,64,117,118 Acute fractures and dislocations may occur in athletes of any age with a frequency comparable to that of the general population, but these injuries are less common than ligamentous instability.32,35
ANATOMY
BONE AND CARTILAGE
Elbow anatomy, including the ossification centers and pattern of ossification in the elbow, is discussed in detail in Chapters 1 and 2. Elbow injury patterns in skeletally immature athletes are associated with stages of growth and development; the skeletal developmental stage defines the weakest link. Childhood terminates with the appearance of all secondary centers of ossification, adolescence terminates with the fusion of all secondary ossification centers, and young adulthood is signified by the completion of skeletal growth.90 Injuries during childhood are related to the developing epiphyses. Excessive forces may alter vascularization or ossification. During adolescence, peripheral fragment avulsions, subchondral osteonecrosis, or physeal injury or nonunion may occur. By the time patients reach young adulthood, stress reactions become more typical, as do ligamentous or capsular injuries.90
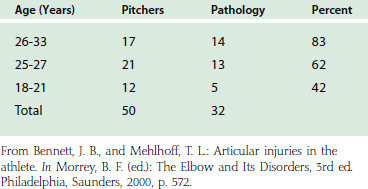
Accessory ossicles are of particular anatomic concern to physicians treating articular injuries. These may occur extra-articularly (medial epicondyle or tip of the olecranon in the triceps tendon) or intra-articularly (olecranon fossa, coronoid fossa, lateral epicondyle)45 (Figs. 49-1 and 49-2). Persistent apophyses at the medial or lateral epicondyle may be confused with loose bodies. Sesamoid fabella cubiti in the biceps tendon, patella cubiti in the triceps tendon, or accessory ossicles such as the supratrochlear posterius in the olecranon fossa or the os supratrochlear anterius in the coronoid fossa must also be distinguished from pathologic loose bodies.120
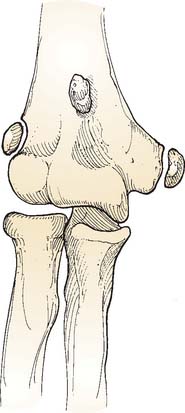
FIGURE 49-1 Accessory ossicles, medial and lateral epicondyle apiphysis about the elbow joint (anteroposterior view).
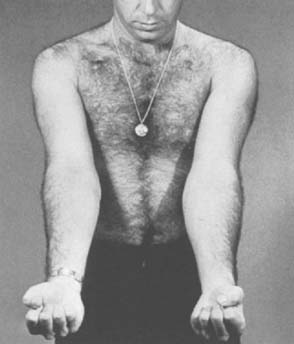
(Redrawn from Bennett, J. B., and Mehlhoff, T. L.: Articular injuries in the athlete. In Morrey, B. F. [ed]: The Elbow and Its Disorders, 3rd ed. Philadelphia, Saunders, 2000, p. 563.)
LIGAMENTS
Ligamentous anatomy in the elbow region is discussed at length in Chapters 2, 47, and 48. A brief review of their functional anatomy as it relates to articular injuries is presented here.
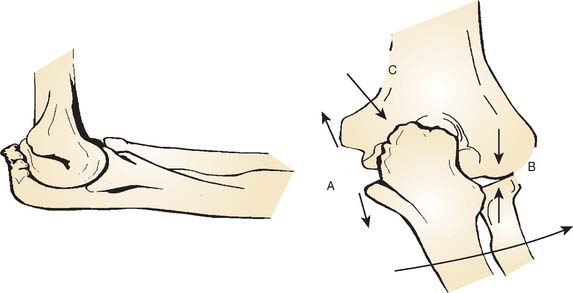
The ulnar collateral ligament (UCL) complex consists of three main portions: the anterior band, the posterior band, and the transverse ligament. The anterior band serves as the primary stabilizer to valgus stress, with the radiocapitellar joint providing secondary stability.27,80,97 Repetitive valgus stresses associated with activities such as throwing generate three, well-described forces on the elbow and its articular surfaces: (1) medial tension, (2) lateral compression, and (3) posterior shear (Fig. 49-3).30,107 Microtrauma to the anterior band of the UCL may cause progressive valgus laxity, which causes an alteration of the basic biomechanics of the joint. Shear forces on the olecranon develop, leading to synovitis, osteophytes, and loose bodies in the posterior compartment. Additionally, an increase in compressive forces is transmitted to the radiocapitellar joint. Fragmentation, loose bodies, or both may result. These changes in the elbow articulation may result in well-described clinical findings, such as increased valgus carrying angle, flexion contractures, medial epicondyle hypertrophy or fragmentation, and trochlear or olecranon fragmentation.42,54,90
DIAGNOSIS
HISTORY
A detailed history helps narrow the extensive differential diagnosis of elbow pain in athletes (Table 49-1). We find it most helpful to classify injuries by mechanism, with further subclassification based on anatomic compartment involved (medial, lateral, posterior) and onset of pain (acute, chronic). Pertinent information includes age, sport played, level of competition, position, characterization of pain (location, duration, onset), mechanism of injury, and past medical history. As mentioned earlier, skeletal age can provide the physician with useful information regarding the likely diagnosis.
Different sports predispose athletes to different injuries. Gymnasts must lock out their elbows to support their body weight, causing posterior elbow injuries.93 Baseball players, especially pitchers, put large magnitude valgus stresses on the elbow, which can result in myriad injuries. For pitchers in particular, effectiveness over their previous outings, numbers of pitches thrown, types of pitches thrown, phase of throwing associated with the pain, and parent’s or coach’s observations of any changes in mechanics are pertinent. A detailed knowledge of the phases of throwing will help the treating physician narrow the differential diagnosis of elbow pain in throwers. This is discussed at length in Chapter 47. It is important to note that number of pitches thrown and not innings pitched is what places throwers at risk for injury.93
PHYSICAL EXAMINATION
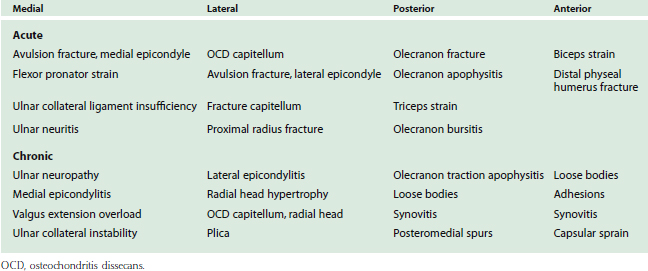
Bilateral upper extremities should be examined, beginning with inspection to note muscle atrophy or hypertrophy, bony deformities, elbow asymmetry, or flexion contractures.20 Range of motion of both shoulders and elbows is tested, and carrying angles of the elbows should be compared (Fig. 49-4). Palpation should include the medial and lateral epicondyles, the medial and lateral collateral ligaments, the sublime tubercle, the radial head, and the olecranon process. Careful examination of the ulnar nerve may reveal subluxation, tenderness, or both. Lateral ligaments are tested with varus stress and internal rotation of the arm, whereas medial ligament stability is tested with a valgus stress applied to an externally rotated arm. Special maneuvers used to help diagnose elbow medial collateral ligament (MCL) insuffiency include the moving valgus stress test and the milking test, both of which are detailed in Chapters 4 and 46. Pain with forced hyperextension may suggest hyperextension valgus overload syndrome, whereas mechanical locking or catching may indicate loose bodies or osteochondral defects. In throwing athletes, it may help to have them simulate a pitch to reproduce their symptoms. The examination requires a complete neurologic and vascular assessment, with special attention given to the ulnar nerve.
IMAGING
Standard anteroposterior (AP), lateral, and reverse axial views of both the affected and contralateral elbow are an essential part of the workup. Stress views may help detect subtle ligamentous instability; however, negative stress films do not rule out ligamentous pathology. Magnetic resonance imaging (MRI) can be used in these cases to further evaluate the ligament in question. Additionally, MRI is helpful for diagnosing osteochondritis dissecans (OCD) lesions, stress fractures, and other soft tissue pathology. Computed tomographic (CT) scans are also useful to evaluate loose bodies, bone spurs, and articular cartilage lesions.
ARTHROSCOPY
Arthroscopy of the elbow can facilitate or confirm diagnosis of both articular and ligamentous injuries (Fig. 49-5). For example, OCD lesions can be inspected and probed at arthroscopy, which can help dictate the appopriate treatment; the arthroscopic valgus stress test can be used to confirm disruption to the medial UCL.8,12 Chapters 38, 39, and 41 detail the expanding role of arthroscopy of the elbow in the treatment cartilage and synovial lesions in the athlete, such as lateral synovial plicas, loose bodies, OCD lesions, and posterior compartment osteophytes.24,31,51
MEDIAL TENSION INJURIES IN ADOLESCENCE
MEDIAL EPICONDYLAR STRESS LESIONS (LITTLE LEAGUER’S ELBOW)
The term Little League elbow was originally used by Bennett to describe the spectrum of bony changes caused by medial tensile forces and lateral compressive stresses in young, developing throwers.17 In these athletes, the repetitive tensile stress on the medial epicondyle caused by valgus stress and the pull of the flexor-pronator muscle mass and the medial UCL leads to microtrauma at the epiphysis.2,3,36,37,88–90 The resulting spectrum of injury at the medial epicondyle includes subtle widening, separation, fragmentation, and hypertrophy (Fig. 49-6). A recent study revealed that up to 63% of little leaguers had soreness at the medial epicondyle, and of these throwers, 70% exhibited separation and 40% had evidence of fragmentation.48

FIGURE 49-6 Radiograph of medial epicondylar stress lesion demonstrating fragmentation and separation.
Clinically, patients may present with progressively worsening, medial-sided elbow pain that is exacerbated with throwing. A triad of symptoms has been described, which includes pain in the late cocking and early acceleration phases, loss of velocity and distance, and decreased throwing effectiveness. On examination, there is point tenderness at the medial epicondyle and a flexion contracture. Patients have pain with valgus stress, but no frank instability. Radiographic findings range from subtle widening to separation or fragmentation. Medial epicondylar stress lesions are benign entities that respond well to cessation from throwing and, if flexion contractures are present, physical therapy for stretching. A return to throwing is predicated on complete resolution of symptoms and the absence of tenderness on examination. A gradual return using a strict throwing program emphasizing proper mechanics is critical.
It is important to recognize that, at times, the term Little Leaguer’s elbow is used as a “wastebasket diagnosis” to refer to a constellation of injuries including medial epicondylar avulsion fractures, medial epicondyle apophysitis, OCD, Panner’s disease, hypertrophy of the ulna, olecranon apophyseal injury, and medial UCL injury.3,41,45,71,99,102 In this context, the term is nonspecific and not helpful for tailoring treatment. When evaluating young throwers with medial elbow pain, it is important to make a specific diagnosis.
MEDIAL EPICONDYLE AVULSION FRACTURES
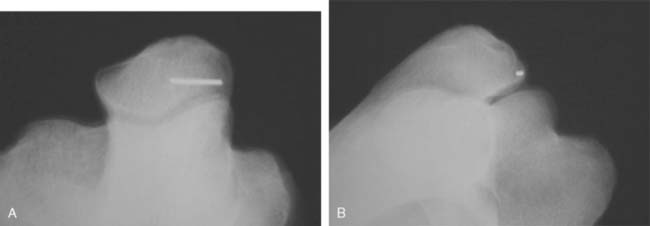
When a significant, acute, valgus stress is applied through a violent muscle contracture such as during the throwing motion or arm wrestling, an avulsion fracture of the medial epicondyle can result.72,84 Separation classically occurs through the epiphyseal growth plate, because this is the weakest area of the epicondyle. Clinically, this results in tenderness over the epicondyle and, often, a flexion contracture that may be greater than 15 degrees. Assessment of ulnar nerve function is critical, and physicians must maintain a high index of suspicion for a spontaneously reduced elbow dislocation. Radiographs confirm the diagnosis. A view that we have found particularly useful to evaluate the medial epicondylar apophysis in children is the posterior impingement view as described by John Conway (John Conway Personal communication, 2002)34 (Fig. 49-7A and B). It is an axial view with the elbow maximally flexed and the humerus externally rotated 40 degrees. The x-ray beam is directed perpendicular to the humeral axis. Additionally, this view is useful to visualize the posterior medial olecranon margin in cases of valgus extension overload.
Woods and colleagues123 have classified the lesions based on patient age and fragment size. Type I injuries occur in younger patients. These are large fragments typically involving the entire apophpysis with the MCL, and the fragments often displace and rotate. Type II fractures occur in adolescents. These fragments are usually smaller, representing an avulsion of the flexor origin. The anterior oblique ligament is usually intact.
Treatment depends on the amount of fragment displacement, although the definition of acceptable displacement is controversial. Less than 3 to 5 mm of displacement is typically well tolerated and responds well to splinting for 2 to 3 weeks, followed by conversion to a hinged elbow orthosis.59 Operative indications include displacement greater than 3 to 5 mm, fragment rotation, valgus instability, ulnar nerve dysfunction, and fragment incarceration (Fig. 49-8). An increasing number of authors are advocating more aggressive treatment of these injuries in competitive, skeletally immature overhead athletes using more then 2 mm of displacement as an indication to operate.53 This is based on studies showing that subtle instability after non-operative management causes degenerative radiocapitellar changes.53
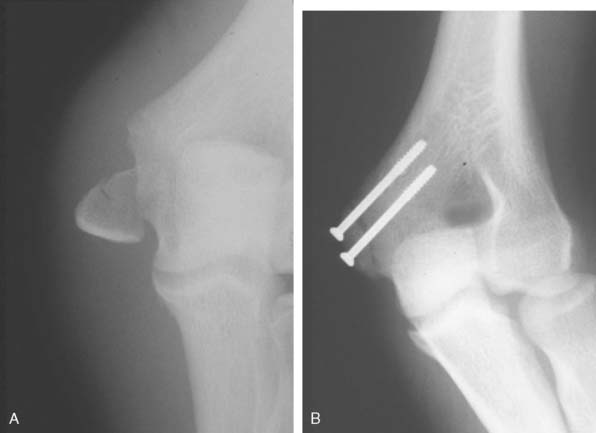
FIGURE 49-8 A, Medial epicondyle fracture. B, Medial epicondyle fracture treated with internal fixation.
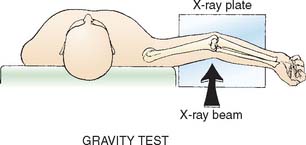
Gravity Stress Test
Schwab and associates105 described a radiograph using gravity to impart a valgus stress to help diagnose instability. With the patient lying supine, the shoulder is brought into maximum external rotation (Fig. 49-9). At this point, the sagittal plane of the elbow is parallel to the floor, and the weight of the forearm is resisted solely by the flexor forearm mass and anterior oblique ligament. Instability of the elbow, secondary to loss of MCL continuity, is indicated by movement of the fragment distally. A positive gravity stress test is an indication for surgical treatment.
MEDIAL LIGAMENT INSTABILITY
Injuries of the medial UCL are relatively uncommon in younger throwing athletes; however, there has been an alarming trend of increasing numbers of high school–aged athletes being treated for UCL insufficiency.93 The increasing incidence of these throwers requiring UCL reconstruction may be directly related to overuse of the throwing arm and throwing breaking balls at youngerages.93 Clinically, these patients usually have subtle findings of instability on examination. The previously described gravity stress test is sometimes useful in diagnosing UCL injury, although MRI is usually a better imaging modality (Fig. 49-10).
Treatment options include direct surgical repair or ligament reconstruction.54,57 According to Jobe, direct repair is indicated if stability can be restored; otherwise reconstruction with a tendon graft should be performed. Petty et al.93 found that the results of UCL reconstruction in high school athletes are less successful than the results in older age groups. For a more complete discussion of UCL injury diagnosis and treatment, please refer to Chapter 47.
LATERAL COMPRESSION INJURIES IN ADOLESCENCE
OSTEOCHONDRITIS DISSECANS OF THE CAPITELLUM
OCD of the capitellum is a disease of unclear etiology that typically affects patients aged 10 to 15 years.71,124 The most commonly accepted theory is that the lesion is secondary to vascular insufficiency.88,124 Several authors have noted the association between throwing and OCD.1,2,6,13 Tullos and King concluded that compressive forces between the capitellum and radial head occur during the throwing motion.118 Schenk and Dalinka104 showed that a biomechanical mismatch between the radial head and capitellum exist. Together, these studies support the theory that compressive forces produce focal arterial injury and subsequent bone death (or OCD lesions).
The focal lesions usually occur in the dominant arm and cause pain and a flexion contracture of 15 degrees or more. A joint effusion is often present. Initial radiographs may be normal. As the disease progesses, irregularities of the capitellum or even a defect in the bone can develop. Loose bodies may be present. Takahara described the use of a 45-degree flexion AP elbow radiograph to reveal lesions that may be underestimated by conventional radiographs110,112 (Fig. 49-11A and B).
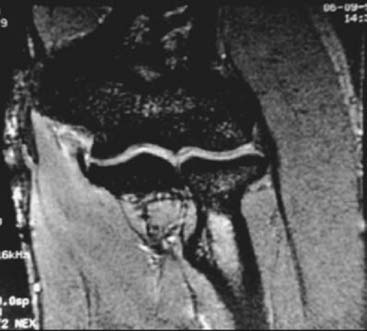
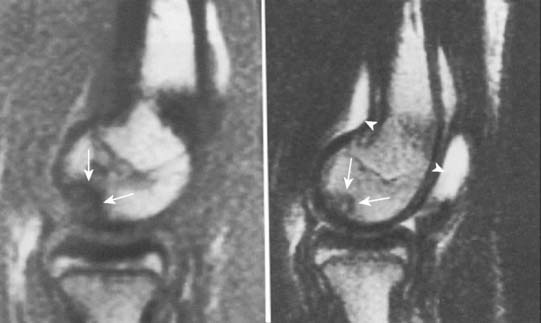
Arthrograms, ultrasound, and MRI are useful imaging modalities.50,112 The sensitivity and specificity of MRI make it particularly valuable in diagnosing capitellar lesions19 (Fig. 49-12). Decreased signal on T1-weighted images and increased signal on T2-weighted and fast spin–echo sequences are consistent with marrow edema, and are often present before similar changes are seen on plain film.66,104 MR arthrograms are helpful to demonstrate unstable lesions that are not loose bodies.104 It is important to note that there is a normal anatomic sulcus between the lateral condyle and capitellum that may be mistaken for an osteochondral fragment.66 This sulcus is located posteriorly, whereas OCD lesions are usually located more anteriorly.
It is imperative to differentiate OCD of the capitellum from osteochondrosis of the capitellum, or Panner’s disease. Panner’s disease is characterized by disordered ossification of the capitellum with degeneration and necrosis, followed by regeneration and ossification.89 The proposed mechanism involves an alteration in the vascularity of the developing capitellum.101 Age, radiographic findings, the presence of loose bodies, and deformity of the capitellum help to distinguish between the two entities (Table 49-2). Panner’s disease most commonly affects children between the ages of 5 to 10 years. Similar to patients with OCD of the capitellum, patients may complain of dull, aching lateral-sided elbow pain that is aggravated by activity. Unlike OCD, however, flexion contractures are not common. Radiographically, the disease is characterized by fragmentation and deformity of the ossific nucleus of the capitellum66 (Fig. 49-13). Unlike OCD, Panner’s disease is a self-limited process that rarely results in loose body formation. It responds well to conservative treatment, and the capitellum usually heals without late deformity or collapse. Young athletes with Panner’s disease should be restricted from throwing and gymnastics to prevent axial loading and valgus stress to the elbow.54
TABLE 49-2 Comparison of OCD of the Capitellum and Panner’s Disease
| Osteochondritis Dissecans | Panner’s Disease | |
|---|---|---|
| Age | Teens | ∼10 years |
| Onset | Insidious | Acute |
| Radiographic finding | Island of subchondral bone demarcated by a rarefied zone | Fragmentation of entire capitellar ossific nucleus |
| Loose bodies | Present | Absent |
| Residual deformity of capitellum | Present | Minimal |
From Bennett, J. B., and Mehlhoff, T. L.: Articular injuries in the athlete. In Morrey, B. F. (ed.): The Elbow and Its Disorders, 3rd ed. Philadelphia, Saunders, 2000, p. 569.
The natural history of OCD is much less predictable. There are no good criteria to predict healing; and late sequelae, such as loose bodies and residual deformity, do occur. Takahara and colleagues111 treated 24 patients with OCD nonoperatively and found that the lesions had a poor tendency to heal, and that if there was any fragment instability, failure was likely. Because of the inherently poor potential for unstable lesions to heal, they are usually treated surgically. Treatment is guided by lesion classification. The most important factor in staging OCD lesions is determining whether or not the fragment has separated.
Intact, stable capitellar lesions (Type Ia) respond well to conservative treatment, which includes rest, anti-inflammatory medications, early splinting for acute symptoms, and a gradual return to activity when asymptomatic.92
Surgery is indicated for intact, stable lesions that fail conservative measures and for all unstable lesions (Type Ib, II, III).15,49,92,113 Treatment options include removal of loose bodies, microfracture, abrasion chondroplasty, internal fixation of larger lesions, osteochondral autograft transfer, and drilling of lesions.67,70,75,113–115 Most of these techniques are now performed arthroscopically. Baumgarten et al.15 developed an arthroscopic classification system that helps guide which treatment option would be best. Grade 1 lesions have smooth but soft ballotable cartilage, and they respond well to drilling.56 Grade 2 lesions exhibit fibrillation or fissuring of cartilage. In these cases, cartilage should be débrided back to a stable rim, then drilling, microfracture or abrasion chondroplasty should be performed.5,15,18,22,25,69,75 Grade 3 lesions have exposed bone with a fixed fragment, and grade 4 lesions are loose but nondisplaced fragments. These two stages have traditionally been treated with removal of the fragment, followed by drilling, microfracture, or chondroplasty. Grade 5 lesions are loose bodies, and along with removal of the fragment, they are treated in a similar manner to grade 3 or 4 lesions.
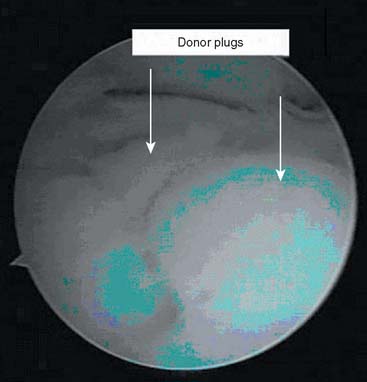
In the short-term, the above-mentioned options seem to improve patients’ symptoms.15,18 However, long-term results indicate impairment of elbow function.14,78,111 In one series with an average follow-up of 23 years, 50% of patients had restricted motion, and 61% had degenerative changes on radiographs.14 Mixed results have also been reported regarding the ability of patients to return to competitive athletics.24,75,115 Newer treatment options aim to improve outcomes. Kiyoshige et al.65 described the use of a lateral closing wedge osteotomy of the capitellum to treat OCD in seven adolescent baseball players. Preliminary results were promising, with 86% having complete relief of symptoms and return to full activity. Osteochondral autograft transplantation and mosaicplasty for grade 3 and 4 lesions have shown promise; however, longer term follow-up is necessary to better elucidate their efficacy in the treatment of OCD of the capitellum (Fig. 49-14).5,55,125
Chappell and ElAttrache28 recently presented their results treating capitellar OCD lesions. Five patients with lesions involving the lateral column of the capitellum with engagement of the radial head were treated with arthroscopic autologous osteochondral allografts. Three out of the five patients had excellent outcomes, and all five returned to their previous level of sports participation. Fifteen patients with OCD lesions were treated with microfracture. Eleven were available for follow-up, of which all returned to previous levels of sports competition. Based on the above-mentioned findings, it may be that the location of the OCD lesion may be more important than lesion size. Lateral OCD lesions compromise lateral column support, which bear a large portion of the valgus forces generated by athletes during overhand motions. Chapter 39 provides an in-depth discussion of the above-mentioned techniques.
POSTERIOR EXTENSION AND SHEAR INJURIES IN ADOLESCENCE
OSTEOCHONDROSIS OF THE OLECRANON
Olecranon apophyseal injuries are rare, but they can affect young athletes, including divers, gymnasts, hockey players, and throwing athletes.33,73,106 The etiology is unknown, although several theories have been advanced. Some authors implicate repetitive microtrauma to the olecranon apophysis during the acceleration phase of throwing.91,120 Gore et al.44 maintained that a traction apophysitis, similar to what occurs at the medial epicondyle, is the causative mechanism. Others propose a connection to Osgood-Schlatter disease, with rapid growth and musculotendinous imbalance resulting in an apophysitis.53,76
Clinically, patients complain of activity-related pain with swelling and tenderness around the olecranon process. On plain films, fragmentation and irregularity of the apophysis are visible. Widening may occur.26 Opposite elbow films must be obtained, and the contralateral apophysis must be closed to make the diagnosis. Activity restriction or brief immobilization with a gradual return to sports usually provides a successful outcome.82 Indications for operative treatment include the persistence of symptoms despite more than 3 to 6 months of conservative treatment or radiographically documented failure of apophyseal closure despite nonsurgical management.26 In these cases, open reduction and internal fixation using a single cancellous screw, with or without a tension band, can provide excellent results with minimal complications.26,98
OLECRANON STRESS FRACTURES
Stress fractures of the olecranon have been reported in throwing athletes, gymnasts, and weight lifters.4,13,74,77,87,93,109,121 These injuries result from the persistent abutment of the olecranon into its fossa, traction from the triceps during the deceleration phase of throwing, and from valgus forces causing impaction of the medial olecranon onto the medial wall of the olecranon fossa.4,64 Different predominating forces cause different fracture configurations: Triceps traction and extension forces lead to transverse fractures, whereas valgus and extension forces create oblique fractures.109 In fact, oblique stress fractures have been shown to occur in combination with partial medial UCL injuries.109
On examination, tenderness occurs over the poste-rior and posteromedial olecranon. Patients often lack extension. Because valgus stress testing may elicit pain in both the olecranon and the medial UCL, Suzuki recommends performing the milking maneuver at 90 degrees of flexion to prevent the olecranon from engaging in the olecranon fossa. This helps differentiate valgus extension overload syndrome from medial UCL injury.109 Radiographs may demonstrate a fracture line or sclerosis (Fig. 49-15). MRI and bone scan have also been used to make or confirm the diagnosis of stress fracture.
Tension band constructs and compression screws have both been used successfully.43,68,95,121 Orava and Hulkko87 recommended screw compression for oblique fractures and tension band constructs for transverse fracture lines. Arthroscopy can be used with screw fixation to diagnose associated lesions and to view the intra-articular part of the stress fracture.26 Charlton and Chandler29 treated skeletally immature athletes who had persistence of their olecranon physis with operative stabilization and autogenous bone graft. All patients returned to their prior level of play.
ACUTE INSTABILITY IN ADULTS
ELBOW DISLOCATIONS WITH ASSOCIATED FRACTURES
The incidence of elbow dislocations is second only to glenohumeral dislocations, with about 10% resulting from athletic activities.23 Successful management of simple elbow dislocations typically consists of minimal immobilization, followed by early, aggressive range of motion.60 However, when associated injuries occur with dislocations, recommended treatment often differs. Fractures associated with elbow dislocations include radial head fractures (5% to 10% frequency), epicondyle avulsions (12%), and coronoid or olecranon fractures (10%).23,52,60,108,119
The radial head serves as an important secondary stabilizer to valgus stress. This is particularly true after elbow dislocations, when the medial UCL is compromised. In nonathletes, reconstruction of the radial head may be sufficient to restore stability and to allow the ligament to heal. In athletes, however, the increased valgus stress that these patients apply to their elbow necessitates repair of the ligament as well.23,79
Arthroscopy can play a role in both the evaluation and management of nondisplaced fractures of the radial head in athletes.31,58 It allows for recognition of associated soft tissue injuries including medial UCL injury, lateral collateral ligament insufficiency, and annular ligament disruption. Osteochondral defects and loose bodies can also be identified and treated. Short-term results show that a satisfactory outcome can be obtained treating minimally displaced fractures with arthroscopic reduction and fixation.100 Contraindications to the use of arthroscopy in the setting of acute trauma include severe soft tissue swelling, previous history of an ulnar nerve transposition, and largely displaced intra-articular fractures.
OLECRANON FRACTURES
Olecranon fractures have been classified and discussed in Chapter 25. When discussing the appropriate management of these fractures in athletes, it is important to understand the effect of olecranon resection on elbow stability.7,61,62 An et al.7 looked at the effect of partial removal of the proximal ulna on elbow stability in the context of comminuted olecranon fractures. They showed that constraint of the ulnohumeral joint was linearly proportional to the area of remaining articulation. More recently, biomechanical studies showed that as the amount of posteromedial olecranon resected increased, more valgus stress was generated.61 This led to increased strain in the medial UCL. These studies imply that all attempts should be made to restore the normal anatomy of the olecranon in throwing athletes.
CHRONIC VALGUS INSUFFICIENCY IN ADULTS
THROWING INJURIES
Throwing places unique stresses on the elbow that can be detrimental to the integrity of the joint.36,40,47 The injury patterns that result in this group of athletes are fairly predictable; however, the radiographic findings and symptoms do worsen with age, so prompt diagnosis and treatment is beneficial (Table 49-3). Slocum classified the typical throwing injuries of the elbow into three groups: (1) medial tension injuries, (2) lateral compression injuries, and (3) extensor overload injuries.107 Medial tension injuries include UCL tears, flexor-pronator tendonitis, and ulnar nerve injuries. These medial-sided injuries are discussed in detail in Chapter 47. Laterally, compressive forces between the radial head and capitellum result in chondromalacia and loose body formation. In the posterior compartment, shear forces result in valgus extension overload.122 In many throwers, valgus instability, as evidenced by UCL insufficiency, and valgus extension overload can coincide. It is critical to detect the presence of both, because a failure to do so results in a failure of treatment.
LOOSE BODIES
The use of arthroscopy to treat elbow pathology is discussed in detail in Chapters 37 to 39; however, it is worth noting that arthroscopy is a particularly useful diagnostic and treatment tool for loose bodies in the elbow.8,86
VALGUS EXTENSION OVERLOAD
Stability in the thrower’s elbow is provided by a combination of ligamentous, articular, and muscular re-straints. Initially, valgus torque is primarily resisted by the medial UCL, with secondary stability provided by the radiocapitellar joint and by the olecranon. As the elbow nears full extension, the articular constraints play a more prominent role in ensuring stability.81 With excessive valgus force or increased UCL laxity, olecranon impingement occurs.64 In addition to valgus forces, during the throwing motion, the flexor muscles help resist the large extension force that is generated during the acceleration phase.38,39 If the deceleration force is not well controlled by the muscles, the olecranon traumatically abuts the posterior compartment. The combination of valgus and extension forces causing posterior and posteromedial olecranon osteophytes has been termed valgus extension overload.9,107,122 In cases of isolated valgus extension overload, patients may report pain in the medial aspect of the elbow during both the acceleration and deceleration phases of throwing. Posterior impingement can cause a loss of extension, and osteophytes that fracture may result in loose bodies. Radiographic evaluation, which should include posterior, lateral, and axial views of the elbow, may identify posteromedial osteophytes or loose bodies (Fig. 49-16). In patients with an appropriate history and radiographic findings, diagnosis is confirmed by a positive valgus extension overload test.26 Pain elicited in the posterior compartment with manual pronation, valgus, and extension force applied is consistent with a positive test.

FIGURE 49-16 Posteromedial osteophyte consistent with valgus extension overload in the elbow of a 22-year-old baseball pitcher.
A trial of nonoperative treatment consisting of rest, correction of throwing mechanics, and physical therapy emphasizing flexor-pronator mass strengthening may be warranted; however, Andrews and Timmerman9 noted that posteromedial olecranon impingement is the most common diagnosis requiring surgery in baseball players. Previously, surgical treatment involved osteophyte excision and loose body removal through an arthrotomy.122 This provided successful results; however, given the advantages of decreased morbidity and increased visualization of the entire joint, arthroscopy is becoming the preferred treatment option. Studies have reported that arthroscopic treatment of valgus extension overload can effectively return professional athletes to their previous level of competition.9,51,96 In the study conducted by Reddy et al., athletes with loose bodies or posterior impingement tended to have improved outcomes compared with those with degenerative joint disease.4,96 Andrews and Timmerman believed that arthroscopic osteophyte excision was technically superior to open excision; however, they emphasized that this is a palliative procedure in athletes with a high level of recurrence if they return to play.26
SYNOVIAL LESIONS
Synovial plicae are believed to be normal anatomic structures that represent remnants of embryonic septae formed during development.63,85 Repetitive microtrauma can cause thickening and inflammation of these plicae, which can cause pain and mechanical symptoms in the elbow joint. Typically these symptoms occur in throwing athletes and golfers, and although they are rare, hypertrophic synovial plica may be an underdiagnosed condition.10,63 In the previous edition of this text, Bennett and Melhoff postulated that two types of lateral synovial plicae exist: a plica in the lateral gutter that pops over the olecranon process; and a plica near the radiocapitellar joint that folds over the margins of the capitellum and radial head. The lateral gutter plica is particularly symptomatic in extension, whereas the radial capitellar plica causes mechanical symptoms with forearm rotation when the elbow is flexed. MRI arthrography is very helpful to make the diagnosis. Awaya et al.11 determined that synovial folds of more than 3 mm in thickness were abnormal and correlated with clinical symptoms.
Nonoperative management includes anti-inflammatory medication, physical therapy, and activity modification. Corticosteroid injection may help to decrease the synovial reaction. For those in whom nonoperative measures have failed, arthroscopy is highly successful at returning athletes to their previous level of play.10,31,63,102
REHABILITATION
Morrey and An81 defined the functional range of motion of the elbow as 30 to 130 degrees of flexion. Although most activities of daily living can be performed through this arc of motion; athletes typically have increased demands. In these cases, therapy should be attempted. However, recalcitrant cases require surgical contracture release. Arthroscopic treatment, including anterior capsule release, medial and lateral gutter débridement, and removal of excessive bone when necessary, is technically demanding but can provide excellent results.58,83,94,103
1 Adams I. Bone injuries in very young athletes. Clin. Orthop. Relat. Res. 1968;58:129.
2 Adams J. Injury to the throwing arm: a study of traumatic changes in the elbow joints of boy baseball players. Calif. Med. 1965;102:127.
3 Adler S.F.G., MacAusland W. Treatment of olecranon fracture, indications for excision of the olecranon fracture, repair of the triceps tendon. J. Trauma. 1962;2:597.
4 Ahmad C.S., ElAttrache N.S. Valgus extension overload syndrome and stress injury of the olecranon. Clin. Sports Med. 2004;23:665.
5 Ahmad C., ElAttrache N.S. Treatment of capitellar osteochondritis dissecans. Tech. Shoulder Elbow Surg. 2006;7:169.
6 Albright J.A., Jokl P., Shaw R., Albright J.P. Clinical study of baseball pitchers: correlation of injury to the throwing arm with method of delivery. Am. J. Sports Med. 1978;6:15.
7 An K.N., Morrey B.F., Chao E.Y. The effect of partial removal of proximal ulna on elbow constraint. Clin. Orthop. Relat. Res. 1986;209:270.
8 Andrews J.R., Carson W.G. Arthroscopy of the elbow. Arthroscopy. 1985;1:97.
9 Andrews J.R., Timmerman L.A. Outcome of elbow surgery in professional baseball players. Am. J. Sports Med. 1995;23:407.
10 Antuna S.A., O’Driscoll S.W. Snapping plicae associated with radiocapitellar chondromalacia. Arthroscopy. 2001;17:491.
11 Awaya H., Schweitzer M.E., Feng S.A., Kamishima T., Marone P.J., Farooki S., Trudell D.J., Haghighi P., Resnick D.L. Elbow synovial fold syndrome: MR imaging findings. A. J. R. Am. J. Roentgenol. 2001;177:1377.
12 Baker C.L.Jr, Jones G.L. Arthroscopy of the elbow. Am. J. Sports Med. 1999;27:251.
13 Barnes D.A., Tullos H.S. An analysis of 100 symptomatic baseball players. Am. J. Sports Med. 1978;6:62.
14 Bauer M., Jonsson K., Josefsson P.O., Linden B. Osteochondritis dissecans of the elbow. A long-term follow-up study. Clin. Orthop. Relat. Res. 1992;284:156.
15 Baumgarten T.E., Andrews J.R., Satterwhite Y.E. The arthroscopic classification and treatment of osteochondritis dissecans of the capitellum. Am. J. Sports Med. 1998;26:520.
16 Bennett G. Elbow and shoulder lesions of the professional baseball pitcher. J. A. M. A. 1941;117:510.
17 Bennett G. Elbow and shoulder lesions of baseball players. Am. J. Surg. 1959;98:484.
18 Bojanic I., Ivkovic A., Boric I. Arthroscopy and microfracture technique in the treatment of osteochondritis dissecans of the humeral capitellum: report of three adolescent gymnasts. Knee Surg. Sports Traumatol. Arthrosc. 2006;14:491.
19 Bowen R.E., Otsuka N.Y., Yoon S.T., Lang P. Osteochondral lesions of the capitellum in pediatric patients: role of magnetic resonance imaging. J. Pediatr. Orthop.. 2001;21:298.
20 Bradley, J., and Petrie, R.: Elbow injuries in children and adolescents. In DeLee, J. C., Drez D. and Miller, M. D. (eds.): Orthopedic Sports Medicine, 2nd ed. Philadelphia, Saunders, p. 1249.
21 Brodgon B., Crow N. Little leaguer’s elbow. A. J. R. Am. J. Roentgenol. 1960;8:671.
22 Brownlow H.C., O’Connor-Read L.M., Perko M. Arthroscopic treatment of osteochondritis dissecans of the capitellum. Knee Surg. Sports Traumatol. Arthrosc. 2006;14:198.
23 Burra G., Andrews J.R. Acute shoulder and elbow dislocations in the athlete. Orthop. Clin. North Am. 2002;33:479.
24 Byrd J.W., Elrod B.F., Jones K.S. Elbow arthroscopy for neglected osteochondritis dissecans of the capitellum. J. South. Orthop. Assoc. 2001;10:12.
25 Byrd J.W., Jones K.S. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am. J. Sports Med. 2002;30:474.
26 Cain E.L.Jr, Dugas J.R., Wolf R.S., Andrews J.R. Elbow injuries in throwing athletes: a current concepts review. Am. J. Sports Med. 2003;31:621.
27 Callaway G.F.L., Deng X.H., Torzilli P.A., O’Brien S.J., Altchek D.W., Warren R.F. Biomechanical evaluation of the medial collateral ligament of the elbow. J. Bone Joint Surg. Am. 1997;79A:1223.
28 Chappell, J., and ElAttrache, N.: Clinical outcomes of OCD lesions of the capitellum treated with osteochondral autografts. In Open Meeting American Shoulder Elbow Surgeons; 2008; San Francisco; 2008.
29 Charlton W.P., Chandler R.W. Persistence of the olecranon physis in baseball players: Results following operative management. J. Shoulder Elbow Surg. 2003;12:59.
30 Chen F.S., Rokito A.S., Jobe F.W. Medial elbow problems in the overhead-throwing athlete. J. Am. Acad. Orthop. Surg. 2001;9:993.
31 Clarke R.P. Symptomatic, lateral synovial fringe (plica) of the elbow joint. Arthroscopy. 1988;4:112.
32 Conn J., Wade P. Injuries of the elbow: ten-year review. J. Trauma. 1961;1:248.
33 Danielsson L.G., Hedlund S.T., Henricson A.S. Apophysitis of the olecranon. A report of four cases. Acta Orthop. Scand. 1983;54:777.
34 David T.S. Medial elbow pain in the throwing athlete. Orthopedics. 2003;26:94. quiz 104
35 Dehaven K.E., Ferguson A., Hale C.J., Larson R., Tullos H. Symposium: Throwing injuries to the adolescent elbow. Contemp. Surg. 1976;9:65.
36 Dehaven K., Evartsm C. Throwing injuries of the elbow in athletes. Orthop. Clin. North Am. 1973;1:801.
37 Dunn N. Operation for fracture of the olecranon. B. M. J. 1939;1:214.
38 Fleisig G.S., Barrentine S.W., Escamilla R.F., Andrews J.R. Biomechanics of overhand throwing with implications for injuries. Sports Med. 1996;21:421.
39 Fleisig G.S., Barrentine S.W., Zheng N., Escamilla R.F., Andrews J.R. Kinematic and kinetic comparison of baseball pitching among various levels of development. J. Biomech. 1999;32:1371.
40 Gainor B., Piotrowski G., Puhl J., Allen W.C., Hagen R. The throw: biomechanics and acute injury. Am. J. Sports Med. 1980;8:114.
41 Gartsman G., Sculco T., Otis J. Operative treatment of olecranon fractures: excision or open reduction with internal fixation. J. Bone Joint Surg. Am. 1981;63A:718.
42 Gerbino P.G., Waters P. Elbow injuries in the young athlete. Op. Tech. Sports Med. 1998;6:259.
43 Gicquel P., Maximin M.C., Boutemy P., Karger C., Kempf J.F., Clavert J.M. Biomechanical analysis of olecranon fracture fixation in children. J. Pediatr. Orthop. 2002;22:17.
44 Gore R., Rogers L., Bowerman J., Suker J., Conpere C. Osseous manifestations of elbow stress associated with sports pitchers. A. J. R. Am. J. Roentgenol. 1980;134:971.
45 Gudmundsen T., Ostensen H. Accessory ossicles in the elbow. Acta Orthop. Scand. 1987;58:130.
46 Guggenheim J., Stanley R., Woods G.W., Tullos H.S. Little League survey: The Houston Study. Am. J. Sports Med. 1976;4:189.
47 Hang V., Lippert G., Spolek G., Frankel V., Harrington R. Biomechanical study of the pitching elbow. Int. Orthop. 1979;3:217.
48 Hang D.W., Chao C.M., Hang Y.S. A clinical and roentgenographic study of Little League elbow. Am. J. Sports Med. 2004;32:79.
49 Harada M., Ogino T., Takahara M., Ishigaki D., Kashiwa H., Kanauchi Y. Fragment fixation with a bone graft and dynamic staples for osteochondritis dissecans of the humeral capitellum. J. Shoulder Elbow Surg. 2002;11:368.
50 Harada M., Takahara M., Sasaki I. Using sonography for the early detection of elbow injuries among young baseball players. A. J. R. Am. J. Roentgenol. 2006;187:1436.
51 Hepler M., Steinmann S., Rosenwasser M. Elbow arthroscopy in the treatment of posterior olecranon impingement. Arthroscopy. 1998;14:430.
52 Inoue G., Kuwahata Y. Surgical repair of traumatic medial disruption of the elbow in competitive athletes. Br. J. Sports Med. 1995;29:139.
53 Ireland M.L., Andrews J.R. Shoulder and elbow injuries in the young athlete. Clin. Sports Med. 1988;7:473.
54 Ireland M.L., Hutchinson M.R. Upper extremity injuries in young athletes. Clin. Sports Med. 1995;14:533.
55 Iwasaki N., Kato H., Ishikawa J., Saitoh S., Minami A. Autologous osteochondral mosaicplasty for capitellar ostechondritis dissecans in teenaged patients. Am. J. Sports Med. 2006;34:1233.
56 Jackson D.W., Silvino N., Reiman P. Osteochondritis in the female gymnast’s elbow. Arthroscopy. 1989;5:129.
57 Jobe F.W., Stark H., Lombardo S.J. Reconstruction of the ulnar collateral ligament in athletes. J. Bone Joint Surg. Am. 1986;68:1158.
58 Jones G.S., Savoie F.H.3rd. Arthroscopic capsular release of flexion contractures (arthrofibrosis) of the elbow. Arthroscopy. 1993;9:277.
59 Josefsson P.O., Danielsson L.G. Epicondylar elbow fracture in children. 35-year follow-up of 56 unreduced cases. Acta Orthop. Scand. 1986;57:313.
60 Josefsson P.O., Johnell O., Gentz C.F. Long-term sequelae of simple dislocation of the elbow. J. Bone Joint Surg. 1984;66A:927.
61 Kamineni S., ElAttrache N.S., O’Driscoll S.W., Ahmad C.S., Hirohara H., Neale P.G., An K.N., Morrey B.F. Medial collateral ligament strain with partial posteromedial olecranon resection. A biome-chanical study. J. Bone Joint Surg. Am. 2004;86-A:2424.
62 Kamineni S., Hirahara H., Pomianowski S., Neale P.G., O’Driscoll S.W., ElAttrache N., An K.N., Morrey B.F. Partial posteromedial olecranon resection: a kinematic study. J. Bone Joint Surg. Am. 2003;85-A:1005.
63 Kim D.H., Gambardella R.A., Elattrache N.S., Yocum L.A., Jobe F.W. Arthroscopic treatment of posterolateral elbow impingement from lateral synovial plicae in throwing athletes and golfers. Am. J. Sports Med. 2006;34:438.
64 King J., Brelsford H., Tullos H.S. Analysis of the pitching arm of the professional pitcher. Clin. Orthop. Relat. Res. 1969;67:116.
65 Kiyoshige Y., Takagi M., Yuasa K., Hamasaki M. Closed-wedge osteotomy for osteochondritis dissecans of the capitellum. A 7- to 12-year follow-up. Am. J. Sports Med. 2000;28:534.
66 Kobayashi K., Burton K.J., Rodner C., Smith B., Caputo A.E. Lateral compression injuries in the pediatric elbow: Panner’s disease and osteochondritis dissecans of the capitellum. J. Am. Acad. Orthop. Surg. 2004;12:246.
67 Kondo M., Asoh K. The treatment of osteochondritis dissecans of the elbow: Pull out wiring method. Jap. Joint Surg. 1992;11:630.
68 Kovach J.2nd, Baker B.E., Mosher J.F. Fracture separation of the olecranon ossification center in adults. Am. J. Sports Med. 1985;13:105.
69 Krijnen M.R., Lim L., Willems W.J. Arthroscopic treatment of osteochondritis dissecans of the capitellum: Report of 5 female athletes. Arthroscopy. 2003;19:210.
70 Kuwahata Y., Inoue G. Osteochondritis dissecans of the elbow managed by Herbert screw fixation. Orthopedics. 1998;21:449.
71 Larson R.L., McMahan R. The epiphysis and the childhood athlete. J. A. M. A. 1966;196:607.
72 Lokiec F., Velkes S., Engel J. Avulsion of the medial epicondyle of the humerus in arm wrestlers: a report of five cases and a review of the literature. Injury. 1991;22:69.
73 Lowery W.D.Jr, Kurzweil P.R., Forman S.K., Morrison D.S. Persistence of the olecranon physis: a cause of “little league elbow.”. J. Shoulder Elbow Surg.. 1995;4:143.
74 Maffulli N., Chan D., Aldridge M.J. Overuse injuries of the olecranon in young gymnasts. J. Bone Joint Surg. Br. 1992;74:305.
75 McManama G.B.Jr, Micheli L.J., Berry M.V., Sohn R.S. The surgical treatment of osteochondritis of the capitellum. Am. J. Sports Med. 1985;13:11.
76 Micheli L.J. The traction apophysitises. Clin. Sports Med. 1987;6:389.
77 Miller J. Javelin thrower’s elbow. J. Bone Joint Surg. 1960;42B:788.
78 Mitsunaga M.M., Adishian D.A., Bianco A.J.Jr. Osteochondritis dissecans of the capitellum. J. Trauma. 1982;22:53.
79 Morrey B.F. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr. Course Lect. 1995;44:175.
80 Morrey B., An K. Functional anatomy of the ligaments of the elbow. Clin. Orthop. Relat. Res. 1985;201:84.
81 Morrey B.F., An K.N. Articular and ligamentous contributions to the stability of the elbow joint. Am. J. Sports Med. 1983;11:315.
82 Nuber G.W., Diment M.T. Olecranon stress fractures in throwers. A report of two cases and a review of the literature. Clin. Orthop. Relat. Res. 1992;278:58.
83 Nguyen D., Proper S.I., MacDermid J.C., King G.J., Faber K.J. Functional outcomes of arthroscopic capsular release of the elbow. Arthroscopy. 2006;22:842.
84 Nyska M., Peiser J., Lukiec F., Katz T., Liberman N. Avulsion fracture of the medial epicondyle caused by arm wrestling. Am. J. Sports Med. 1992;20:347.
85 Ogata S., Uhthoff H.K. The development of synovial plicae in human knee joints: an embryologic study. Arthroscopy. 1990;6:315.
86 O’Holleran J.D., Altchek D.W. Elbow arthroscopy: treatment of the thrower’s elbow. Instr. Course Lect. 2006;55:95.
87 Orava S., Hulkko A. Delayed unions and nonunions of stress fractures in athletes. Am. J. Sports Med. 1988;16:378.
88 Panner H. A peculiar affection of the capitulum humeri resembling Calve-Perthes disease of the hip. Acta Radiol. 1928;10:234.
89 Pappas A.M. Osteochondrosis dissecans. Clin. Orthop. Relat. Res. 1981;158:59.
90 Pappas A.M. Elbow problems associated with baseball during childhood and adolescence. Clin. Orthop. Relat. Res. 1982;164:30.
91 Pavlov H., Torg J.S., Jacobs B., Vigorita V. Nonunion of olecranon epiphysis: two cases in adolescent baseball pitchers. A. J. R. Am. J. Roentgenol. 1981;136:819.
92 Peterson R.K., Savoie F.H.3rd, Field L.D. Osteochondritis dissecans of the elbow. Instr. Course Lect. 1999;48:393.
93 Petty D.H., Andrews J.R., Fleisig G.S., Cain E.L. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am. J. Sports Med. 2004;32:1158.
94 Phillips B.B., Strasburger S. Arthroscopic treatment of arthrofibrosis of the elbow joint. Arthroscopy. 1998;14:38.
95 Rao P.S., Rao S.K., Navadgi B.C. Olecranon stress fracture in a weight lifter: a case report. Br. J. Sports Med. 2001;35:72.
96 Reddy A.S., Kvitne R.S., Yocum L.A., Elattrache N.S., Glousman R.E., Jobe F.W. Arthroscopy of the elbow: a long-term clinical review. Arthroscopy. 2000;16:588.
97 Regan W.D., Korinek S.L., Morrey B.F., An K.N. Biomechanical study of ligaments around the elbow joint. Clin. Orthop. Relat. Res. 1991;271:170.
98 Rettig A.C., Wurth T.R., Mielingm P. Nonunion of olecranon stress fractures in adolescent baseball pitchers: a case series of 5 athletes. Am. J. Sports Med. 2006;34:653.
99 Roberts P. Dislocations of the elbow. Lancet. 1934;2:78.
100 Rolla P.R., Surace M.F., Bini A., Pilato G. Arthroscopic treatment of fractures of the radial head. Arthroscopy. 2006;22:233 e1.
101 Ruch D.S., Poehling G.G. Arthroscopic treatment of Panner’s disease. Clin. Sports Med. 1991;10:629.
102 Ruch D.S., Papadonikolakis A., Campolattaro R.M. The posterolateral plica: a cause of refractory lateral elbow pain. J. Shoulder Elbow Surg. 2006;15:367.
103 Savoie F.H.3rd, Field L.D. Arthrofibrosis and complications in arthroscopy of the elbow. Clin. Sports Med. 2001;20:123. ix
104 Schenk M., Dalinka M.K. Imaging of the elbow. An update. Orthop. Clin. North Am. 1997;28:517.
105 Schwab G.H., Bennett J.B., Woods G.W., Tullos H.S. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin. Orthop. Relat. Res. 1980;146:42.
106 Singer K., O’Neill D. Update of elbow injuries in the young athlete. In: Grana W.B., editor. Advances in Sports Medicine. Chicago: Year Book Medical Publishers; 1990:147.
107 Slocum D. Classification of elbow injuries from baseball pitching. Texas Med. 1968;64:48.
108 Sneed J., Boyd H. Fractures about the elbow. Am. J. Surg. 1937;38:727.
109 Suzuki K., Minami A., Suenaga N., Kondoh M. Oblique stress fracture of the olecranon in baseball pitchers. J. Shoulder Elbow Surg. 1997;6:491.
110 Takahara M., Shundo M., Kondo M., Suzuki K., Nambu T., Ogino T. Early detection of osteochondritis dissecans of the capitellum in young baseball players. Report of three cases. J. Bone Joint Surg. Am. 1998;80:892.
111 Takahara M., Ogino T., Fukushima S., Tsuchida H., Kaneda K. Nonoperative treatment of osteochondritis dissecans of the humeral capitellum. Am. J Sports Med. 1999;27:728.
112 Takahara M., Ogino T., Sasaki I., Kato H., Minami A., Kaneda K. Long term outcome of osteochondritis dissecans of the humeral capitellum. Clin. Orthop. Relat. Res. 1999;363:108.
113 Takeda H., Watarai K., Matsushita T., Saito T., Terashima Y. A surgical treatment for unstable osteochondritis dissecans lesions of the humeral capitellum in adolescent baseball players. Am. J. Sports Med. 2002;30:713.
114 Thomson N. Osteochondritis dissecans and osteochondral fragments managed by herbert compression screw fixation. Clin. Orthop. Rel. Res. 1987;224:71.
115 Tivnon M., Anzel S., Waugh T. Surgical management of osteochondritis dissecans of the capitellum. Am. J. Sports Med. 1976;4:121.
116 Torg J.S., Moyer R.A. Non-union of a stress fracture through the olecranon epiphyseal plate observed in an adolescent baseball pitcher. A case report. J. Bone Joint Surg. Am. 1977;59:264.
117 Tullos H.S., Erwin W., Woods G.W. Unusual lesions of the pitching arm. Clin. Orthop. Relat. Res. 1972;88:169.
118 Tullos H.S., King J. Lesions of the pitching arm in adolescents. J. A. M. A. 1972;220:264.
119 Wadsworth T. The Elbow. Edinburgh: Churchill Livingstone, 1982.
120 Warwick R., Williams P. Gray’s Anatomy, 35th ed. Philadelphia: WB Saunders Co., 1973.
121 Wilkerson R.D., Johns J.C. Nonunion of an olecranon stress fracture in an adolescent gymnast. A case report. Am. J. Sports Med. 1990;18:432.
122 Wilson F.D., Andrews J.R., Blackburn T.A., McCluskey G. Valgus extension overload in the pitching elbow. Am. J. Sports Med. 1983;11:83.
123 Woods G.W., Tullos H.S., King J.W. The throwing arm: elbow joint injuries. J. Sports Med. 1973;1:43.
124 Woodward A., Bianco A.J. Osteochondritis dissecans of the elbow. Clin. Orthop. Relat. Res. 1975;110:35.
125 Yamamoto Y., Ishibashi Y., Tsuda E., Sato H., Toh S. Osteochondral autograft transplantation for osteochondritis dissecans of the elbow in juvenile baseball players: minimum 2-year follow-up. Am. J. Sports Med. 2006;34:714.