Chapter 47  Articular Cartilage Rating Systems
Articular Cartilage Rating Systems
INTRODUCTION
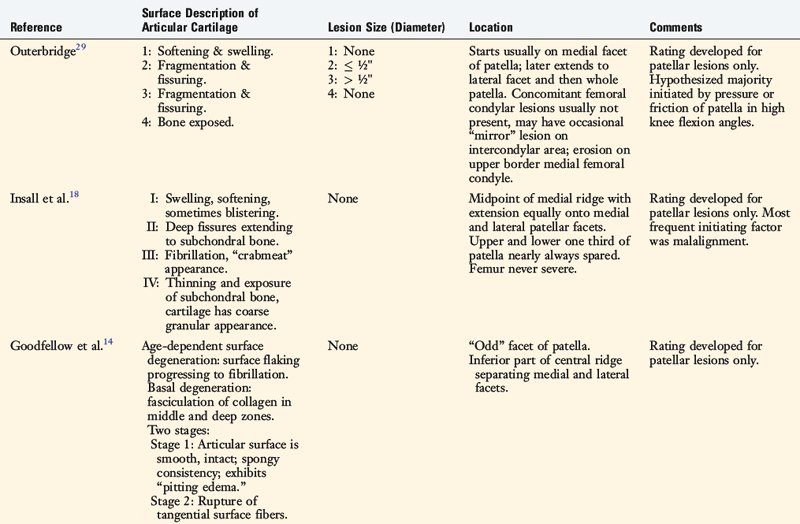
Many systems have been proposed to classify lesions of the articular cartilage in the knee joint (Table 47-1). The cartilage systems published in the 1960s and 1970s introduced grading schemes for lesions located only in the patellofemoral joint and documented the most frequent locations of damage in this compartment.13,14,18,29 The first of these patellofemoral classification systems, proposed by Outerbridge,29 remains one of the most commonly used schemes to grade lesions located in all three compartments of the knee (patellofemoral, medial tibiofemoral, and lateral tibiofemoral).10 As arthroscopy and imaging techniques have evolved, a few investigators 17,28 and societies (International Cartilage Repair Society [ICRS], French Society of Arthroscopy [SFA]) have proposed articular cartilage rating systems that are far greater in sophistication in classifying lesions, as is described later. These systems are useful for formal clinical investigations to determine the etiology and prognosis of partial and full-thickness cartilage injuries after various knee injuries22 and to determine the indications and outcomes of cartilage resurfacing procedures including mosaicplasty and autologous chondrocyte implantation (ACI).6
REVIEW OF PUBLISHED ARTICULAR CARTILAGE RATING SYSTEMS
Outerbridge
In 1961, Outerbridge29 introduced a system for grading articular cartilage lesions in the patellofemoral joint. The four-gradient scale was based on the appearance of the cartilage and, in two of the levels, the size of the lesion. A grade 1 lesion was defined as softening and swelling of the cartilage. A grade 2 lesion involved fissuring and fragmentation in an area less than ½” in diameter. A grade 3 lesion involved fissuring and fragmentation in an area greater than ½” in diameter. In a grade 4 lesion, the cartilage was eroded down to subchondral bone. This rating system did not specify the location, depth, or exact size of the lesion.
Insall
Insall and coworkers18 proposed a classification system for patellofemoral articular cartilage lesions that was composed of four stages based on the cartilage appearance. The first stage consisted of swelling, softening, and blistering of the cartilage. The second stage included lesions with deep fissures that extended to subchondral bone. The third stage involved fibrillation and a “crabmeat” appearance. In the fourth stage, thinning of the cartilage and exposure of subchondral bone in some areas were noted, with the remainder of the cartilage demonstrating a “coarse granular appearance.” This rating system also failed to specify the location, depth, and size of the lesion.
Critical Points REVIEW OF PUBLISHED ARTICULAR CARTILAGE RATING SYSTEMS
Cincinnati Knee Rating System
SFA System (French Society of Arthroscopy)
International Cartilage Repair Society
Hunt
Goodfellow
Goodfellow and associates15 described two different types of disorders of articular cartilage in the patellofemoral compartment: age-dependent surface degeneration and basal degeneration. Age-dependent surface degeneration was usually found on the odd facet, was often present in middle-aged patients, and became even more frequent with increasing age. These lesions involved surface flaking that progressed to fibrillation and, finally, subchondral bone exposure. The authors believed these lesions were asymptomatic in younger patients, but could become painful as degenerative joint disease in later years.
Casscells
Casscells8 used a rating system to describe lesions located on the undersurface of the patella and femoral condyles in an anatomic cadaveric investigation. The five-level gradient classification included both cartilage appearance and size of the lesion. Grade 0 indicated normal surfaces with no gross lesions present. Grade 1 included small, superficial areas of cartilage erosion, 1 cm or less in diameter. Grade 2 lesions were 1 to 2 cm in diameter and involved the “deeper layers” of cartilage. Grade 3 indicated lesions that were 2 to 4 cm in diameter in which the cartilage was completely eroded and subchondral bone was exposed. Grade 4 designated cartilage that was “completely destroyed,” often involving complete loss of the entire articular surface.
Ficat and Hungerford
Ficat and Hungerford12 described a two-stage classification system for lesions in the patellofemoral compartment based on the appearance of the cartilage. Stage one was described as closed chondromalacia in which the surface was intact but the degree of severity varied from simple softening to “pitting edema” and loss of elasticity. Stage two was defined as open chondromalacia. This stage was subdivided into two groups: A, single or multiple fissures that were either relatively superficial or extended down to subchondral bone; and B, ulceration or localized loss of cartilage substance, exposed dense subchondral bone that represented the final stage of cartilage destruction.
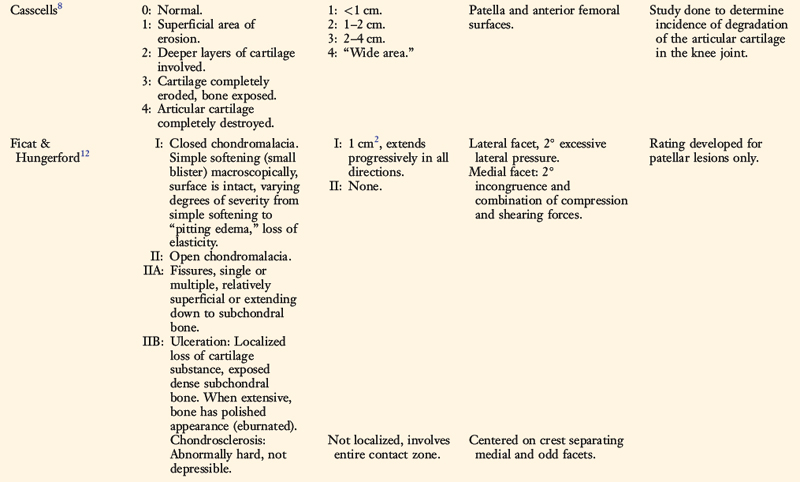
Cincinnati Knee Rating System
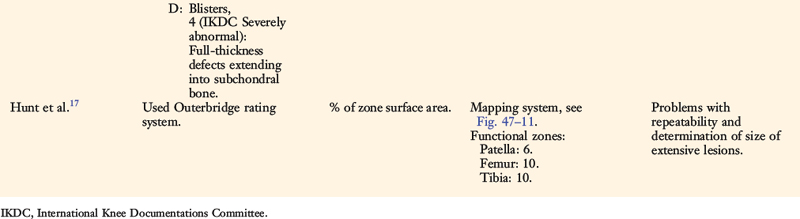
In 1989, Noyes and Stabler28 proposed a new articular cartilage classification system that included four variables: the appearance of the cartilage (as visualized arthroscopically), the depth of the lesion, the size (diameter) of the lesion, and the location of the lesion. A point scaling system was devised for research purposes to facilitate statistical analyses (Table 47-2).
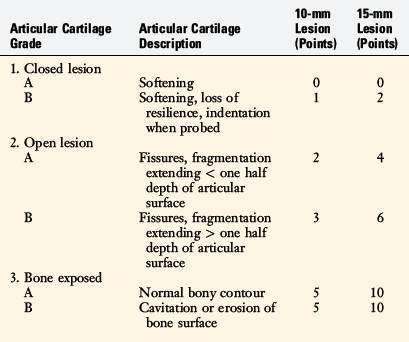
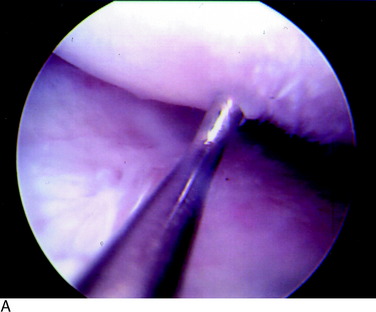
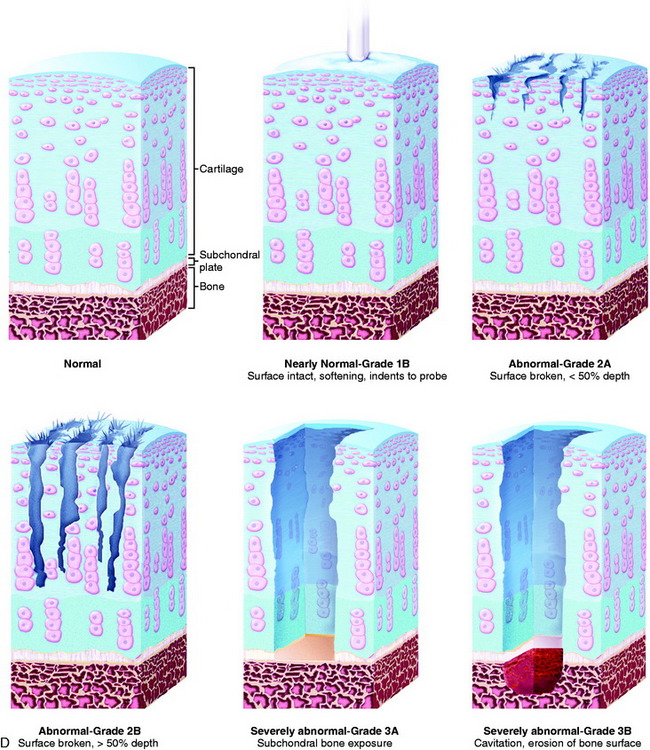
Grade 1A corresponds to a moderate degree of softening of the cartilage compared with its normal resilient appearance (Fig. 47-1A). Grade 1B designates complete loss of resilience, resulting in full indentation of the surface when probed (see Fig. 47-1B). This grade is reserved for lesions in which a severe softening of the cartilage exists without gross surface breakage. This description indicates the initial stage of cartilage deterioration characterized by diminished glycoproteins and early collagen fiber deterioration.28 These lesions, which commonly involve the undersurface of the patella, have a high potential to progress to an open lesion.
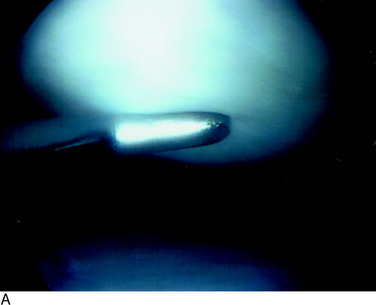
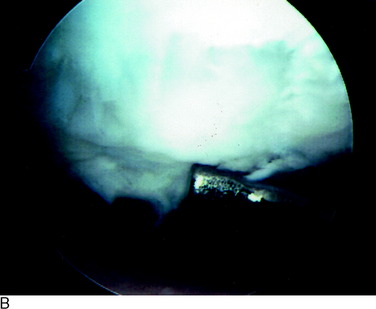
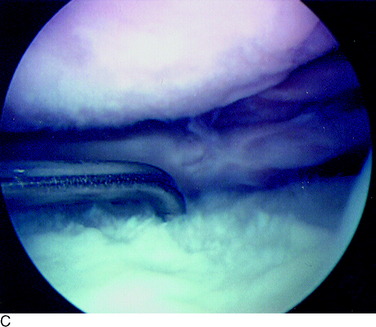
A grade 2A lesion (Fig. 47-2A) is an open disruption of the cartilage surface, including cracks, surface blisters, fissures, fibrillations, and fragmentations that extend less than one half of the thickness of the cartilage. Grade 2B lesions (see Fig. 47-2B and C) are similar in appearance, but extend greater than one half of the thickness of the cartilage. Superficial lesions with fibrillation-type changes are usually easily distinguishable from deeper lesions that involve lacerations, clefts, and fragmentation down to bone. Chondrosclerosis is classified as a grade 2 lesion, because the surface is abnormal. Lesions that have two or three deep lacerations that extend through the cartilage surrounded by otherwise normally appearing cartilage are graded as 2B.
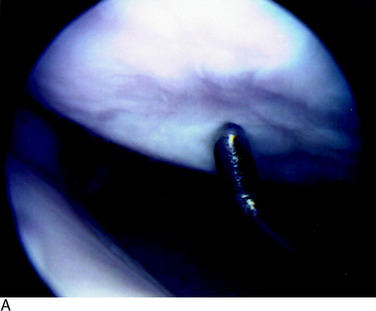
A grade 3A lesion (Fig. 47-3A) indicates a surface with exposed bone in which the normal bony contour remains. The most severe lesion, grade 3B (Fig. 47-3B and C), indicates cavitation or erosion of the bone surface. An example of a grade 3B lesion is an osteochondritis dissecans lesion in which there is loss of the subchondral bone. Other examples are lesions in which grooving of the bony surface is visualized or those involving fractures that extend through the subchondral bone.
The size of all lesions is determined using a calibrated nerve hook probe. The size is recorded according to one of five categories ranging from less than 10 mm to greater than 25 mm (see Table 47-1). A schematic illustration of all grades is shown in Figure 47-3D.
Figure 47-4A illustrates how this classification system is used to record the visual appearance of articular cartilage lesions. The patella has a 10-mm grade 2A lesion that is surrounded by a larger closed area of softening (1B) that extends 20 mm in diameter. The trochlea has a large area of extensive softening as well, graded as a 1B that is 25 mm in diameter. The medial femoral condyle also has a large area of extensive softening, measuring 15 mm in diameter. A “kissing” lesion is found on the medial tibial plateau of a grade 2A lesion that is 10 mm in diameter. The lateral femoral condyle has a complex lesion; 10 mm of exposed bone (3A) is surrounded by an open lesion of fragmentation of 20 mm in diameter (2B), which is in turn surrounded by a closed lesion of soft cartilage that extends to 25 mm (1B). The lateral tibial plateau has a large 2B lesion, 15 mm in diameter. For research purposes, the lesions may be quantified on a scaling system to allow statistical analysis (see Table 47-2). Any lesion that is less than 10 mm in diameter, or graded 1A, is not considered clinically significant and, therefore, no points are given. Figure 47-4B illustrates the points awarded for the lesions noted in the example.
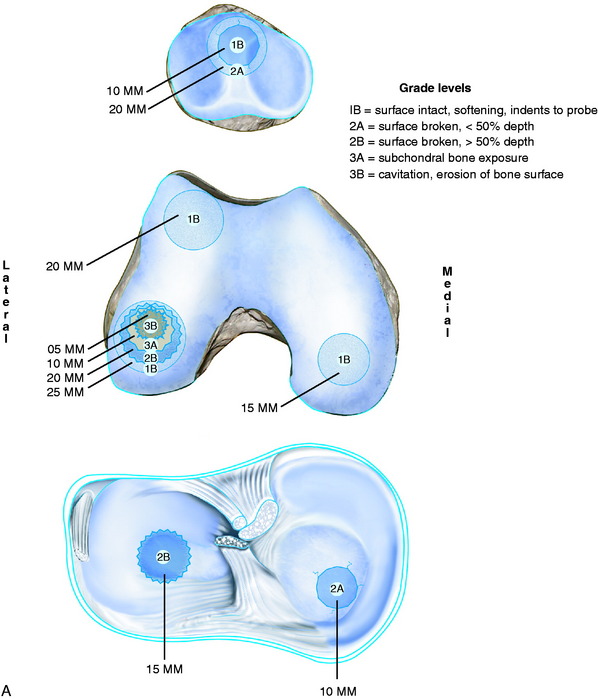
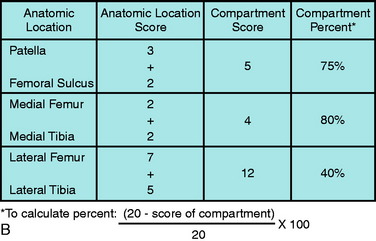
FIGURE 47-4 A, An example of the grading of articular cartilage lesions found at arthroscopy. B, Scoring system for articular cartilage lesions (see Table 47-2).
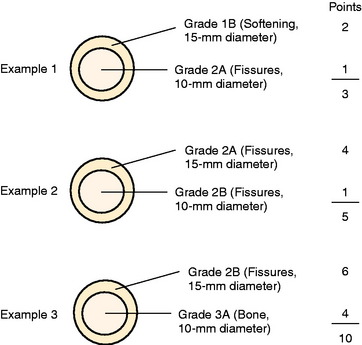
Occasionally, complex lesions are encountered such as a 2A circumferential fibrillation surrounding a 10-mm 2B lesion. For scoring purposes, additional points for complex lesions may be incorporated so that the total points to be subtracted are increased, but still less than the corresponding 15 mm lesion. Examples for scoring complex lesions are shown in Figure 47-5.
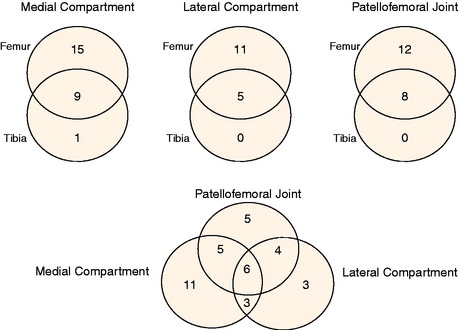
This classification system allows clinical investigations to analyze results according to the condition of the articular cartilage and to determine the difference in outcome between patients with normal cartilage, noteworthy cartilage damage (grade 2B), and severe cartilage damage (grade 3).24–27 For instance, in a study of 66 patients who had an anterior cruciate ligament (ACL) revision reconstruction,27 the authors found that patients with grades 2B or 3A lesions had significantly poorer subjective and functional outcomes a mean of 42 months postoperatively compared with those with normal or grade 1 surfaces (Table 47-3). The factors included pain (P = .03), stair-climbing (P = .01), kneeling (P = .01), running (P = .001), jumping (P = .01), twisting and turning (P = .01), and the overall Cincinnati Knee Rating Score (CKRS; P = .0001). Analysis of the preoperative data found significant differences between these subgroups as well for giving-way (P = .004), walking (P = .04), stair-climbing (P = .04), kneeling (P = .01), running (P = .004), jumping (P = .001), twisting and turning (P = .01), and the overall CKRS (P = .0001). Differences were also noted in the sports activity levels patients resumed postoperatively (Table 47-4). The stratification of lesions according to the six compartments may be presented as shown in Figure 47-6. These findings allow appropriate patient counseling regarding the expected outcome of the operation according to, among other factors, the condition of the articular cartilage. Larger sample sizes would allow further analysis of the effect of not only the grade of lesions but their locations as well.
TABLE 47-3 Effect of the Condition of the Articular Cartilage at the Index Operation on the Subjective Scores and Overall Rating at the Latest Follow-up Examination after Anterior Cruciate Ligament Revision Reconstruction
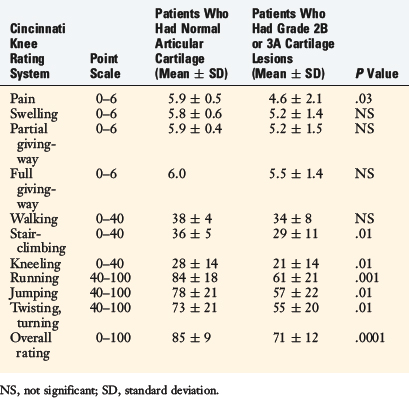
TABLE 47-4 Effect of the Condition of the Articular Cartilage at the Index Operation on the Sports Activity Level at the Latest Follow-up Examination after Anterior Cruciate Ligament Revision Reconstruction
| Type of Sports Activity | Patients Who Had Normal Articular Cartilage (N = 28) | Patients Who Had Grade 2B or 3A Cartilage Lesions (N = 37) |
|---|---|---|
| Jumping, pivoting, cutting | 8 (29%) | 3 (8%) |
| Running, twisting, turning | 7 (25%) | 6 (16%) |
| Swimming, bicycling | 9 (32%) | 18 (49%) |
| No sports | 4 (14%) | 10 (27%) |
SFA System
Dougados and colleagues11 described a rating system for assessing the severity of articular cartilage lesions by determining the location, size, and appearance of the lesions. The location of the lesions was drawn on a diagram for the patella, trochlea, medial femur, medial tibia, lateral femur, and lateral tibia. The size of the lesion was recorded in terms of percentage of the joint surface affected. The appearance was graded according to a system proposed by Beguin and Locker2 in which grade I represents closed lesions; grade II, superficial fissuring; grade III, deep fissuring, reaching subchondral bone that is not visualized but may be probed; and grade IV, subchondral bone exposure.
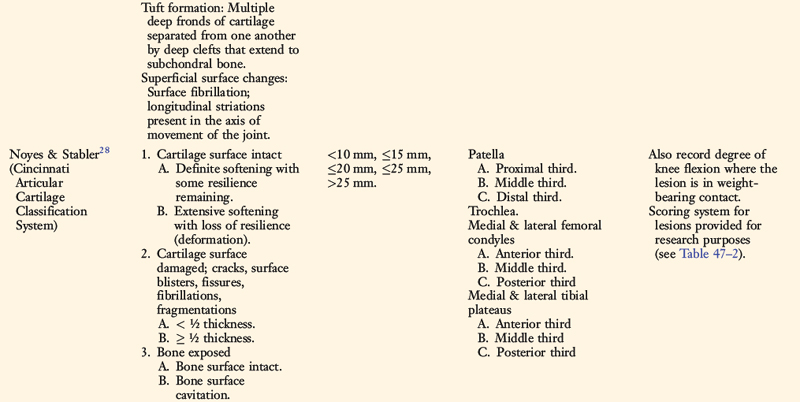
ICRS
The ICRS was founded in 1997 to develop a standardized system for the evaluation of articular cartilage injury and repair.4,5 The system focuses on the depth of lesions (graded from 0–4; see Table 47-1), the size of the lesion (recorded in millimeters), and the area of damage (documented on a mapping system; Fig. 47-7). The results are also recorded as either normal, nearly normal, abnormal, or severely abnormal for use with the International Knee Documentation Committee (IKDC) knee rating system.16
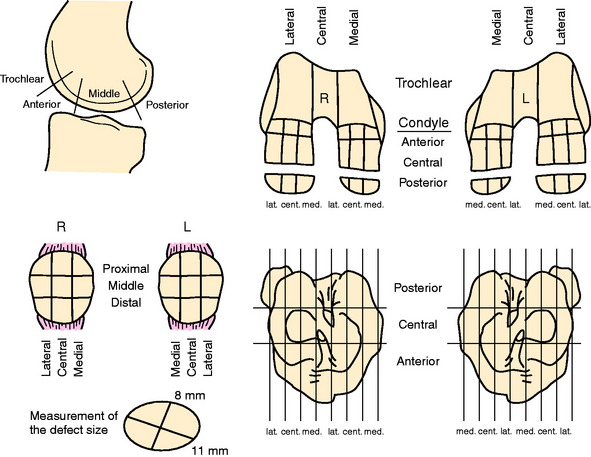
FIGURE 47-7 International Cartilage Repair Society knee cartilage mapping system.
(Document reprinted with permission from the International Cartilage Repair Society, Switzerland.)
Normal cartilage is graded as ICRS 0, or normal on the IKDC system (see Chapter 45, The International Knee Documentation Committee Rating System). Intact lesions with slight softening or mild fibrillation are classified as ICRS 1A and, if additional superficial lacerations and fissures are present, are classified as ICRS 1B (nearly normal on the IKDC system for both ICRS 1A and 1B). Lesions that extend deeper than 1B defects that involve less than 50% of the cartilage thickness are classified as ICRS 2, or abnormal on the IKDC system.
The ICRS mapping system requires validation because it contains 46 zones that have minimal anatomic and functional referencing.17 Brittberg and Winalski6 expressed that “If the total joint involvement can be assessed with percentages and/or with such a scoring system, perhaps with the aid of a computer-based system, the progression or improvement of cartilage disease can be followed.”6
The ICRS proposed a rating for the assessment of cartilage resurfacing procedures such as mosaicplasty, osteochondral autograft transfer, and ACI. The assessment includes consideration of the volume of the defect that is filled with repair tissue, the integration of repair tissue with surrounding articular cartilage, and the macroscopic surface appearance (Table 47-5). A grading system is incorporated that allows both statistical analysis of the total points obtained (scale, 1–12 points) and placement of patients into IKDC overall rating categories.
TABLE 47-5 International Cartilage Repair Society Cartilage Repair Assessment
| Criteria | Findings | Points |
|---|---|---|
From Brittberg, M.; Winalski, C. S.: Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85(suppl 2):58–69, 2003.
| Overall Repair Assessment: | Grade I (Normal) | 12 points |
| Grade II (Nearly normal) | 8–11 points | |
| Grade III (Abnormal) | 4–7 points | |
| Grade IV (Severely abnormal) | 1–3 points |
ACI, autologous chondrocyte implantation; OAT, osteochondral autograft transplantation.
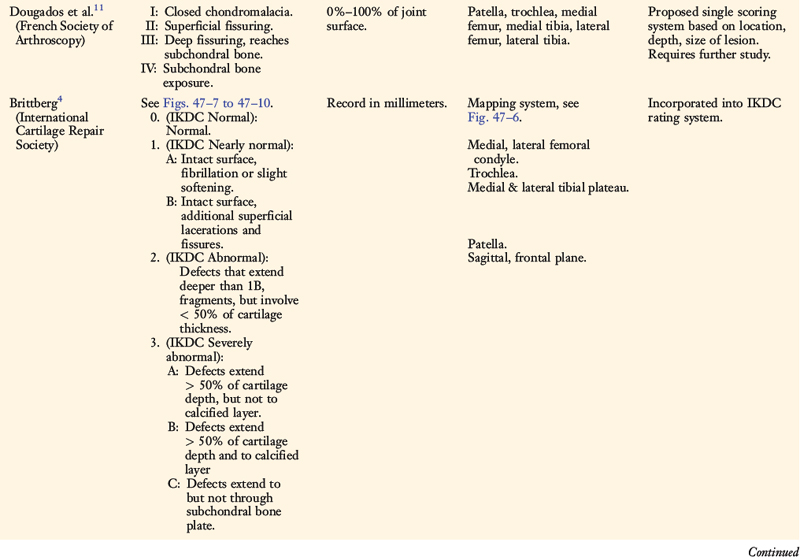
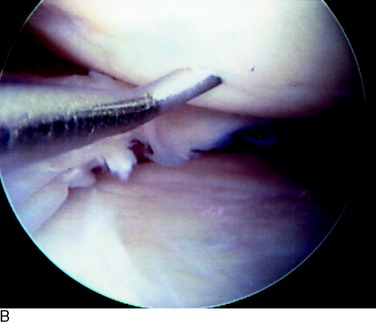
Hunt
Hunt and coworkers17 devised a rating system for chondral lesions of the knee that assessed location, size, and appearance of the cartilage. These authors devised anatomic articular maps that were divided into zones (Fig. 47-8) according to weight-bearing function and contact with other structures. Ten zones were determined on the femur by tibiofemoral weight-bearing function and flexion horizons. Ten zones were mapped on the tibia in relation to the menisci. Six zones were determined on the patella according to proximal-distal location and the median ridge. The size of lesions was measured with a graduated probe at arthroscopy and converted to a percentage of each articular surface. Outerbridge grades were used to rate the appearance of the lesions.
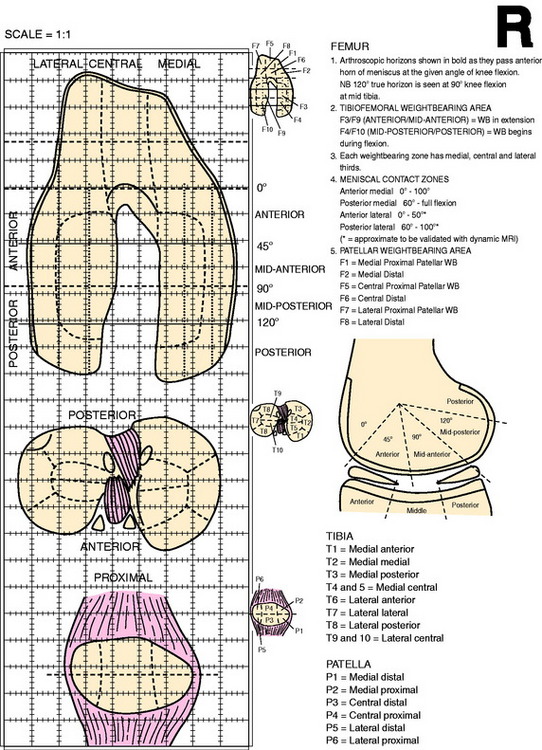
FIGURE 47-8 Articular maps of femur, tibia, and patella.
(From Hunt, N.; Sanchez-Ballester, J.; Pandit, R.; et al.: Chondral lesions of the knee: a new localization method and correlation with associated pathology. Arthroscopy 17:481–490, 2001.)
Data were collected from 1000 consecutive arthroscopies in which 1553 chondral lesions were noted. The majority of patients (85%) had concomitant joint pathology including meniscus tears, ligament ruptures, synovial lesions, and patellofemoral malalignment. The most commonly affected regions of articular damage were the main weight-bearing areas of the medial and lateral femur that were in contact with the tibial plateau and menisci in extension (see F3 in Fig. 47-8). Frequency distribution of the zones affected according to diagnosis showed marked differences between patients with complete ACL ruptures, meniscus tears, and symptomatic synovial plicas. For instance, patients with ACL ruptures had an increase in the incidence of lesions on the lateral tibiofemoral compartment, and a decrease in the incidence of lesions in the patellofemoral compartment, compared with patients with other diagnoses.
INVESTIGATIONS BY INDEPENDENT INSTITUTIONS
Reliability Studies of Cartilage Rating Systems
Only a select number of intraobserver and interobserver reliability studies of various articular cartilage rating systems have been conducted to date.3,7,22,23 Brismar and associates3 measured intraobserver and interobserver reliability among four orthopaedic surgeons who rated lesions according to Outerbridge, SFA, and a modified Collins9 classification system. Videotapes of 19 knees with a total of 114 surfaces were rated by each surgeon during two separate sessions that were at least 2 months apart. The authors reported that the coefficient kappa statistic (measurement of agreement beyond that expected by chance alone) demonstrated only moderate intraobserver and interobserver agreements. Disagreement was evident both between and within observers in the rating of lesions; however, only 6% to 8% of the paired intraobserver classifications differed by more than one grade or category within each rating system. The investigators concluded that, for research purposes, an improved classification system was required.
Cameron and colleagues7 investigated six cadaveric knees aged 50 to 79 years in which first standard arthroscopy was performed and then arthrotomy and measurement of lesions was accomplished using calipers to assign the appropriate grade according to the Outerbridge classification system. A total of nine orthopaedic surgeons reviewed each videotape twice during the same session and graded any lesions viewed.
Critical Points INVESTIGATIONS BY INDEPENDENT INSTITUTIONS
Reliability Studies of Cartilage Rating Systems
Correlation of ICRS Rating and Changes in Tissue Mechanical Properties
Sensitivity and Specificity of Standing Radiographs to Detect Mild Osteoarthritis
accurately grade chondral lesions” with the Outerbridge classification system. The number of years of orthopaedic experience did not significantly influence the study findings.
Marx and coworkers22 measured the interobserver variability in the grading of articular cartilage lesions using the Outerbridge system as observed on surgical videotapes. Six surgeons provided grades for each articular surface in 53 knees. In the first 31 knees, grades 2 and 3 were combined, whereas in the remaining 22 knees, these grades were not combined. Multirater kappa statistics demonstrated high interrater agreement for all joint surfaces except the medial and lateral tibial plateau when grades 2 and 3 were combined. However, in the knees in which grades were not combined, only moderate interrater agreement was reported.
Smith and associates30 tested the validity and reliability of the ICRS system and the previously unpublished Oswestry Arthroscopy Score (OAS), as used to rate repair of articular cartilage using procedures such as osteochondral autograft transfer and ACI. The OAS score rates five macroscopic parameters of graft level with surrounding cartilage, integration with surrounding cartilage, appearance of surface, color of graft, and stiffness on probing to reveal an overall point score from 0 to 10 points. Six orthopaedic surgeons viewed five arthroscopic videotapes in patients who had undergone ACI and scored the chondral surfaces according to both rating systems twice, 6 weeks apart.
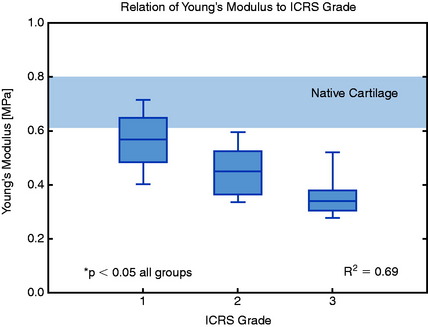
Correlation of ICRS Rating and Changes in Tissue Mechanical Properties
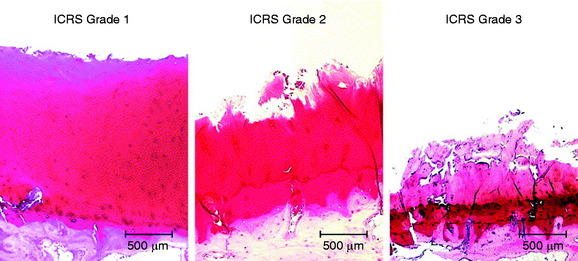
Kleemann and colleagues19 conducted an investigation to determine the relationship between various stages of articular cartilage deterioration, as rated macroscopically by the ICRS system (grades 0–4) and changes in tissue mechanical propeties. Tibial plateaus were collected in 21 patients who underwent total knee arthroplasty and ICRS grades assigned by three surgeons. The specimens were examined biomechanically and histologically using a modified Mankin scoring system (Table 47-6).21 The mechanical properties were measured with a custom-made testing material testing device that determined the Young modulus of the cartilage by unconfined compression. Histologic analysis used hematoxylin and eosin staining and safranin-O staining for the evaluation of the Mankin score.
TABLE 47-6 Mankin Histologic and Histochemical Grading System for Evaluation of Articular Cartilage Degeneration
| Grade | ||
|---|---|---|
| I |
From Mankin, H. J.; Dorfman, H.; Lippiello, L.; Zarins, A.: Biochemical and metabolic abnormalities in articular cartilage from osteoarthritic human hips. II. Correlation of morphology with biochemical and metabolic data. J Bone Joint Surg Am 53:523–537, 1971.
The results showed a correlation between increasing ICRS grade and reduction in stiffness (Young’s modulus) (R2 = 0.69, P < .01; Fig. 47-9). Progressive thinning of the cartilage was noted in specimens rated ICRS grade 3.
Histologic analyses showed a significant correlation between Mankin scores and ICRS grades (R2 = 0.74, P < .01; Figs. 47-10 and 47-11). Higher Mankin scores were obtained with increasing ICRS grades. The mean Mankin scores according to ICRS grades were 3.2 ± 1.5 points for grade 1, 5.7 ± 2.0 points for grade 2, and 7.6 ± 1.7 points for grade 3. A moderate correlation was found between the Mankin score and the Young modulus (R2 = 0.47, P < .02). The authors reported that early stage of degenerative joint disease, ICRS grade 1, was very difficult to detect owing to the “inconspicuous changes of the surface appearance between ICRS Grade 1 and native cartilage.”
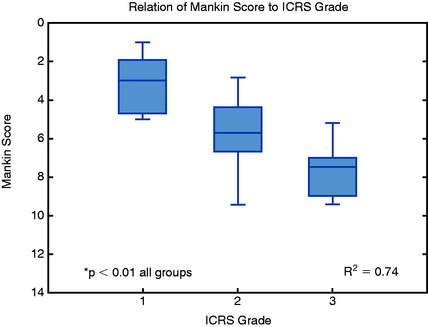
FIGURE 47-10 Stiffness reduction in degenerated cartilage (increasing ICRS grade) related to histologic appearance (Mankin score).
(From Kleemann, R. U.; Krocker, D.; Cedraro, A.; et al.: Altered cartilage mechanics and histology in knee osteoarthritis: relation to clinical assessment [ICRS grade]. Osteoarthritis Cartilage 13:958–963, 2005.)
Sensitivity and Specificity of Standing Radiographs to Detect Mild Osteoarthritis
Wright and coworkers31 determined the sensitivity and specificity of standing anteroposterior (AP) and 45° weight-bearing posteroanterior (PA) radiographs in detecting Outerbridge grade 2 (fragmentation and fissuring, < ½” in diameter) chondral lesions in a group of 349 patients. All patients underwent standing AP and PA views that were measured by two blinded radiologists for articular cartilage narrowing (in millimeters). At arthroscopy, a single surgeon provided Outerbridge gradings. The authors reported that, although both radiographic techniques had specificity rates greater than 90%, both techniques had poor sensitivity rates for detecting grade 2 changes in the medial (3% AP; 6% PA) and lateral (16% AP; 6% PA) compartments. Lysholm and associates20 reported a similar poor correlation between mild osteoarthritis (Outerbridge grade 2) and the Ahlbäck classification1 rating of standing radiographs.20
1 Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;277(Suppl):7-72.
2 Beguin J., Locker B. Chondropathie rotulienne. 2ème Journèe d’Arthroscopie du Genou. 1983;1:89-90.
3 Brismar B.H., Wredmark T., Movin T., et al. Observer reliability in the arthroscopic classification of osteoarthritis of the knee. J Bone Joint Surg Br. 2002;84:42-47.
4 Brittberg M. Evaluation of cartilage injuries and cartilage repair. Osteologie. 2000;9:17-25.
5 Brittberg M., Peterson L. Introduction of an articular cartilage classification. ICRS Newsl. 1998;1:5-8.
6 Brittberg M., Winalski C.S. Evaluation of cartilage injuries and repair. J Bone Joint Surg Am. 2003;85(suppl 2):58-69.
7 Cameron M.L., Briggs K.K., Steadman J.R. Reproducibility and reliability of the Outerbridge classification for grading chondral lesions of the knee arthroscopically. Am J Sports Med. 2003;31:83-86.
8 Casscells S.W. Gross pathological changes in the knee joint of the aged individual: a study of 300 cases. Clin Orthop Relat Res. 1978;132:225-232.
9 Collins D.H., editor. The Pathology of Articular and Spinal Diseases. London: Edward Arnold, 1949.
10 Curl W.W., Krome J., Gordon E.S., et al. Cartilage injuries: a review of 31,516 knee arthroscopies. Arthroscopy. 1997;13:456-460.
11 Dougados M., et al. The SFA system for assessing articular cartilage lesions at arthroscopy of the knee. Arthroscopy. 1994;10:69-77.
12 Ficat R.P., Hungerford D.S. Chondrosis and arthrosis: a hypothesis. In: Ficat R.P., Hungerford D.S., editors. Disorders of the Patellofemoral Joint. Baltimore: Williams & Wilkins; 1977:194-232.
13 Ficat R.P., Philippe J., Hungerford D.S. Chondromalacia patellae: a system of classification. Clin Orthop Relat Res. 1979;144:55-62.
14 Goodfellow J., Hungerford D.S., Zindel M. Patello-femoral joint mechanics and pathology. 1. Functional anatomy of the patello-femoral joint. J Bone Joint Surg Br. 1976;58:287-290.
15 Goodfellow J., Hungerford D.S., Woods C. Patello-femoral joint mechanics and pathology. 2. Chondromalacia patellae. J Bone Joint Surg Br. 1979;58:291-299.
16 Hefti F., Muller W., Jakob R.P., Staubli H.U. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226-234.
17 Hunt N., Sanchez-Ballester J., Pandit R., et al. Chondral lesions of the knee: a new localization method and correlation with associated pathology. Arthroscopy. 2001;17:481-490.
18 Insall J., Falvo K.A., Wise D.W. Chondromalacia patellae. A prospective study. J Bone Joint Surg Am. 1976;58:1-8.
19 Kleemann R.U., Krocker D., Cedraro A., et al. Altered cartilage mechanics and histology in knee osteoarthritis: relation to clinical assessment (ICRS grade). Osteoarthritis Cartilage. 2005;13:958-963.
20 Lysholm J., Hamberg P., Gillquist J. The correlation between osteoarthrosis as seen on radiographs and on arthroscopy. Arthroscopy. 1987;3:161-165.
21 Mankin H.J., Dorfman H., Lippiello L., Zarins A. Biochemical and metabolic abnormalities in articular cartilage from osteo-arthritic human hips. II. Correlation of morphology with biochemical and metabolic data. J Bone Joint Surg Am. 1971;53:523-537.
22 Marx R.G., et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33:1654-1657.
23 Mehta V.M., Paxton L.W., Fornalski S.X., et al. Reliability of the International Knee Documentation Committee radiographic grading system. Am J Sports Med. 2007;35:933-935.
24 Noyes F.R., Barber-Westin S.D. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft in patients with articular cartilage damage. Am J Sports Med. 1997;25:626-634.
25 Noyes F.R., Barber-Westin S.D. Arthroscopic-assisted allograft anterior cruciate ligament reconstruction in patients with symptomatic arthrosis. Arthroscopy. 1997;13:24-32.
26 Noyes F.R., Barber-Westin S.D. Revision anterior cruciate surgery with use of bone–patellar tendon–bone autogenous grafts. J Bone Joint Surg Am. 2001;83:1131-1143.
27 Noyes F.R., Barber-Westin S.D., Roberts C.S. Use of allografts after failed treatment of rupture of the anterior cruciate ligament. J Bone Joint Surg Am. 1994;76:1019-1031.
28 Noyes F.R., Stabler C.L. A system for grading articular cartilage lesions at arthroscopy. Am J Sports Med. 1989;17:505-513.
29 Outerbridge R.E. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752-757.
30 Smith G.D., Taylor J., Almqvist K.F., et al. Arthroscopic assessment of cartilage repair: a validation study of 2 scoring systems. Arthroscopy. 2005;21:1462-1467.
31 Wright R.W., Boyce R.H., Michener T., et al. Radiographs are not useful in detecting arthroscopically confirmed mild chondral damage. Clin Orthop Relat Res. 2006;442:245-251.