Chapter 8 Arthrosis Following Anterior Cruciate Ligament Tear and Reconstruction
Pathophysiology of Osteoarthritis Following Anterior Cruciate Ligament Injury
Previous studies have shown that restoring knee stability through ACL reconstruction does not necessarily decrease the incidence of posttraumatic OA.1,2 It therefore follows that other mechanisms, rather than the initial mechanical disturbance of stability at the time of injury, may be responsible for the development of OA, both in the chronic ACL deficient knee and in the reconstructed knee.
Several biochemical mechanisms have been proposed. It has been shown that an early increase in the proteoglycan content of articular cartilage adjacent to the torn ligament occurs following ACL rupture.3 Other studies4,5 have shown an increase in collagenase activity leading to increased denaturation and loss of type II collagen in the articular cartilage of the knee following injury. These changes are also seen in the knee with idiopathic OA.
Intraarticular pro-inflammatory cytokines are also increased immediately after ACL rupture.6,7 These include interleukins (IL) -1, -6, and -8, tumor necrosis factor alpha (TNF-α), and keratan sulfate. Of note, IL-1 (in both its alpha and beta forms) and TNF-α have direct chondrodestructive effects independent of their inflammatory properties. These cytokines are present in higher concentrations with more severe chondral damage, and levels fall gradually beginning approximately 3 months postinjury. Granulocyte-macrophage colony-stimulating factor (GM-CSF) concentrations are initially normal but become grossly elevated beginning approximately 3 months postinjury. Conversely, the chondroprotective cytokine IL-1Ra concentration decreases with increasing severity of chondral damage and with chronic ACL deficiency.
It has been shown that ligamentous knee injury is strongly associated with bone bruising.8 Magnetic resonance imaging (MRI) scans performed acutely following ACL rupture have shown occult subchondral lesions in 85% of patients, mainly involving the lateral femoral condyle and lateral tibial plateau.9 Although the majority of these lesions resolved with time, permanent chondral damage is known to have occurred in some lesions. Histological analysis of these bone bruises has shown associated areas of chondrocyte degeneration and necrotic osteocytes, which suggests that significant damage to the articular cartilage is sustained at the time of injury.10
Following ACL reconstruction, further factors may play an additional role in the development of arthrosis. It has been shown that pretensioning the graft can cause changes in joint biomechanics that may lead to arthrosis in the long term.11,12 Shortening of the patellar tendon may occur after patellar tendon autograft, which has been shown to lead to patellofemoral arthrosis and a worse functional outcome, both of which are directly associated with the degree of shortening of the patellar tendon.13
Any intraarticular damage that requires treatment with meniscectomy will diminish the joint contact surface area and increase the stress on the tibia.14 The resultant increased stress on the knee joint has been shown to accelerate the development of OA.15
Natural History of the Untreated Anterior Cruciate Ligament Deficient Knee
The development of arthrosis following ACL rupture is widely recognized,16,17 and in a review by Gillquist and Messner18 it was concluded that in the long term (i.e., 10 to 20 years), as many as 70% of all ACL deficient knees had radiological signs of arthrosis, although clinical symptoms of knee arthritis were infrequent. Segawa et al19 found radiographic changes of OA in 63% of patients who were followed for 12 years after a conservatively treated ACL rupture. The main risk factor for arthrosis was shown to be meniscectomy, in combination with the risk factors for primary OA, such as increased age at time of injury, increased level of sports activity, obesity, and OA of the contralateral knee.
In a study of patients with symptomatic knee OA, 22.8% had complete ACL rupture identified at MRI, compared with 2.7% of controls.20 Patients with OA in the presence of an ACL rupture had more severe radiological OA.
A cohort of female soccer players in Sweden was assessed 12 years after a known ACL injury, and although radiographic evidence of OA was seen in 82%, there was no difference in the incidence of OA between those ACL injuries treated nonoperatively (38%) and those treated with reconstruction, and the same proportion (75%) of those without radiographic OA had knee symptoms.2 Comparable results were seen in a similar study of male soccer players in Sweden 14 years following a known ACL injury.21
In children and adolescents with ACL rupture, nonoperative treatment is often favored to avoid drilling surgical tunnels across physeal growth plates. However, it has been shown that ACL injuries treated nonoperatively in this age group are likely to develop instability and poor function, with development of radiological signs of degeneration in almost half of children.22 Subsequent studies have shown that ACL reconstruction can be safely undertaken in adolescents nearing skeletal maturity.23 It has not yet been proven that this can be safely performed in very young children with opened physes.
Despite this evidence, some studies challenge the concept that ACL tears are inextricably linked to development of arthritis. It has been shown that in older patients (40 to 60 years old) with an ACL rupture treated nonoperatively, 87% had little or no radiographic changes at a mean of 7 years postinjury.24 In 46 young recreational athletes followed up at an average of 5 years following conservative treatment of an ACL tear diagnosed at arthroscopy, only 17.4% had mild radiographic osteoarthritic changes, and only one patient (2.2%) was symptomatic.25
Arthrosis Following Anterior Cruciate Ligament Reconstruction
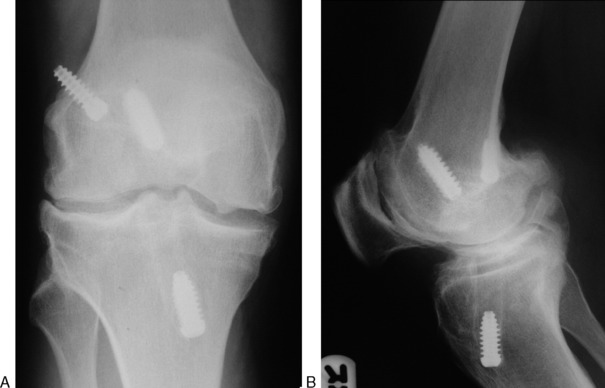
With the knowledge that ACL tears are associated with an increased risk of OA, it would seem reasonable to assume that ACL reconstruction would play a useful role in prevention of arthrosis in the long term. The difficulties in implementing large long-term follow-up studies following ACL reconstruction have already been mentioned. Table 8-1 summarizes the recent literature that has evaluated the incidence of arthrosis following ACL reconstruction. Analysis of these studies clearly suggests that surgical reconstruction of the ligament does not prevent the development of radiological OA. A meta-analysis by Lohmander and Roos26 found no evidence that ACL reconstruction slowed the progression of arthrosis following ACL rupture, and it does not seem that ACL reconstruction reduces the clinical symptoms of OA in the long term.2 However, it is noteworthy that most authors have found the majority of patients to be essentially asymptomatic at follow-up, regardless of the radiological changes, which are often mild. Clearly a spectrum of joint changes exists, with many patients demonstrating minimal radiographic change and few clinical symptoms, although unfortunately a minority will go on to have symptomatic arthrosis (Fig. 8-1).
Table 8-1 Summary of Studies Reporting Results Following Anterior Cruciate Ligament (ACL) Reconstruction
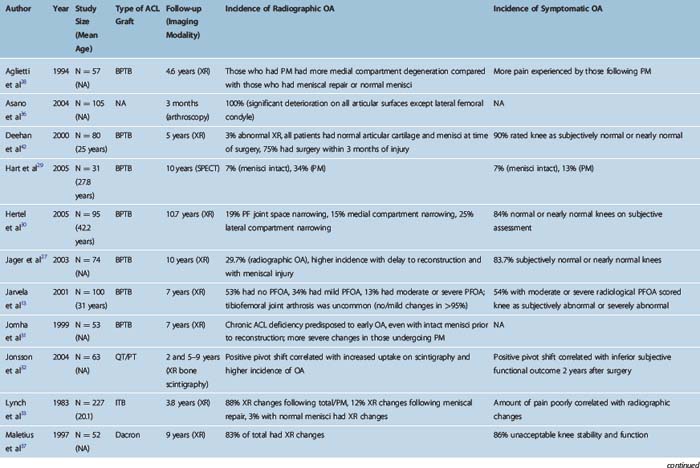
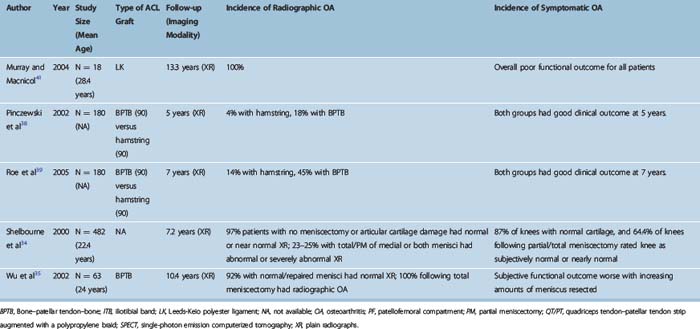
As with conservatively managed ACL tears, the major risk factor associated with the development of OA is meniscal damage27 and the need for meniscal resection at the time of surgery.28–35 Some authors maintain that chondral damage is of more importance than medial meniscal tears, which in turn are more significant than lateral meniscal tears in the development of OA.34 However, even in the absence of chondral damage or meniscal injury, early mild degenerative changes may occur after successful ACL reconstruction.36 Other risk factors appear to be female gender and age older than 30 years,36,37 presence of persistent pivot shift following reconstruction,32 bone–patellar tendon–bone autograft compared with hamstring autograft,38,39 time to surgery,27,33,40 synthetic graft material,37,41 and maintenance of high levels of sporting activity after surgery.42 Surgery within 12 months of injury40,42 appears to reduce the incidence of arthrosis. There does not appear to be any benefit to surgery earlier than 3 months postinjury.43 Anteroposterior (AP) instability post reconstruction does not appear to be a risk.36,32
Looking at the most up-to-date studies that have followed patients undergoing ACL reconstruction using modern graft materials, it appears that the rate of radiographic degenerative changes is between 4% and 47% between 5 and 10 years of follow-up. This figure has been shown to rise as high as 100% following ACL reconstruction with a total meniscectomy.35 It has even been reported that the rate of degenerative change is higher in the reconstructed knee compared with the chronic ACL deficient knee.1 This is probably due to the fact that those patients who have symptomatic instability and require ACL reconstruction are more likely to have concomitant meniscal and/or chondral damage predisposing to the development of OA. By comparison, those patients with normal articular cartilage and menisci can often be satisfactorily managed conservatively.
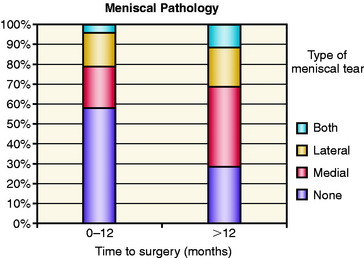
In our own study40 we investigated the relationship of time from injury to surgery on the incidence of meniscal tears and degenerative change. We evaluated 183 patients who underwent ACL reconstruction for isolated ACL tears using a quadruple hamstring graft. An arthroscopically assisted single-incision technique was used. Patients were divided into an early group (surgery within 12 months of injury) and a late group (surgery more than 12 months from injury). The late group was also subdivided into four groups of 12-month periods ranging from 1 year to more than 4 years after injury. There was a significantly higher incidence of meniscal tears in patients undergoing reconstruction after 12 months compared with those in the early group (71.2% versus 41.7%, P < 0.001) (Fig. 8-2). This was due to a large increase in medial meniscal tears in the late group. The incidence of lateral meniscal tears remained relatively unchanged with time. This may indicate that lateral meniscal tears occur at the time of ACL injury or very early after injury, whereas the majority of medial meniscal tears are acquired after the initial ACL tear. The increase in medial meniscal tears after 12 months probably correlates with an attempted return to preinjury levels of sporting activity. The data are consistent with development of knee instability associated with a return to sport, with increased torsional and shear forces resulting in acquired medial meniscal injuries and acceleration of degenerative change in the knee.
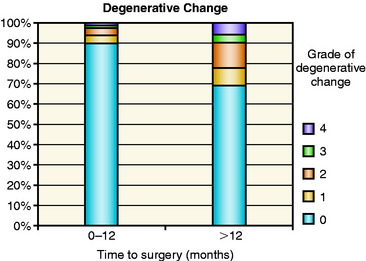
We also found an increased incidence of degenerative change in the late group (31.3% versus 10.7%, P < 0.001) (Fig. 8-3), even though the majority of patients in both groups had no degenerative change at all. The findings in the study indicate that reconstruction carried out within 1 year of injury is associated with a very low incidence of degenerative change. It remains to be seen whether an ACL reconstruction carried out at this stage confers a longer-term benefit in prevention of late degenerative change. In a recent study44 using modern reconstruction techniques with a hamstring autograft, the reported incidence of significant radiographic degenerative change at 2- to 8-years follow-up was only 4%, and these occurred in patients who had undergone meniscectomy. It is possible, therefore, that early reconstruction carried out in the presence of intact menisci may carry a more favorable prognosis with a lower incidence of arthrosis in the longer term.
1 Daniel DM, Stone ML, Dobson BE, et al. Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med. 1994;22:632-644.
2 Lohmander LS, Ostenberg A, Englund M, et al. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145-3152.
3 Nelson F, Billinghurst RC, Pidoux I, et al. Early post-traumatic osteoarthritis-like changes in human articular cartilage following rupture of the anterior cruciate ligament. Osteoarthritis Cartilage. 2006;14:114-119.
4 Price JS, Till SH, Bickerstaff DR, et al. Degradation of cartilage type II collagen precedes the onset of osteoarthritis following anterior cruciate ligament rupture. Arthritis Rheum. 1999;42:2390-2398.
5 Lohmander LS, Atley LM, Pietka TA, et al. The release of cross-linked peptides from type II collagen into human synovial fluid is increased soon after injury and in osteoarthritis. Arthritis Rheum. 2003;48:3130-3139.
6 Cameron M, Buchgraber A, Passler H, et al. The natural history of the anterior cruciate ligament-deficient knee. Changes in synovial fluid cytokine and keratan sulfate concentrations. Am J Sports Med. 1997;25:751-754.
7 Marks PH, Donaldson ML. Inflammatory cytokine profiles associated with chondral damage in the anterior cruciate ligament-deficient knee. Arthroscopy. 2005;21:1342-1347.
8 Bretlau T, Tuxoe J, Larsen L, et al. Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc. 2002;10:96-101.
9 Rosen MA, Jackson DW, Berger PE. Occult osseous lesions documented by magnetic resonance imaging associated with anterior cruciate ligament ruptures. Arthroscopy. 1991;7:45-51.
10 Johnson DL, Urban WPJr, Caborn DN, et al. Articular cartilage changes seen with magnetic resonance imaging-detected bone bruises associated with acute anterior cruciate ligament rupture. Am J Sports Med. 1998;26:409-414.
11 Good L, Askew MJ, Boom A. Kinematic in vitro comparison between the normal knee and two techniques for reconstruction of the anterior cruciate ligament. Clin Biomech. 1993;8:243-249.
12 Heerwaarden van RJ, Stellinga D, Frudiger AJ. Effect of pretension on reconstructions of the anterior cruciate ligament with a Dacron prosthesis. A retrospective study. Knee Surg Sports Traumatol Arthrosc. 1996;3:202-208.
13 Jarvela T, Paakkala T, Kannus P, et al. The incidence of patellofemoral osteoarthritis and associated findings 7 years after anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Am J Sports Med. 2001;29:18-24.
14 Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee: a study of normal and osteoarthrotic knee joints. Acta Orthop Scand. 1980;51:871-879.
15 Englund M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50:2811-2819.
16 Kannus P, Jarvinen M. Conservatively treated tears of the anterior cruciate ligament. Long-term results. J Bone Joint Surg Am. 1987;69:1007-1012.
17 Roos H, Adalberth T, Dahlberg L, et al. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthritis Cartilage. 1995;3:261-267.
18 Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999;27:143-156.
19 Segawa H, Omori G, Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2001;8:5-11.
20 Hill CL, Seo GS, Gale D, et al. Cruciate ligament integrity in osteoarthritis of the knee. Arthritis Rheum. 2005;52:794-799.
21 von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269-273.
22 Aichroth PM, Patel DV, Zorrilla P. The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. A prospective review. J Bone Joint Surg Br. 2002;84:38-41.
23 Aronowitz ER, Ganley TJ, Goode JR, et al. Anterior cruciate ligament reconstruction in adolescents with open physes. Am J Sports Med. 2000;28:168-175.
24 Ciccotti MG, Lombardo SJ, Nonweiler B, et al. Non-operative treatment of ruptures of the anterior cruciate ligament in middle-aged patients. Results after long-term follow-up. J Bone Joint Surg Am. 1994;76:1315-1321.
25 Shirakura K, Terauchi M, Kizuki S, et al. The natural history of untreated anterior cruciate tears in recreational athletes. Clin Orthop Relat Res. 1995;317:227-236.
26 Lohmander LS, Roos H. Knee ligament injury, surgery and osteoarthrosis. Truth or consequences? Acta Orthop Scand. 1994;65:605-609.
27 Jager A, Welsch F, Braune C, et al. Ten year follow-up after single incision anterior cruciate ligament reconstruction using patellar tendon autograft. Z Orthop Ihre Grenzgeb. 2003;141:42-47.
28 Aglietti P, Zaccherotti G, De Biase P, et al. A comparison between medial meniscus repair, partial meniscectomy, and normal meniscus in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1994;307:165-173.
29 Hart AJ, Buscombe J, Malone A, et al. Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament: a study using single-photon emission computed tomography at ten years. J Bone Joint Surg Br. 2005;87:1483-1487.
30 Hertel P, Behrend H, Cierpinski T, et al. ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc. 2005;13:248-255.
31 Jomha NM, Borton DC, Clingeleffer AJ, et al. Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999;358:188-193.
32 Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand. 2004;75:594-599.
33 Lynch MA, Henning CE, Glick KRJr. Knee joint surface changes. Long-term follow-up meniscus tear treatment in stable anterior cruciate ligament reconstructions. Clin Orthop Relat Res. 1983;172:148-153.
34 Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery. Five- to fifteen-year evaluations. Am J Sports Med. 2000;28:446-452.
35 Wu WH, Hackett T, Richmond JC. Effects of meniscal and articular surface status on knee stability, function, and symptoms after anterior cruciate ligament reconstruction: a long-term prospective study. Am J Sports Med. 2002;30:845-850.
36 Asano H, Muneta T, Ikeda H, et al. Arthroscopic evaluation of the articular cartilage after anterior cruciate ligament reconstruction: a short-term prospective study of 105 patients. Arthroscopy. 2004;20:474-481.
37 Maletius W, Gillquist J. Long-term results of anterior cruciate ligament reconstruction with a Dacron prosthesis. The frequency of osteoarthritis after seven to eleven years. Am J Sports Med. 1997;25:288-293.
38 Pinczewski LA, Deehan DJ, Salmon LJ, et al. A five-year comparison of patellar tendon versus four-strand hamstring tendon autograft for arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med. 2002;30:523-536.
39 Roe J, Pinczewski LA, Russell VJ, et al. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005;33:1337-1345.
40 Church S, Keating JF. Reconstruction of the anterior cruciate ligament. Timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87:1639-1642.
41 Murray AW, Macnicol MF. 10–16 year results of Leeds-Keio anterior cruciate ligament reconstruction. Knee. 2004;11:9-14.
42 Deehan DJ, Salmon LJ, Webb VJ, et al. Endoscopic reconstruction of the anterior cruciate ligament with an ipsilateral patellar tendon autograft. A prospective longitudinal five-year study. J Bone Joint Surg Br. 2000;82:984-991.
43 Meighan A, Keating JF, Will E. Early versus delayed reconstruction for acute ACL tears: a prospective randomised trial. J Bone Joint Surg Br. 2003;85:521-524.
44 Prodromos CC, Han YS, Keller BL, et al. Stability results of hamstring anterior cruciate ligament reconstruction at 2- to 8-year follow-up. Arthroscopy. 2005;21:138-146.