CHAPTER 33 Arthroscopic Wafer Resection
Ulnar impaction syndrome or ulnocarpal abutment refers to impaction of the ulnar head against the ulnar carpus, which results in persistent ulnar-sided wrist pain. Additional symptoms may include decreased range of motion, weakness of grip, and clicking of the wrist.1 A positive or neutral ulnar variance is present in 70% of cases as seen on standardized radiographs.2 However, ulnar-negative wrists may present with dynamic ulnar impaction with forceful grip, axial load, forearm pronation, and wrist ulnar deviation.1,3 A positive ulnar variance may be a normal anatomical variant or result after a traumatic injury or abnormal development. Frequent causes include distal radius malunion with loss of radial height, premature distal radial physeal closure, and proximal radial migration after radial head excision. Developmental causes include Madelung’s deformity and multiple enchondromatoses, among others, that affect the distal radius.4,5
Injury to the triangular fibrocartilage complex (TFCC) occurs early in the disease process and has been staged by Palmer as a class II TFCC abnormality (Box 33-1).6,7 Chronic ulnar impaction results in a degenerative TFCC wear, chondromalacia of the lunate or ulnar head, attenuation or tearing of the lunotriquetral interosseous ligament, and, lastly, osteoarthritis of the ulnar carpus. This spectrum of findings has been termed “ulnar impaction syndrome.” TFCC traumatic injuries or class I injuries respond well to repair or débridement.6 However, TFCC tears in degenerative ulnar impaction syndrome have a failure rate as high as 25% with TFCC débridement alone.8–11
Box 33-1 Classification of TFCC Tears
Treatment for ulnar impaction syndrome has focused on mechanically unloading the ulnar side of the wrist. Palmer and Werner demonstrated that load distribution across the distal radius and ulna is dependent on ulnar variance.12 In an ulnar-neutral wrist, 82% of force transmission crosses the radiocarpal joint and 18% crosses the ulnocarpal joint. With 2.5 mm of ulnar lengthening, the force across the ulnocarpal joint increases to 41.9%. When the ulna is shortened 2.5 mm from neutral, force transmission across the ulnocarpal drops to 4.3% and the radiocarpal force transmission increases to 95.7%. The force across the ulnocarpal joint is constant in the native wrist regardless of ulnar variance.5,13 This is because the thickness of the TFCC is variable. It is thicker in an ulnar-negative wrist and thinner in an ulnar-positive wrist. Disruption of the ulnar variance from its native state will alter the ulnocarpal mechanics. Procedures designed to mechanically unload the ulnocarpal joint include an ulnar-shortening osteotomy, open wafer resection, and arthroscopic wafer resection. More invasive procedures include distal ulnar resection (Darrach), the Sauvé-Kapandji procedure, and the hemi-resection interpositional arthroplasty. These techniques should be reserved as salvage procedures. Of these, only the Darrach resection completely unloads the ulnocarpal joint.7,14
Ulnar shortening has given excellent results in the treatment of ulnar impaction syndrome. Milch first described an ulnar shortening in 1941 for a malunited Colles fracture.15 Subsequent modification of the subperiosteal cuff resection by substituting the AO-ASIF principles of rigid plate fixation produced excellent to good results in 93% of patients treated with an ulnar shortening osteotomy for ulnar impaction syndrome.5,16–18 On average, 3 months of postoperative immobilization is required. Complications from an ulnar-shortening osteotomy include extensor carpi ulnaris tendinitis from hardware irritation and delayed union and nonunion of the osteotomy. Tendinitis necessitating removal of the plate has been reported to be as high as 52%.19 Delayed union (>3 months) of the osteotomy has been reported in 18% to 22% of cases.20
An open wafer distal ulnar resection was first published by Feldon and associates in 1992.2 This procedure does not require internal fixation, and it does not require union of an osteotomy. However, it is contraindicated in patients with degenerative arthritis or instability of the distal radioulnar joint (DRUJ) or an ulnar variance greater then 4 mm positive. It is performed through a dorsal approach between the fifth and sixth extensor compartments, as described by Bowers. A radially based, U-shaped flap of the DRUJ capsule is created to expose the DRUJ, TFCC, and proximal articular surfaces of the lunate and triquetrum. After inspection, an osteotome is used to remove 2 to 4 mm of the ulnar head, including articular cartilage and subchondral bone. Care is taken to preserve the styloid process and all TFCC attachments. In addition, the majority of the cartilage articulating with the sigmoid notch of the radius is retained to preserve DRUJ function (forearm rotation). Débridement or repair of the TFCC is also performed. Intraoperative fluoroscopy is used to ensure that 2 mm of ulnar-negative variance is created. Good to excellent results have been obtained in 85% to 100% of patients with near full recovery of motion and grip strength.2,16,21–23 However, tendinitis of the extensor carpi ulnaris sheath occurred in up to 31% of patients.21 When compared with an ulnar-shortening osteotomy for initial treatment of ulnar impaction syndrome, no clinical difference in outcome has been found.19
Arthroscopic wafer distal ulna resection was first reported in the early 1990s for patients presenting with extensive degenerative TFCC tears, chondromalacia of the ulnar head, or arthritis of the DRUJ.8 In one biomechanical study it was shown that excision of the centrum of the TFCC and resection of the radial two-thirds width of the ulnar head to a depth of subchondral bone revealed statistically significant unloading of the ulnar aspect of the wrist.7 It was also shown that ulnocarpal force transmission decreased with continued ulnar recession with maximal unloading at 3 mm of subchondral resection where force was reduced to 10.8%. No correlation with ulnar variance and resection level was observed. However, a trend was observed between optimal unloading and stage. Stage IIB wrists were unloaded with central TFCC excision. Stage IIC wrists tended to be unloaded after TFCC excision and one-third ulnar articular cartilage resection. Lastly, stage IID wrists were unloaded after resection into subchondral bone.7 In 12 wrists with ulnar-positive variance, Tomaino found 67% of patients to be completely pain free and 33% to have minimal symptoms at 14 months after arthroscopic wafer resection.11 All patients were satisfied, and all had a negative ulnocarpal stress test. Preoperative ulnar variance averaged 2 mm positive and was neutral postoperatively. It has also been shown in patients presenting with ulnocarpal abutment syndrome that patients treated initially with an arthroscopic wafer resection had no statistically significant difference in outcome than those treated with arthroscopic TFCC débridement and an ulnar-shortening osteotomy.20
Physical Findings
On physical examination, the wrist is frequently benign in appearance. However, there may be associated swelling over the ulnocarpal joint. Wrist and forearm range of motion are usually full and equal to that of the contralateral side unless the symptoms are secondary to a previous injury or congenital malformation. Pain with palpation is usually localized over the ulnocarpal joint and proximal triquetrum. Pain may be elicited with compression of the TFCC by ulnar deviation of the wrist with simultaneous pronation/supination of the ulnocarpal joint (TFCC compression test).16 If a click is felt or heard, a TFCC tear may also be present.24,25 Pain may also be produced if a tear of the lunotiquetral ligament is present with ballottement of the lunotriquetral joint.
Diagnostic Studies
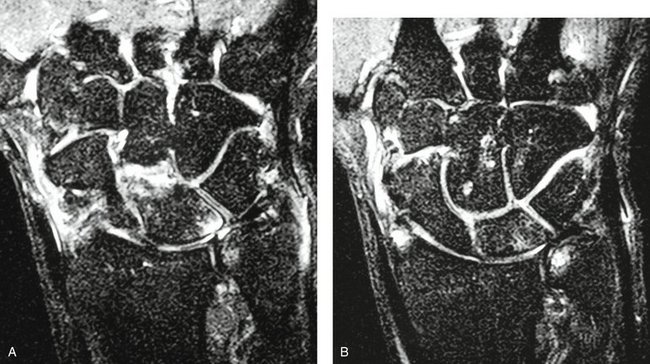
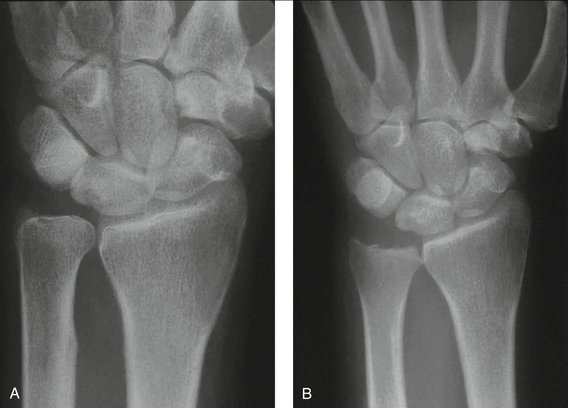
Imaging studies frequently used to evaluate ulnar-sided wrist pain include radiographs, magnetic resonance imaging (MRI), and computed tomography (CT). Radiographs are frequently used to determine ulnar variance, wrist alignment, and joint integrity. Ulnar variance is assessed on a posteroanterior radiograph with the forearm and wrist in neutral rotation (Fig. 33-1). This is easily obtained with the shoulder abducted, elbow flexed 90 degrees, and the wrist lying flat on the radiograph plate.3 Most patients with ulnocarpal impaction will have an ulnar-positive variance. Cystic changes may be present on both the proximal ulnar lunate and ulnar head. To assess for dynamic ulnar carpal impaction, the posteroanterior radiograph should be obtained with the forearm pronated and with forceful grip.13 A lateral radiograph should also be obtained to assess for possible volar intercalated segmental instability. Contrast-enhanced MRI may be helpful to assess the integrity of the TFCC, lunotriquetral ligament, and lunate. Increased signal enhancement may be present in the proximal ulnar portion of the lunate and should not be confused with Kienböck’s disease, which would involve the entire lunate (Fig. 33-2). If malunion or osseous malalignment is suspected, CT with three-dimensional reconstructions may be helpful.
Wrist arthroscopy remains the gold standard for assessing internal derangement of the wrist. It provides both diagnostic as well as therapeutic benefit. Arthroscopy should be considered in patients with suspected ulnar impaction syndrome who have failed at least 3 to 4 months of conservative management. It allows assessment of the TFCC, extrinsic and intrinsic ligaments, as well as the integrity of the joint surfaces.
Indications
Partial wafer resection of the distal ulna is a procedure designed to treat symptomatic TFC tears associated with a positive or neutral ulnar variance and ulnar impaction syndrome, with a dynamic ulnar-positive variance, or ulnocarpal chondromalacia.2,4,11,16,17,21–23 In skeletally mature patients with ulnar impaction syndrome who are found to have a TFCC perforation without arthritic change (type II C and D TFCC tears) an arthroscopic wafer resection can be used to shorten the ulna by up to 4 mm.2,11,16,21 It is still controversial for patients with ulnar impaction syndrome and an intact TFCC (type II A and B lesions) to undergo resection of the TFCC to perform an arthroscopic wafer procedure.
Contraindications
Arthroscopic wafer resection is contraindicated in patients with symptomatic ulnar impaction syndrome who require greater than 4 mm of shortening.2 It is also not indicated in patients who have instability or degenerative arthritis of the DRUJ.21 Patients with advanced ulnocarpal arthritis or with significant instability of the wrist will also unlikely benefit from an arthroscopic wafer procedure.16
Surgical Technique
With the patient under general anesthesia or sedation with an upper extremity nerve block, a standard wrist arthroscopy is performed. The patient is positioned supine on the operating table with the shoulder abducted 90 degrees and centered on a hand table. An examination under anesthesia is then performed to assess for any instability of the DRUJ in both pronation and supination. A well-padded arm tourniquet is then applied and the upper extremity prepared and draped in the usual sterile fashion. After finger traps are applied, the arm is securely fastened in a well padded traction tower with 10 to 15 lb of traction across the wrist. The forearm is placed in neutral rotation, and the wrist is flexed 10 to 15 degrees (Fig. 33-3).
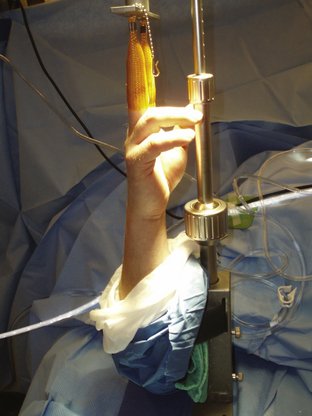
FIGURE 33-3 Example of a standard wrist arthroscopic setup. Note that the forearm rotation is neutral.
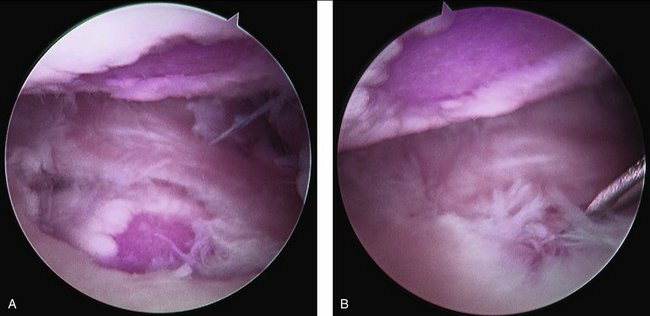
Inspection of the chondral surfaces of the scaphoid, lunate, and distal radius is performed. With ulnar impaction syndrome, chondromalacia is frequently present on the ulnar half of the proximal lunate. A reciprocal “kissing lesion” may be present on the ulnar head and may be easily seen if a full-thickness central TFCC tear is present (Fig. 33-4). This is also usually accompanied by synovitis, which should be débrided to allow adequate visualization. This is best accomplished with a heat probe and small shaver. Care must be used to avoid débridement of the extensor tendons dorsally.
The radiocarpal, ulnocarpal, scapholunate, and lunotriquetral ligaments are then assessed and probed. Full evaluation of the lunotriquetral ligament requires the camera to be switched to the 4-5 portal or the alternate 6R portal. Suspected scapholunate and lunotriquetral tears can be confirmed by “air arthrogram.” This is accomplished with the camera in the 3-4 portal. Air is then infiltrated into the midcarpal joint with a syringe and the scapholunate and lunotriquetral ligaments simultaneously visualized for any extravasation of air bubbles through either the scapholunate or lunotriquetral ligaments, respectively. Any scapholunate or lunotriquetral ligament tears should be inspected further through radial or ulnar midcarpal portals.
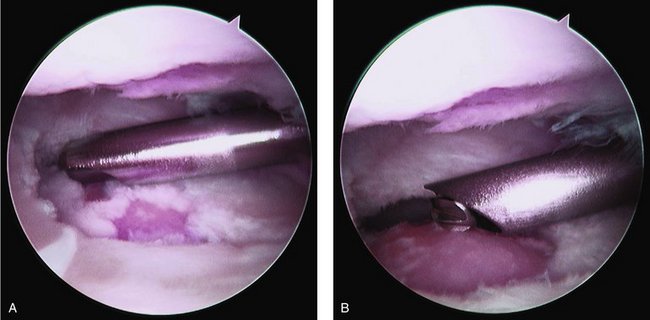
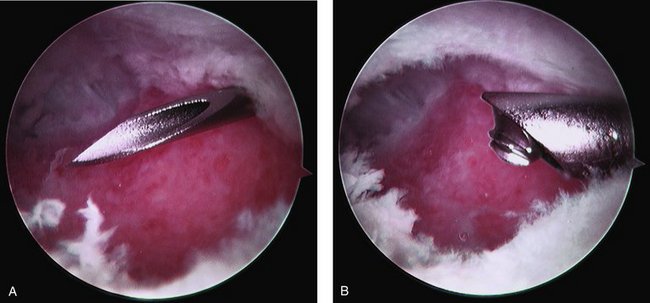
After confirmation of ulnar impaction syndrome, arthroscopic wafer resection can proceed. Using the 3-4, 4-5, and 6R portals, the TFCC tear is débrided with either a suction punch or small arthroscopic shaver (Fig. 33-5). The ulnar head is then inspected for evidence of chondromalacia. A small arthroscopic bur is then placed through the 4-5 portal, and the ulnar head is débrided (Fig. 33-6). Care is taken to both pronate and supinate the forearm as debridement progresses to ensure removal of both the volar and dorsal portions of the ulnar head (Fig. 33-7). After the initial bone resection, a DRUJ portal is created just proximal to the radial attachment of the TFCC. This is created with the aid of a needle to ensure proper placement. The bur is then placed through this portal, and ulnar recession is continued (Fig. 33-8). Caution must be used when progressing ulnarly to ensure that the ulnar styloid is preserved. Throughout the recession, alteration of the working portals as well as the viewing and working portals is required to create an even and sufficient ulnar wafer resection. Fluoroscopy is used intermittently throughout and at the conclusion of the case to ensure complete ulnar recession in both pronation and supination. On a forearm-neutral posteroanterior radiograph, the ulna should be at least neutral if it was positive preoperatively (Fig. 33-9). On average, 2 to 3 mm of distal ulna should be removed. Once the resection is deemed adequate, the wrist is again examined for full forearm rotation and DRUJ stability. The portal sites are closed, and a soft dressing is applied. Mobilization is started after the first postoperative visit.
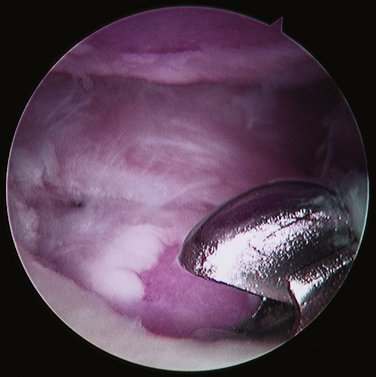
FIGURE 33-5 Intraoperative photograph taken with the arthroscope positioned in the 3-4 portal. A suction punch is used to débride the central TFCC tear back to a stable margin.
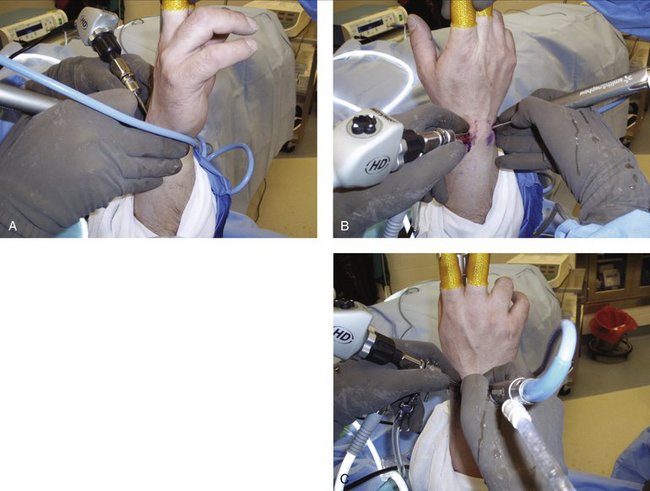
FIGURE 33-7 To ensure complete ulnar head recession, it is frequently necessary to both pronate (A) and supinate (B) the forearm from the neutral (C) position throughout the procedure.
1. Freidman SL, Palmer AK. The ulnar impaction syndrome. Hand Clin. 1999;7:295-310.
2. Feldon P, Terrono AL, Belsky MR. The “wafer” procedure. Clin Orthop Relat Res.. 1992;275:124-129.
3. Epner RA, Bowers WH, Guilford WB. Ulnar variance: the effect of wrist positioning and roentgen filming technique. J Hand Surg.. 1982;7:298-305.
4. Le TB, Vaughan C, Bowen A. Ulnar shortening osteotomy. In: Gelberman RH, Thompson RC, editors. The Wrist: Master Techniques in Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins; 2002:307-321.
5. Chun S, Palmer AK. The ulnar impaction syndrome: follow-up of ulnar shortening osteotomy. J Hand Surg [Am].. 1993;18:46-53.
6. Palmer AK. Triangular fibrocartilage lesions: classification and treatment. J Hand Surg [Am].. 1989;14:594-606.
7. Wnorowski DC, Palmer AK, Werner FW, Fortino MD. Anatomic and biochemical analysis of the arthroscopic wafer procedure. Arthroscopy. 1992;8:204-212.
8. Osterman AL. Arthroscopic débridement of triangular fibrocartialge complex tears. Arthroscopy.. 1990;6:120-124.
9. Westkaemper JG, Mitsionis G, Giannakopoulos PN, Sotereanos DG. Wrist arthroscopy for the treatment of ligament and triangular fibrocartilage complex injuries. Arthroscopy. 1998;14:479-483.
10. Minami A, Ishikawa J, Suenaga N, Kasashima T. Clinical result of treatment of triangular fibrocartilage complex tears by arthroscopic debridement. J Hand Surg [Am].. 1996;21:406-411.
11. Tomaino MW, Weiser RW. Combined arthroscopic TFCC debridement and wafer resection of the distal ulna in wrists with complex tears and positive ulnar variance. J Hand Surg [Am].. 2001;26:1047-1052.
12. Palmer AK, Werner FW. Biomechanics of the distal radio-ulnar joint. Clin Orthop Relat Res.. 1984;187:26-35.
13. Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and triangular fibrocartilage complex thickness. J Hand Surg [Am].. 1984;9:681-683.
14. Werner FW, Glisson RR, Murphy DJ, Palmer AK. Force transmission through the distal radio-ulnar carpal joints: effect of ulnar lengthening and shortening. Handchir.. 1986;18:304-308.
15. Milch H. Cuff resection of the ulna for malunited Colles’ fracture. J Bone Joint Surg. 1941;39:311-313.
16. Loftus JB. Arthroscopic wafer for ulnar impaction syndrome. Tech Hand Upper Extrem Surg.. 2000;4:182-188.
17. Darrow JC, Linscheid RL, Dobyns JH, et al. Distal ulnar recession for disorders of the distal radio-ulnar joint. J Hand Surg [Am].. 1985;10:482-491.
18. Boulas HJ, Milek MA. Ulnar shortening for tears of the triangular fibrocartilaginous complex. J Hand Surg [Am].. 1990;15:415-420.
19. Constantine KJ, Tomaino MM, Herndon JH, Sotereanos DG. Comparison of ulnar shortening osteotomy and wafer resection procedure for ulnar impaction syndrome. J Hand Surg [Am].. 2000;25:55-60.
20. Bernstein MA, Nagle DJ, et al. A comparison of combined arthroscopic triangular fibrocartilage complex débridement and arthroscopic wafer distal ulna resection versus arthroscopic triangular fibrocartilage complex débridement and ulnar shortening osteotomy for ulnocarpal abutment syndrome. Arthroscopy. 2004;20:392-401.
21. Feldon P, Terrono AL, Belsky MR. Wafer distal ulna resection for triangular fibrocartilage tears and/or ulna impaction syndrome. J Hand Surg [Am].. 1992;17:731-737.
22. Bilos ZJ, Chamberland D. Distal ulnar head shortening for treatment of triangular fibrocartilage complex tears with ulna positive variance. J Hand Surg [Am].. 1991;16:1115-1119.
23. Schuurman AH, Bos KE. The ulno-carpal abutment syndrome: follow-up of the wafer procedure. J Hand Surg [Br].. 1995;20:171-177.
24. Roth JH, Poehiling GG. Arthroscopic “ectomy” surgery of the wrist. Arthroscopy. 1990;6:141-147.
25. Hornbach EE, Osterman AL. Partial excision of the triangular fibrocartilage complex. In: Gelberman RH, Thompson RC, editors. The Wrist: Master Techniques in Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins; 2002:279-290.