CHAPTER 26 Arthroscopic Treatment of Triangular Fibrocartilage Complex Injuries
The triangular fibrocartilage complex (TFCC) is a complex anatomical structure located at the ulnar side of the wrist. It has the important biomechanical function of providing stability to both the ulnar carpus and the distal radioulnar joint (DRUJ). Disorders of the TFCC are responsible for the ulnar-sided wrist symptoms of pain, weakness, and instability that affect function. The diagnosis and treatment of these injuries to the TFCC will restore stability, resulting in pain relief and a good prognosis for return of function.
Anatomy
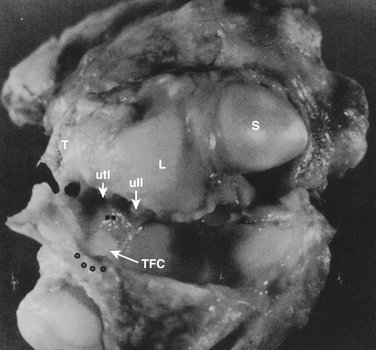
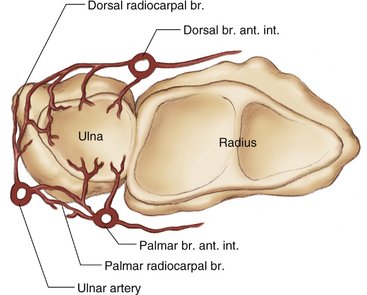
The TFCC is a cartilaginous and ligamentous structure interposed between the ulnar carpus and the distal ulna (Fig. 26-1). It arises from the distal aspect of the sigmoid notch of the radius and inserts into the base of the ulnar styloid. The TFCC attaches to the ulnar carpus via the ulnocarpal ligament complex (ulnolunate, ulnotriquetral, and ulnar collateral ligaments).1–3 The radioulnar ligaments stabilize the DRUJ, limiting rotational as well as axial migration.4 The dorsal and volar radioulnar ligaments (Fig. 26-2) are fibrous thickenings within the substance of the TFCC. As a result of this anatomical configuration, they function as a unit rather than as independent ligaments. The central, horizontal portion of the TFCC is the thinnest portion, composed of interwoven obliquely oriented sheets of collagen fibers5 for the resistance of multidirectional stress.
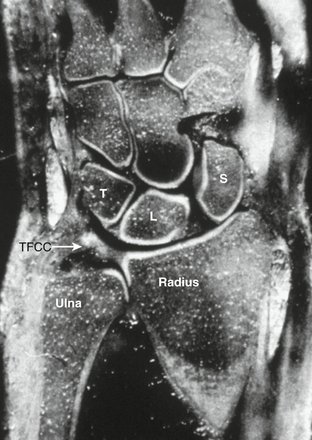
FIGURE 26-1 Anatomical coronal section demonstrating the TFCC and relation to the lunate (L), triquetrum (T), scaphoid (S), and distal ulna and radius.
(From Palmer AK, Werner FW: The triangular fibrocartilage complex of the wrist—anatomy and function. J Hand Surg. 1981; 6A:154.)
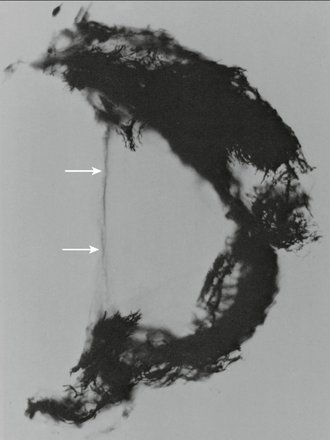
The vascularity of the TFCC has been carefully studied.5–7 The TFCC receives its blood supply from the ulnar artery through its radiocarpal branches and the dorsal and palmar branches of the anterior interosseous artery (Fig. 26-3). These vessels supply the TFCC in a radial fashion. Histologic sections demonstrate that these vessels penetrate only the peripheral 10% to 40% of the TFCC. The central section and radial attachment is avascular (Fig. 26-4). This vascular anatomy supports the concept that peripheral injuries possess the ability to heal if injured and treated appropriately, whereas the tears of the central portion do not heal if sutured and are usually débrided.
Biomechanics
The TFCC has several important biomechanical functions. It transmits 20% of an axially applied load from the ulnar carpus to the distal ulna, it is the major stabilizer of the DRUJ, and it is a stabilizer of the ulnar carpus.3,8–12
The amount of the load transferred to the distal ulna varies with ulnar variance. A greater amount is transferred in ulnar-positive variance than ulnar-negative variance. This results in a corresponding decreased thickness of the central portion of the TFCC in ulnar-positive wrists.10 In addition, there is a variable load placed on the TFCC with forearm rotation. Supination causes ulnar-negative variance owing to the proximal migration of the ulna. This is reversed with pronation as the ulna moves distally, causing it to become ulnar positive.13 The ulnar head also moves within the sigmoid notch in a dorsal direction with pronation and volar with supination.8 The dorsal and volar radioulnar ligaments that form the peripheral portion of the TFCC become tight with forearm rotation, serving as major stabilizers of the DRUJ, which control this translation during rotation.9
Mechanism of Injury
Traumatic injuries of the TFCC result from the application of an extension/pronation force to the axially loaded wrist or by a distraction force to the ulnar aspect of the wrist.1,14 This will most commonly occur with a fall on the outstretched hand. The lesions are more common with ulnar-positive and ulnar-neutral patients and are commonly found in those patients being treated for fractures of the distal radius.
Several authors have examined the incidence of intracarpal soft tissue injuries associated with distal radial fractures. Geissler and coworkers15 studied 60 patients, finding a TFCC injury in 26 (43%). In Lindau and colleagues’ series of 51 patients,16 a TFCC injury was found in 43 (84%): 24 had a peripheral tear, 10 had a central perforation, and 9 had a combined central and peripheral tear. Richards and associates in their series of 118 patients17 reported a TFCC injury in 35% of the patients with intra-articular fractures and 53% of those with extra-articular fractures.
Classification
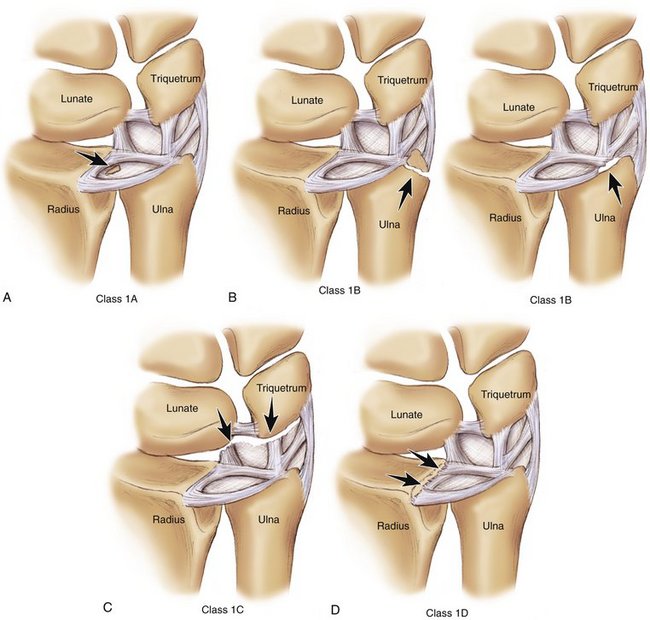
The classification system described by Palmer1 is the most useful for describing TFCC injuries that are both traumatic and degenerative. Only traumatic lesions are discussed here.
A class 1A lesion represents a tear in the horizontal or central portion of the TFCC (Fig. 26-5A). The tear is 2 to 3 mm medial to the radial attachment of the cartilage. It is usually oriented from dorsal to volar.
A class 1B lesion (see Fig. 26-5B) is an avulsion of the peripheral aspect of the TFCC from its insertion onto the distal ulna. This can occur either with a fracture of the ulnar styloid or as a pure avulsion from its bony attachment. This type of injury disrupts the stabilizing effect of the TFCC on the DRUJ, resulting in clinical instability.
A class 1C lesion (see Fig. 26-5C) is an avulsion of the TFCC attachment to the ulnar carpus by disruption of the ulnocarpal ligaments. This lesion will result in ulnar carpal instability with volar translocation of the carpus.
A class 1D lesion (see Fig. 26-5D) is an avulsion of the TFCC from its radial attachment. Involvement of the dorsal and or volar radioulnar ligaments will result in instability of the DRUJ.
Diagnosis
Clinical symptoms consist of ulnar-sided wrist pain frequently with clicking and typically occur after a fall. The initial physical examination reveals swelling over the ulnar aspect of the wrist with inflammation of the tendon of the extensor carpi ulnaris. Point tenderness is present over the TFCC and distal ulna. Ulnar deviation and axial loading of the wrist (TFCC compression test) (Fig. 26-6) will elicit a painful response. A click is frequently present with forearm rotation. The DRUJ must be assessed for instability. Instability is best assessed with the forearm in neutral rotation, but it is also checked in full supination and full pronation. The examiner stabilizes the distal radius with one hand and applies a force to the distal ulna, moving it dorsal and volar in a search for increased motion or subluxation of the distal ulna relative to the radius compared with the opposite uninjured wrist. Significant instability would present as laxity of the distal ulna with a positive “piano key“ sign and dorsal prominence of the distal ulna. This would represent a significant tear or detachment of the dorsal or volar radioulnar ligaments.

FIGURE 26-6 TFCC compression test: ulnar deviation and axial load applied to wrist produces a painful response.
TFCC injuries do not occur in isolation but are a component of a spectrum of injury to the ulnar side of the wrist.18 The examiner must therefore evaluate all of the commonly injured structures on the ulnar side of the wrist. The lunatotriquetral joint must be assessed for instability due to a lunatotriquetral ligament tear. This would cause tenderness over the lunatotriquetral interval with a positive shuck test. The dorsal radial carpal ligament complex should be examined to determine if traumatic midcarpal instability is present.
Imaging
Magnetic resonance imaging (MRI) is useful in the diagnosis of TFCC tears, especially the class 1A and D lesions.19,20 T2-weighted MR images in the coronal plane are of the greatest diagnostic value (Fig. 26-7). The TFCC has a homogeneous low signal intensity. The synovial fluid of the joint appears as a bright image on T2-weighted images and will outline tears in the TFCC. The addition of a gadolinium arthrogram enhances the visualization of TFCC tears.
The series in the literature reviewing the sensitivity and specificity of MRI in diagnosing injuries of the TFCC show significant variation in the reported results. Golimbu and coworkers19 reported a 95% accuracy of MRI in the detection of TFCC tears. They studied 20 patients with the use of MRI. Fourteen of these patients had positive MR studies for TFCC pathology. These patients had surgical examination of the wrist confirming the TFCC pathologic process in 13 of the patients with a positive MRI. None of the patients with a negative MRI had a TFCC pathologic process found at the time of surgery. Schweitzer and associates21 reported in 15 patients a sensitivity of 72%, specificity of 95%, and an accuracy of 89%. Zlatkin and colleagues22 reported a sensitivity of 89%, specificity of 92%, and an accuracy of 90% in 23 patients. Potter and coworkers23 reported a sensitivity of 100%, specificity of 90%, and an accuracy of 97% in 59 patients studied with a high-resolution magnet but they performed arthroscopy only in patients with a positive MRI and therefore could not determine how many patients with a clinical diagnosis of a TFCC injury but a negative MRI had a pathologic process of the TFCC.
Bednar and coworkers24 reported on a series of 75 wrists in 70 patients with a diagnosis of TFCC injury based on clinical criteria. All patients had an MRI examination read by an experienced bone radiologist and then had wrist arthroscopy. The arthroscopic findings were correlated with the MRI and clinical examination. Seventy-one (95%) of the 75 wrists with a clinical diagnosis of TFCC pathology were confirmed to have a TFCC tear by arthroscopy. Thirty-four (48%) had a central tear, 33 (46%) had a peripheral tear, and 4 (6%) had both a central and a peripheral tear. Comparing the arthroscopic with the MRI findings produced 31 (44%) with positive arthroscopic findings and a positive MRI and 40 (56%) with positive arthroscopic findings but a negative MRI; and one of the four wrists with negative findings on arthroscopy had a positive MRI. Correlating TFCC tear type with MRI showed 34 central tears with 19 (56%) MRI positive, 33 peripheral tears with 11 (33%) MRI positive, and 4 central and peripheral tears with 1 (25%) MRI positive. This study produced an MRI sensitivity of 44% (sensitivity is the probability of a positive MRI when a TFCC lesion is present). The clinical examination sensitivity was 95%. If the patients are evaluated using the criteria employed by Potter, the Bednar and coworkers’ study had 32 wrists with a positive MRI, of which 31 were positive by arthroscopy. The sensitivity for this subgroup of MRI-positive patients was 97%. The MRI specificity in the Bednar and coworkers’ study was 75% (specificity is the probability of a negative MRI when a TFCC lesion is absent). The MRI correlated with arthroscopic findings in 45% of the wrists studied.
Joshy and colleagues25 reported a series of 24 patients with a clinical suspicion of TFCC tear studied by direct MR arthrography and then wrist arthroscopy. They found the MR arthrography to have a sensitivity of 74%, specificity of 80%, and accuracy of 79% in detecting a full-thickness TFCC tear. They caution that negative results of MR arthrography in patients with clinical suspicion of TFCC tear should be interpreted with caution.
Conservative Treatment
The treatment of acute TFCC injuries is initially conservative by immobilization of the wrist and DRUJ. The patient must be examined carefully to look for instability of the DRUJ or radiocarpal joint. Routine radiographs should be obtained to detect a fracture or subluxation of the distal ulna. If the radiographs are negative and instability is not present, then immobilization for 4 to 6 weeks is recommended to allow healing of the TFCC disruption. A peripheral tear would be expected to heal if the torn edges are held in close contact, owing to the good vascularity of the periphery of the TFCC. Many central tears also become asymptomatic with immobilization even though there is no significant vascularity to the central portion. Mikic26 examined the TFCC in 180 cadavers ranging in age from infant to 97 years old. He found no TFCC perforations in those wrists of individuals younger than 30 years of age. A linear progression of perforations with age was present over time such that all specimens in individuals over age 50 were found to have a TFCC perforation. This supports the concept that a defect in the central portion of the TFCC can occur without symptoms. It is those tears involving the ligamentous portion of the TFCC or those that heal with a flap of cartilage that impinges on the carpus or distal ulna that will clinically fail conservative treatment and require further treatment.
Surgical Treatment
Class 1A lesions are isolated stable central tears of the TFCC (Fig. 26-8). In patients with ulnar-neutral or ulnar-negative variance, who have failed conservative treatment, arthroscopic limited débridement of the central portion of the tear will give excellent relief of symptoms.27 The biomechanical effect of excision of the central portion of the TFCC has been examined.12,28,29 The excision of the central two thirds of the TFCC with maintenance of the dorsal and volar radioulnar ligaments as well as the ulnocarpal ligaments had no statistically significant effect on forearm axial load transmission (Fig. 26-9). The removal of more than two thirds will unload the ulnar column, shifting load to the distal radius and destabilizing the DRUJ.12 Adams further emphasized that the peripheral 2 mm of the TFCC must be maintained during central débridement to not have a biomechanical effect on load transfer.28
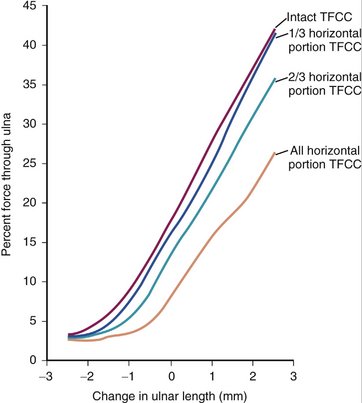
FIGURE 26-9 Biomechanical effect of central TFCC débridement on load transfer.
(Adapted from Palmer AK: The distal radioulnar joint: anatomy, biomechanics, and triangular fibrocartilage complex abnormalities. Hand Clin. 1987; 3:39.)
Arthroscopic débridement is performed by insertion of the arthroscope through the 3-4 portal to visualize the tear and by insertion of a small punch and shaver through the 6R portal to trim the tear (Fig. 26-10). The dorsal ulnar portion of the TFCC cannot be trimmed from the 6R portal using a punch. It can be trimmed using a small arthroscopic knife or the edge of an 18-gauge needle, raising a flap sufficient for the punch to trim. The alternative solution is to switch the scope to the 6R portal and use the punch through the 3-4 portal to accomplish the trimming of the ulnar portion of the tear.
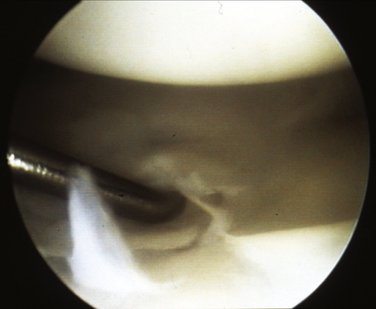
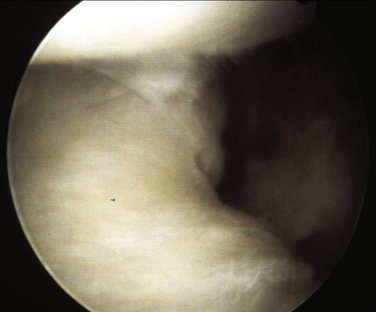
Class 1B lesions that are present in the chronic stage of more than 3 months after injury require arthroscopic evaluation. A peripheral tear that involves the dorsal radioulnar ligament can easily be repaired by arthroscopic means. This is performed by a two-needle technique similar to that employed for the repair of a knee meniscus. Initial arthroscopic evaluation may not show a discrete tear of the TFCC periphery. A probe placed through the 6R portal will demonstrate loss of the normal trampoline effect of the TFCC, indicating a peripheral tear and loss of mechanical function (Fig. 26-11). Synovitis and thin scar will be seen along the periphery of the TFCC at the location of the tear. A shaver will easily débride the synovium and scar to demonstrate the tear (Fig. 26-12). Adhesions will be present between the undersurface of the TFCC and the distal ulna. These must be released and the TFC mobilized sufficiently to allow advancement to reattach it and to restore proper tension. Failure to adequately débride and mobilize the chronic TFCC tear will prevent an adequate repair. After débridement, two hollow needles are passed across the tear percutaneously under arthroscopic vision (Fig. 26-13). A wire loop is passed through one needle to retrieve a 2-0 PDS suture, which is passed through the other needle. This allows the passage of a horizontal mattress-type suture across the tear. We prefer a horizontal type of suture for TFCC repair. Many other authors have reported good results using multiple simple vertical sutures placed at the periphery of the TFCC. As the suture is drawn tight it approximates the tear and restores tension to the TFCC. The suture can be tied under the skin, over the dorsal wrist capsule, or out of the skin over a bolster. The patient is immobilized in a long arm cast for 4 to 6 weeks before restarting rotational motion and suture removal. Those patients with a nonunited ulnar styloid fragment and instability of the DRUJ due to the disruption of the TFCC require open reattachment of the styloid fragment or excision of the fragment and reattachment of the TFCC to the remaining proximal ulna.

FIGURE 26-11 Probe on TFCC demonstrates absent trampoline effect indicating a peripheral TFCC detachment.
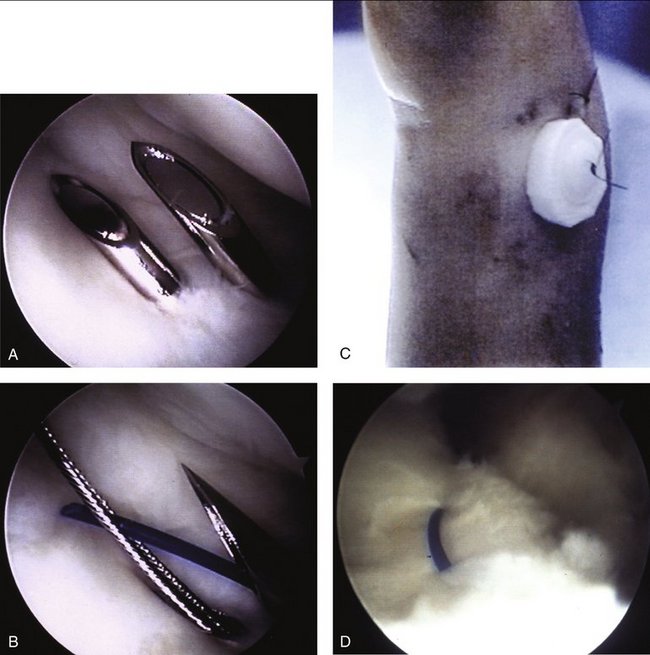
FIGURE 26-13 Arthroscopic repair of a Palmer class 1B peripheral TFCC tear. A, Two hollow needles passed across the tear. B, Wire loop in one needle used to pass 2-0 suture across tear. C, Suture tied over bolster. D, Suture approximates tear and restores tension to TFCC.
Class 1C lesions involve a disruption of the ulnocarpal ligament complex (Fig. 26-14). Those tears that do not heal with immobilization require operative repair to stabilize the ulnar carpus. Peripheral tears that involve the volar radioulnar ligaments or the ulnocarpal ligament complex can be repaired arthroscopically with limited open exposure to retract the ulnar nerve and artery (Fig. 26-15). The success rate for open repair is 80% to 85% good and excellent results.30,31
Class 1D lesions involve the radial detachment of the TFCC from the sigmoid notch of the distal radius. The treatment of these lesions remains controversial. There appears to be no vascularity to this portion of the TFCC. Theoretically, a reattached cartilage would not heal at this repair site. Clinical experience with open repair of these tears, however, has been good.31 This may be attributed to vascular ingrowth from the radial insertion site, which occurs with abrasion of the attachment site, stimulating the formation of new vessels. The tear needs to be assessed arthroscopically to determine its extent. If the radial tear includes disruption of one or both of the radioulnar ligaments, repair is required to prevent chronic instability of the DRUJ.
Short32 has described an arthroscopic technique for repair of class 1D lesions. The arthroscope is placed in the 3-4 portal. A bur is placed through the 6R portal to roughen the radial attachment of the TFCC. A 0.062-inch Kirschner wire is used to predrill two holes for the placement of the repair suture. The wires need to exit the radius on the radial side just volar to the first extensor compartment. An incision is made to retract the radial sensory nerve and the tendons of the first extensor compartment. A cannula is placed in the 6R portal through which a meniscal repair suture (suture with a long straight needle at each end) is passed through the radial aspect of the TFCC in a horizontal mattress fashion with each needle passing through the predrilled holes in the radius. The suture is tied over the radius.
Results
The results of arthroscopic repair of class 1B TFCC lesions are equivalent to those reported for open repair. Hermansdorfer and Kleinman30 reported the results of open repair in 11 patients, with 8 of 11 having complete pain relief and grip strength return to 87% of normal. Cooney and colleagues31 reported the results of open repair in 33 patients evaluated using the Mayo Modified Wrist Score. The average score was 83, with 11 excellent, 15 good, 6 fair, and 1 poor result. Bednar33 reported the results of arthroscopic repair of a class 1B lesion in 40 wrists assessed by the Mayo Modified Wrist Score. The average score was 86, with 11 excellent, 22 good, 6 fair, and 1 poor result.
Trumble and associates34 reported the results of arthroscopic repair in 24 wrists (9 1B, 2 1C, and 13 1D lesions). The average postoperative grip strength was 85%, with 89% excellent or good, 11% fair, and 0% poor results. Corso and coworkers35 reported the results of a multicenter study evaluating 45 wrists from three institutions: 27 of the 45 wrists had other associated injuries (4 with distal radial fracture, 7 with scapholunate ligament injury, 9 with lunatotriquetral ligament injury, 2 with ulnocarpal ligament injury, and 2 with radiocarpal ligament injury). All TFCC injuries were repaired arthroscopically. The patients were evaluated by the Mayo Modified Wrist Score with 29 excellent, 12 good, 1 fair, and 3 poor results.
The treatment of class 1B TFCC tears in an ulnar-positive patient is determined by history and arthroscopic findings. If the patient reports an acute injury in a previously asymptomatic wrist and arthroscopic evaluation demonstrates an acute peripheral tear with no arthroscopic findings of ulnar abutment (chronic central tear, osteochondral lesion on the ulnar aspect of the lunate), then an arthroscopic repair of the TFCC is performed. Note that the long ulna will decrease the available working space in the joint between the TFCC and the carpus, which will increase the technical difficulty of passing the repair suture. Bednar36 presented the results of arthroscopic repair of a class 1B lesion in an ulnar-positive wrist in 20 patients assessed by the Mayo Modified Wrist Score. The average score was 83, with 5 excellent, 9 good, 5 fair, and 1 poor result. The average grip strength was 73% of normal. If there is a history of ulnar abutment type symptom before acute tear and arthroscopic evaluation demonstrates evidence of ulnar abutment in addition to an acute TFCC injury, then, in addition to TFCC repair, ulnar shortening osteotomy is recommended. Trumble and associates37 reported the results of arthroscopic TFCC repair with ulnar-shortening osteotomy in 21 patients (9 1B, 2 1C, 10 1D lesions) with 90% pain relief and grip strengths of 81% of normal.
Short32 reported 79% excellent and good results in his series, with return of grip strength to 90% after an arthroscopic repair of a radial TFCC tear.
If the radial tear does not involve the radioulnar ligaments it is not destabilizing, and débridement of the central one to two thirds of the TFCC is recommended. Osterman38 reported a series of 19 patients with radial TFCC tears. All tears were chronic, and no patient had instability of the DRUJ. Ten patients were treated with arthroscopic débridement and 9 with arthroscopic repair. Eighty percent of the débridement group and 67% of the repair group were asymptomatic at follow-up. The data suggested that débridement of the radial TFCC tear was equally effective to repair in the patients with no instability.
1. Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg [Am]. 1989;14:594-606.
2. Palmer AK. Triangular fibrocartilage disorders: injury patterns and treatment. Arthroscopy. 1990;6:125-132.
3. Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist—anatomy and function. J Hand Surg [Am]. 1981;6:153-162.
4. Schuind F, An KN, Berglund L, et al. The distal radioulnar ligaments: a biomechanical study. J Hand Surg [Am]. 1991;16:1106-1114.
5. Chidgey LK. Histologic anatomy of the triangular fibrocartilage. Hand Clin; 2:1991; 249-262.
6. Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: its clinical significance. J Hand Surg [Am]. 1991;16:1101-1105.
7. Thiru-Pathi RG, Ferlic DC, Clayton ML. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surg [Am]. 1986;11:258-263.
8. Ekenstein FW, Palmer AK, Glisson RR. The load on the radius and ulna in different positions of the wrist and forearm. Acta Orthop Scand. 1984;55:363-365.
9. Palmer AK. The distal radioulnar joint. In: Taleisnik J, editor. Hand Clinics—Management of Wrist Problems. Philadelphia: WB Saunders; 1987:31-40.
10. Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and TFCC thickness. J Hand Surg [Am]. 1984;9:681-683.
11. Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res. 1984;187:26-34.
12. Palmer AK, Werner FW, Glisson RR, et al. Partial excision of the triangular fibrocartilage complex. J Hand Surg [Am]. 1988;13:391-394.
13. Palmer AK, Glisson RR, Werner FW. Ulnar variance determination. J Hand Surg [Am]. 1982;7:376-379.
14. Coleman HM. Injuries of the articular disc at the wrist. J Bone Joint Surg Br. 1960;42:552-559.
15. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-365.
16. Lindau T, Adlercreutz C, Aspenberg P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fracture. J Hand Surg [Am]. 2000;25:464-468.
17. Richards RS, Bennett JD, Roth JH, Milne K Jr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg [Am]. 1997;22(5):772-776.
18. Melone CPJr, Nathan R. Traumatic disruption of the triangular fibrocartilage complex: pathoanatomy. Clin Orthop Relat Res. 1992;275:65-73.
19. Golimbu CN, Firooznia H, Melone CPJr, et al. Tears of the triangular fibrocartilage of the wrist: MR imaging. Radiology. 1989;173:731-733.
20. Skahen JR, Palmer AK, Levinsohn EM, et al. Magnetic resonance imaging of the triangular fibrocartilage complex. J. Hand Surg [Am]. 1990;15:552-557.
21. Schweitzer ME, Brahme SK, Hodler J, et al. Chronic wrist pain: spin-echo and short tau inversion recovery MR imaging and conventional and MR arthrography. Radiology. 1992;182:205-211.
22. Zlatkin MB, Chao PC, Osterman AL, et al. Chronic wrist pain: evaluation with high-resolution MR imaging. Radiology. 1989;173:723-729.
23. Potter HG, Asnis-Ernberg L, Weiland AJ, et al. The utility of high-resolution magnetic resonance imaging in the evaluation of the triangular fibrocartilage complex of the wrist. J Bone Joint Surg [Am]. 1997;79:1675-1684.
24. Bednar JM, Bos M, Giacobetti F: Comparison of the accuracy of clinical exam and MRI in diagnosing TFCC lesions. Presented before the 52nd annual meeting of the American Society for Surgery of the Hand, Denver, CO, September 11, 1997.
25. Joshy S, Lee K, Deshmukh SC. Accuracy of direct magnetic resonance arthrography in the diagnosis of triangular fibrocartilage complex tears of the wrist. Int Orthop. 2008;32:251-253. Epub 2007; Jan 11
26. Mikic ZD. Age changes in the triangular fibrocartilage of the wrist joint. J Anat. 1978;126:367-384.
27. Osterman AL. Arthroscopic debridement of triangular fibrocartilage complex tears. Arthroscopy. 1990;6(2):120-124.
28. Adams BD. Partial excision of the triangular fibrocartilage complex articular disk: a biomechanical study. J Hand Surg [Am]. 1993;18:334-340.
29. Menon J, Wood VE, Schoene HR, et al. Isolated tears of the triangular fibrocartilage of the wrist: results of partial excision. J Hand Surg [Am]. 1984;9:527-530.
30. Hermansdorfer JD, Kleinman WB. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg [Am]. 1991;16:340-346.
31. Cooney WP, Linscheid RL, Dobyns JH. Triangular fibrocartilage tears. J Hand Surg [Am]. 1994;19:143-154.
32. Short WH. Arthroscopic repair of radial-sided triangular fibrocartilage complex tears. J Am Soc Surg of the Hand. 2001;1:258-266.
33. Bednar JM: Arthroscopic repair of peripheral tears of the triangular fibrocartilage complex. Presented before the American Academy of Orthopaedic Surgeons. Atlanta, GA, February 23, 1996.
34. Trumble TE, Gilbert M, Vedder N. Isolated tears of the triangular fibrocartilage: management by early arthroscopic repair. J Hand Surg [Am]. 1997;22:57-65.
35. Corso SJ, Savoie FH, Geissler WB, et al. Arthroscopic repair of peripheral avulsions of the triangular fibrocartilage complex of the wrist: a multicenter study. Arthroscopy. 1997;13:78-84.
36. Bednar JM: Arthroscopic TFCC repair in the ulna positive wrist. Presented before the International Federation of the Society of Surgery of the Hand, Vancouver, BC, Canada, May 25, 1998.
37. Trumble TE, Gilbert M, Vedder N. Ulnar shortening combined with arthroscopic repairs in the delayed management of triangular fibrocartilage complex tears. J Hand Surg [Am]. 1997;22:807-813.
38. Osterman AL: Radial triangular fibrocartilage tears: debride or repair? Presented at the ASSH/ASHT annual meeting, San Antonio, TX, September 23, 2005.