CHAPTER 47 Arthroscopic Treatment of Scapholunate Ligament Tears
Scapholunate interosseous ligament (SLIL) injuries are common causes of mechanical wrist pain. Despite an increased knowledge of carpal injuries and improvements in radiological evaluation, the diagnosis of a SLIL tear can be difficult or missed unless the evaluating physician has a high index of suspicion and an appropriate level of understanding of wrist anatomy and injury patterns. Usually a detailed history and physical examination and a series of plain radiographs are sufficient to make a diagnosis of SLIL injury (Fig. 47-1). Occasionally, advanced imaging techniques, such as magnetic resonance imaging (MRI) with or without intra-articular contrast enhancement, can be helpful in establishing a diagnosis and evaluating the wrist for associated injuries.1–3 MRI usually detects large, complete tears better than partial, smaller tears, however, particularly if the tear configuration is oblique to the imaging plane, or the tear is smaller than the distance between contiguous image slices.
After successful introduction in the knee and shoulder, arthroscopy gained popularity as a useful modality to diagnose and treat a wide spectrum of wrist pathology.4,5 This procedure has become the gold standard for diagnosis of SLIL injuries.6–8 Arthroscopy is a minimally invasive procedure allowing direct observation of intrinsic and extrinsic carpal ligaments and articular cartilage integrity under static and dynamic conditions. Comprehensive and accurate diagnosis and treatment of all carpal injuries can be done concurrently.
Because a delayed or missed diagnosis of an SLIL tear can lead to progressive carpal instability and predispose the patient to a predictable pattern of carpal arthritis called scapholunate advanced collapse (SLAC),9–11 we believe that wrist arthroscopy should be considered early during the evaluation and management of a patient with a suspected SLIL injury. It should be used selectively, however, for patients with significant symptoms, for patients with a mechanism of injury consistent with SLIL injury, and for patients in whom conservative treatment has failed or in whom acute operative management is indicated.
Anatomy of the Scapholunate Complex
The wrist is a complex structure comprising multiple small joint articulations with stability resulting from a complex linkage of intrinsic, intercarpal ligaments and extrinsic capsular ligaments. The wrist can be thought of as two separate rows with hand motion being the composite effect of motion between the radius, ulna, proximal carpal row (scaphoid, lunate, and triquetrum) and distal carpal row (scaphoid, trapezium, trapezoid, capitate, and hamate). The scaphoid is uniquely situated in both rows on an oblique axis to stabilize the carpus, while still permitting coordinated relative motion between the two rows and the radius and ulna. The scaphoid is stabilized by many ligaments, including the SLIL, radioscaphocapitate, scaphotrapeziotrapezoid, scaphocapitate, and dorsal intercarpal.12
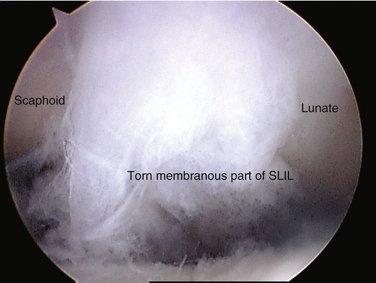
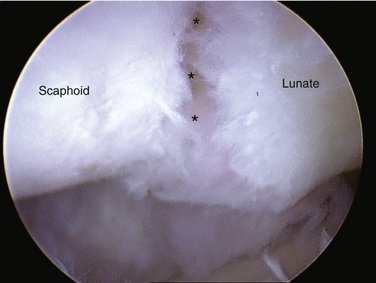
The SLIL is a C-shaped structure connecting the dorsal, proximal, and palmar surface between the scaphoid and the lunate, leaving the distal aspect of the joint bare of soft tissue allowing the evaluation of scapholunate articular congruity, preservation, and instability. This midcarpal visualization is essential in assessing the degree of instability between the two bones and in grading the spectrum of partial to complete injury.13 The dorsal and palmar portions of the SLIL are true ligamentous structures.14 The proximal portion is a membranous structure composed mainly of fibrocartilaginous tissue. In the absence of a tear, the transition between the dorsal and the proximal portion is not readily visualized during arthroscopy. Palpation of the SLIL with a probe permits differentiation, however, between the thick, taut dorsal ligament and the softer, thin proximal portion.
A partial SLIL tear may appear as a patulous, convex outpouching, rather than a confluent, barely discernible structure (Fig. 47-2). The probe may uncover a complete disruption of the insertion of the SLIL often from the lunate, which could not be perceived with observation alone. Partial tears may require palpation in the radiocarpal joint with a probe to appreciate the laxity and a thorough evaluation of the distal scapholunate joint articular surface congruity in the midcarpal joint to observe subtle incongruity or diastasis. A significant complete intrasubstance SLIL tear is readily visualized in the radiocarpal and the midcarpal joints.
Biomechanical and Kinematic Considerations
The three different portions of the SLIL have different biomechanical properties. The dorsal portion of the SLIL has a highest load at ultimate failure, followed by the palmar portion and then the proximal portion.15 Serial, sequential ligament sectioning studies in cadavers have shown that the SLIL is the primary ligament scapholunate stabilizer.16–21 No significant dissociation between the scaphoid and the lunate is shown, however, on static radiographs with an isolated, complete SLIL disruption.16,22 This is explained by the presence of secondary stabilizers of the scapholunate joint, which must be injured either acutely or chronically to show radiographic instability. Injury to the volar extrinsic (radiolunate and radioscaphocapitate),16,23 the distal intrinsic (scaphotrapezial),16,24 or the dorsal intercarpal ligaments and the SLIL is needed to visualize pathological carpal bone rotation radiographically.25
An isolated tear of the SLIL changes carpal loading and kinematics even without demonstrable radiographic abnormalities. Isolated loss of this major stabilizer of the carpus may lead to attenuation of the secondary supporting structures and progressive dissociation and rotation of the scaphoid and the lunate. With axial loading over time and without proximal restraint by the intact scapholunate joint, the capitate can descend proximally, further driving the scaphoid and lunate apart like a wedge. This results in midcarpal instability, loss of carpal height, and increased clinical symptoms as the bones increase their abnormal rotation. Changes in the radiocarpal, intercarpal, and midcarpal joint contact areas and loads in conjunction with the altered kinematics result in predictable SLAC arthritis. This process begins with radial styloid beaking and radial styloscaphoid joint narrowing (stage 1), then progresses proximally to alter the radioscaphoid facet proximal pole scaphoid articulation (stage 2), and finally progresses to the midcarpal capitolunate joint (stage 3).9
Treatment Options
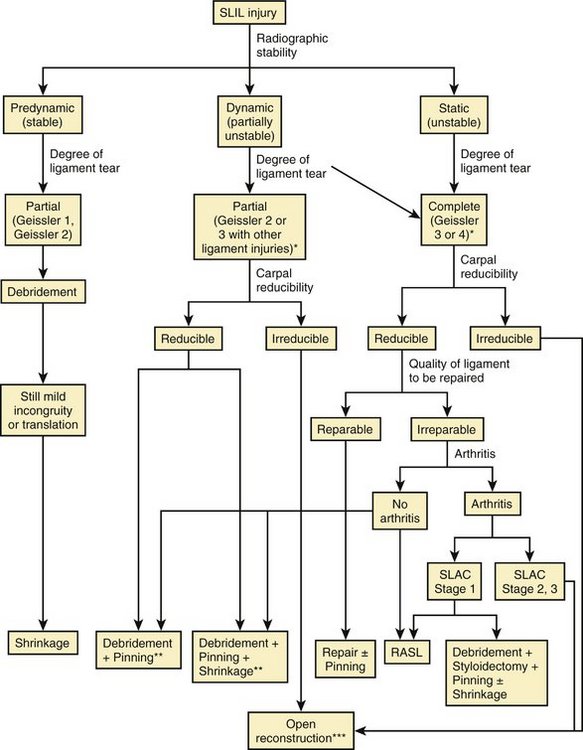
Several factors need to be considered in clinical decision making about an arthroscopic procedure, not only to diagnose, but also to treat symptomatic scapholunate injuries (Fig. 47-3). Acute repairable lesions have heretofore been treated with open suture repair or reattachment with bone anchors. Previous reports have sought to separate acute injuries from chronic by using an arbitrary and unproven 6 weeks as a cutoff, with the implied understanding that only acute injuries could be repaired. Because the patient history is often unreliable regarding the first subtle injury versus the most recent and now symptomatic injury, however, dates alone should not indicate irreparable ligaments. We believe all such presumed SLIL injuries should be evaluated arthroscopically to stage properly and treat all injured structures. Repair, if possible, is preferred. Arthroscopy also has the added advantages that it is real time, can include direct palpation of structures, and can assess the dynamic nature of the instability and its reducibility (neither of which can be known from even the best MRI study).
Arthroscopic assessment guides and rationalizes the potential for repair by confirming the degree of injury and the severity of instability.13 Arthroscopic treatment options include the following either in isolation or in combination: ligament débridement, ligament thermal shrinkage, transarticular Kirschner wire (K-wire) fixation, and radial styloidectomy (see Fig. 47-3).
Complete repairable tears in the senior author’s (M.P.R.) experience are best managed with open techniques. If the dorsal ligament has been avulsed from its attachment, it can and should be primarily repaired either with transosseous suture or with suture anchor. Depending on the amount of associated soft tissue injuries, this can be augmented with any of the numerous variations on dorsal capsulodesis.26–28
Standard Arthroscopic Technique
After successful cannula placement, the trocar is removed, and a 30-degree angled, 2.7-mm arthroscope is inserted. Distention of the radiocarpal space is maintained by a pressurized irrigation system through the cannula with outflow through a separately placed 18-gauge needle into the radiocarpal joint in the 1,2 portal or the ulnocarpal joint through the 6R or 6U portals. The 3,4, 4,5, 6U, 6R, midcarpal radial, and midcarpal ulnar portals are necessary to complete a thorough diagnostic evaluation and allow therapeutic procedures.
Arthroscopic Débridement
Indications
Arthroscopic débridement alone is indicated for acute or chronic partial, but stable tears of the volar or membranous portion of the ligament in a patient with mechanical symptoms (Fig. 47-4). These patients usually have focal reproducible mechanical wrist pain over the dorsal scapholunate joint worsened by activity and normal x-rays. It is common to treat these patients conservatively for several months with splints and activity modification. Persistent symptoms often lead to MRI; imaging rarely provides a definitive diagnosis and does not illuminate the treatment options. Arthroscopy in these patients typically reveals a stable Geissler grade 1 or 2 injury pattern with slight midcarpal incongruity and joint widening. Patients’ symptoms are due to tears in the substance of the ligament, which, although not destabilizing, create mechanical impingement during wrist motion causing focal dorsal wrist pain and occasionally leading to a synovitis and dorsal capsular thickening. Débridement of these SLIL flap tears in either the dorsal or the membranous portions and partial synovectomy often ameliorate symptoms.
Results
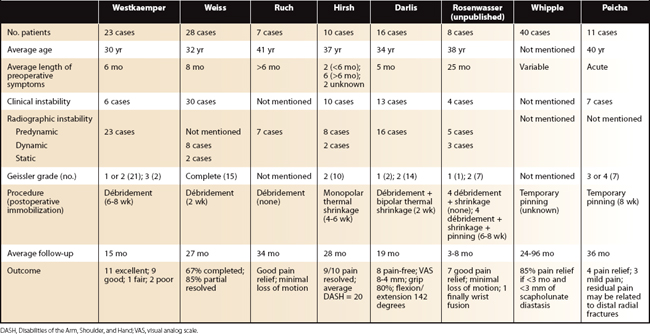
Isolated arthroscopic débridement has been reported in several small case series (Table 47-1).5,7,29 Most patients have predynamic or dynamic radiographic instability and Geissler grade 1 or 2 tears. Good pain relief, grip strength improvement, and maintenance of range of motion have been reported. The need for postoperative immobilization is unclear because some studies treated patients in a soft dressing with immediate motion, and some studies reported wrist immobilization for 6 to 8 weeks.
Radiofrequency Thermal Collagen Shrinkage
Technique
One study describes thermal stabilization using monopolar cautery (Oratec, Mountain View, CA) placed through the 4,5 portal.30 The probe is applied to the SLIL starting volarly and working dorsally until all the lax and redundant SLIL has been made taut. The authors recommend continuous irrigation with a safety limit on the probe set to 75°C to prevent chondral thermal injury. When midcarpal examination reveals the scapholunate joint congruency without gapping, the thermal shrinkage is complete. The authors believe postoperative immobilization for 4 to 6 weeks is crucial to allow ligament healing and to prevent recurrent laxity.
Another study uses a 2.3-mm bipolar probe (Vapr; Mitek, Westwood, MA), which is placed through the 4,5 portal.31 The probe was carefully applied to the torn rim of the volar portion of the ligament, the proximal membranous portion, and a small part of the dorsal ligament using multiple strokes similar to a paintbrush until visual color changes occurred. The probe was used intermittently, delivering energy for only a few seconds at a time to allow adequate outflow of warmed fluid. The tissue quality was palpated with a probe to confirm decreased laxity.
The senior author (M.P.R.) often applies the radiofrequency probe (Microblator 30 1.4 mm; Arthrocare, Sunnyvale, CA) to the proximal, membranous portion of the SLIL and the palmar midcarpal ligaments. In the midcarpal joint, the palmar ligamentous tissue at the junction of the scaphoid and lunate corresponds to the distal edge of the palmar SLIL and the radioscaphocapitate ligament (Fig. 47-5). Careful, limited, short bursts of thermal energy applied to this palmar midcarpal ligamentous and capsular tissue tightens the scapholunate and scapholunocapitate articulations. This midcarpal application of thermal collagen shrinkage can address proximal row intercarpal and midcarpal instability. Decreased gapping between the scaphoid and the lunate is readily observable. Manual reciprocal palmar-dorsal translation between the scaphoid and lunate before and after thermal shrinkage should be performed without traction to determine if there are any changes in stability after shrinkage. Without reduction of traction, a false increased sense of stability may be appreciated. Additionally, it should be more difficult to insert a probe in the midcarpal scapholunate interval.
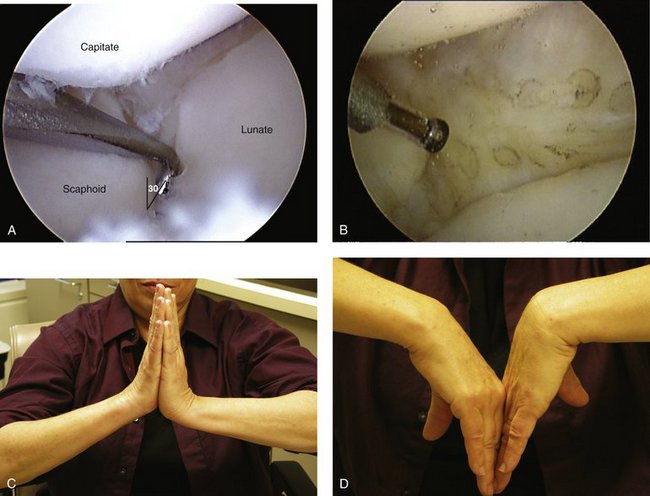
FIGURE 47-5 A, Midcarpal joint picture of the patient (from Figs. 47-1, 47-2, and 47-4) with a probe inserted into scapholunate joint and able to rotate greater than 30 degrees, indicating at least a Geissler grade 2 tear. B, After thermal capsular shrinkage of the palmar midcarpal ligaments, note the brown color change from A. C, Clinical follow-up of patient 4 months after débridement, thermal shrinkage, and temporary Kirschner wire fixation. Wrist extension of 52 degrees (right) and 80 degrees (left). D, Wrist flexion of 40 degrees (right) and 55 degrees (left).
Results
There are two published series of 10 and 16 patients treated with monopolar and bipolar electrothermal collagen shrinkage and postoperative immobilization ranging from 2 to 6 weeks (see Table 47-1).30,31 Complete pain relief ranged from 50% to 90% with preservation of wrist motion and no postoperative radiographic instability.
Arthroscopic-Assisted Temporary Transarticular Wire Placement
Technique
After the bones have been derotated, a percutaneous wire is placed across the scapholunate joint from radial to ulnar. Either 0.045-inch or 0.062-inch wires can be used. Pin insertion technique is crucial because the anatomical snuffbox contains the dorsal branch of the radial artery, the cephalic vein, and multiple sensory nerve branches with a narrow safe zone.32 Wires should be pushed through the skin and down to the scaphoid freehand. Then the wire driver is placed over the wire and turned on. By having the wire tip fixed to the bone before wire rotation by the driver, soft tissue injury is minimized. Several divergent pins can be placed across the scapholunate and scaphocapitate joint in this manner. This is the best way to maintain the reduction of the scapholunate diastasis achieved through derotation.
Results
Two case series have been reported on patients who underwent arthroscopic reduction of the scapholunate joint and temporary transarticular scapholunate joint fixation for isolated SLIL injury or associated with a distal radius fracture (see Table 47-1).33,34 These types of injuries are very different and do not act the same way clinically over long-term follow-up. Acute injuries recognized and treated after trauma have more predictable outcomes, in contradistinction to chronic injuries with a vague history of significant antecedent trauma; this correlates with the quality of the tissue at the ligamentocapsular injury site and its capacity to heal.
Arthroscopic Débridement, with or without Thermal Shrinkage, with or without Temporary Transarticular Pinning
Contraindications
This procedure is contraindicated and inadequate for patients with static carpal malalignment. Static carpal malalignment corresponds to chronicity, and that translates to a lack of adequate residual ligament as scaffolding that could foster repair and provide stability and improved carpal kinematics. These patients require supplemental tissue grafting using open or closed techniques, such as various capsulodeses and ligament reconstruction with tendon grafts or bone-ligament-bone constructs or salvage procedures that restrict carpal motion and maintain reduction through limited intercarpal fusions, such as scaphotrapeziotrapezoid. Simple débridement and Kirschner pinning for these static instabilities routinely fail to maintain the correction of carpal alignment achieved at surgery.26,35,36
Results
To date, there are no published reports detailing the outcomes of patients treated with this protocol. This communication is the opinion of the senior author (M.P.R.), who has performed thermal ligament shrinkage in eight patients with follow-up to an early clinical result. The average age of patients was 38.3 years (range 21 to 54 years) (personal communication) (see Table 47-1), and all met the clinical and radiographic inclusion criteria discussed previously. Procedures included ligament débridement (eight), scaphocapitate (four) and scapholunate (four) transarticular pinning (0.045-inch K-wire), dorsal ganglionectomy (one), débridement of the triangular fibrocartilage complex (two), and posterior interosseous neurectomy (one). Predynamic and dynamic radiographic instability was observed in five (predynamic) and three (dynamic) patients. The proximal scapholunate ligament was thermally shrunk in all patients, and the midcarpal palmar ligaments were shrunk in four patients.
Reduction and Association of the Scaphoid and Lunate
The RASL procedure was developed as an open reconstructive procedure to reassociate the scapholunate joint and foster a fibrous neoligament by dechondrification of the interface and maintaining the reduction through healing with a headless bone screw, which is placed transarticularly by the senior author (M.P.R.). The procedure can be and is being done arthroscopically, and although the follow-up time is shorter, the results are similar.38–40
Indications
The premise of RASL technique is that it is important to maintain the obligatory intercarpal scapholunate rotation, while still controlling the aberrant scaphoid flexion and lunate extension by relinking the joints without fusing them. The crucial elements of a successful RASL procedure are the dechondrification of the opposing surfaces of the scaphoid and lunate; the anatomical reduction of the scaphoid, lunate, and capitate; and the maintenance of this normal carpal alignment during the reparative phase in which the formation of a fibrous neoligament between the scaphoid and the lunate occurs. The planned retention of a headless bone screw (Fig. 47-6) augments and protects the fibrous neoligament, while undergoing an expected lucency around the lunate screw threads as it permits near-physiological motion between the scaphoid and the lunate. This concept has been confirmed by a cadaver biomechanical study in which scapholunate motion after the RASL procedure was found to be preserved within 5 degrees of the preinjury state for all positions of wrist motion.41
Technique
The scapholunate joint is anatomically reduced by derotation reciprocally by performing flexion of the lunate and extension of the scaphoid using the wire joysticks. This also results in reduction of the capitolunate joint, which is anatomical when the cartilage of the capitate proximal pole is no longer visualized. A Kocher clamp is placed on the reduced K-wires to maintain the reduction, which is confirmed fluoroscopically and visually. Then the wire for the cannulated Headless Bone Screw (Hand Innovations, Miami, FL) is inserted through the radial incision just proximal to the scaphoid waist toward the lunate vertex. The wire should pass through the center of the scaphoid and lunate in the coronal and the sagittal planes to establish an isometric rotation point, which nearly restores carpal kinematics. The depth should be measured so that the screw can be countersunk slightly within the scaphoid. The screw is advanced, and fluoroscopy is used to confirm appropriate screw position and length. The K-wires all are removed. Interrupted absorbable sutures are used to close the radial capsule. The first dorsal retinaculum is closed over the relocated tendons. The dorsal wrist capsule is carefully repaired without imbrication, and no capsulodesis is performed to limit motion. The extensor pollicis longus remains transposed from its sheath.
Conclusion
Scapholunate ligament injuries are common, but they are often difficult to diagnose with many overlapping and confounding conditions. Inadequate treatment can lead to progressive instability because of changes in associated intrinsic and extrinsic ligaments. Arthroscopy plays a major role in staging the degree of chondral and ligamentous injuries and indicating treatment. Various arthroscopic procedures can be performed alone or in combination based on radiographic instability, location, and extent of the ligament injuries. These arthroscopic techniques include débridement, thermal capsuloligamentous shrinkage, transarticular wire placement, styloidectomy, and the RASL procedure. Increasingly severe static deformity resistant to reduction via the arthroscope should be repaired with an open procedure. Advanced arthritis should be treated with accepted salvage procedures.
1 Morley J, Bidwell J, Bransby-Zachary M. A comparison of the findings of wrist arthroscopy and magnetic resonance imaging in the investigation of wrist pain. J Hand Surg [Br]. 2001;26:544-546.
2 Haims AH, Schweitzer ME, Morrison WB, et al. Internal derangement of the wrist: indirect MR arthrography versus unenhanced MR imaging. Radiology. 2003;227:701-707.
3 Schmitt R, Christopoulos G, Meier R, et al. Direct MR arthrography of the wrist in comparison with arthroscopy: a prospective study on 125 patients. ROFO. 2003;175:911-919.
4 Rettig ME, Amadio PC. Wrist arthroscopy: indications and clinical applications. J Hand Surg [Br]. 1994;19:774-777.
5 Ruch DS, Poehling GG. Arthroscopic management of partial scapholunate and lunotriquetral injuries of the wrist. J Hand Surg [Am]. 1996;21:412-417.
6 Dautel G, Goudot B, Merle M. Arthroscopic diagnosis of scapho-lunate instability in the absence of x-ray abnormalities. J Hand Surg [Br]. 1993;18:213-218.
7 Westkaemper JG, Mitsionis G, Giannakopoulos PN, et al. Wrist arthroscopy for the treatment of ligament and triangular fibrocartilage complex injuries. Arthroscopy. 1998;14:479-483.
8 Sennwald G. Diagnostic arthroscopy: indications and interpretation of findings. J Hand Surg [Br]. 2001;26:241-246.
9 Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg [Am]. 1984;9:358-365.
10 Watson HK, Weinzweig J, Zeppieri J. The natural progression of scaphoid instability. Hand Clin. 1997;13:39-49.
11 Taleisnik J. Current concepts review: carpal instability. J Bone Joint Surg Am. 1988;70:1262-1268.
12 Berger RA. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop. 2001;383:32-40.
13 Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg [Am]. 1996;78:357-365.
14 Berger RA. The gross and histologic anatomy of the scapholunate interosseous ligament. J Hand Surg [Am]. 1996;21:170-178.
15 Berger RA, Imeada T, Berglund L, et al. Constraint and material properties of the subregions of the scapholunate interosseous ligament. J Hand Surg [Am]. 1999;24:953-962.
16 Short WH, Werner FW, Green JK, et al. Biomechanical evaluation of ligamentous stabilizers of the scaphoid and lunate. J Hand Surg [Am]. 2002;27:991-1002.
17 Burgess RC. The effect of rotatory subluxation of the scaphoid on radio-scaphoid contact. J Hand Surg [Am]. 1987;12:771-774.
18 Ruch DS, Smith BP. Arthroscopic and open management of dynamic scaphoid instability. Orthop Clin North Am. 2001;32:233-240.
19 Short WH, Werner FW, Green JK, et al. The effect of sectioning the dorsal radiocarpal ligament and insertion of a pressure sensor into the radiocarpal joint on scaphoid and lunate kinematics. J Hand Surg [Am]. 2002;27:68-76.
20 Meade TD, Schneider LH, Cherry K. Radiographic analysis of selective ligament sectioning at the carpal scaphoid: a cadaver study. J Hand Surg [Am]. 1990;15:855-862.
21 Blevens AD, Light TR, Jablonsky WS, et al. Radiocarpal articular contact characteristics with scaphoid instability. J Hand Surg [Am]. 1989;14:781-790.
22 Berger RA, Blair WF, Crowninshield RD, et al. The scapholunate ligament. J Hand Surg [Am]. 1982;7:87-91.
23 Ruby LK, An KN, Linscheid RL, et al. The effect of scapholunate ligament section on scapholunate motion. J Hand Surg [Am]. 1987;12:767-771.
24 Boabighi A, Kuhlmann JN, Kenesi C. The distal ligamentous complex of the scaphoid and the scapho-lunate ligament: an anatomic, histological and biomechanical study. J Hand Surg [Br]. 1993;18:65-69.
25 Mitsuyasu H, Patterson RM, Shah MA, et al. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg [Am]. 2004;29:279-288.
26 Szabo RM, Slater RRJr, Palumbo CF, et al. Dorsal intercarpal ligament capsulodesis for chronic, static scapholunate dissociation: clinical results. J Hand Surg [Am]. 2002;27:978-984.
27 Wintman BI, Gelberman RH, Katz JN. Dynamic scapholunate instability: results of operative treatment with dorsal capsulodesis. J Hand Surg [Am]. 1995;20:971-979.
28 Lavernia CJ, Cohen MS, Taleisnik J. Treatment of scapholunate dissociation by ligamentous repair and capsulodesis. J Hand Surg [Am]. 1992;17:354-359.
29 Weiss AP, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg [Am]. 1997;22:344-349.
30 Hirsh L, Sodha S, Bozentka D, et al. Arthroscopic electrothermal collagen shrinkage for symptomatic laxity of the scapholunate interosseous ligament. J Hand Surg [Br]. 2005;30:643-647.
31 Darlis NA, Weiser RW, Sotereanos DG. Partial scapholunate ligament injuries treated with arthroscopic debridement and thermal shrinkage. J Hand Surg [Am]. 2005;30:908-914.
32 Steinberg BD, Plancher KD, Idler RS. Percutaneous Kirschner wire fixation through the snuff box: an anatomic study. J Hand Surg [Am]. 1995;20:57-62.
33 Whipple TL. The role of arthroscopy in the treatment of scapholunate instability. Hand Clin. 1995;11:37-40.
34 Peicha G, Seibert F, Fellinger M, et al. Midterm results of arthroscopic treatment of scapholunate ligament lesions associated with intra-articular distal radius fractures. Knee Surg Sports Traumatol Arthrosc. 1999;7:327-333.
35 Wyrick JD, Youse BD, Kiefhaber TR. Scapholunate ligament repair and capsulodesis for the treatment of static scapholunate dissociation. J Hand Surg [Br]. 1998;23:776-780.
36 Muermans S, De Smet L, Van Ransbeeck H. Blatt dorsal capsulodesis for scapholunate instability. Acta Orthop Belg. 1999;65:434-439.
37 Yao J, Osterman AL. Arthroscopic techniques for wrist arthritis (radial styloidectomy and proximal pole hamate excisions). Hand Clin. 2005;21:519-526.
38 Lipton CB, Ugwonali OF, Sarwahi V, et al. Reduction and association of the scaphoid and lunate for scapholunate ligament injuries (RASL). Atlas Hand Clin. 2003;8:249-260.
39 Rosenwasser MP, Miyasaka KC, Strauch RJ. The RASL procedure: reduction and association of the scaphoid and lunate using the Herbert screw. Tech Hand Upper Extrem Surg. 1997;1:263-272.
40 Lipton C, Ugwonali O, Sarwahi V, et al. The treatment of chronic scapholunate dissociation with reduction and association of the scaphoid and lunate (RASL). Atlas Hand Clin. 2003;8:95-105.
41 Amin F, Gardner TR, Ko BH, et al: The RASL procedure (reduction and association of the scaphoid and lunate using the Herbert screw): an evaluation of inter-carpal kinematics in cadaveric wrists. Presented at the American Association for Hand Surgery Meeting, Tucson, AZ, January 2006.