CHAPTER 13 Arthroscopic Labral Debridement
Basic science and rationale for treatment
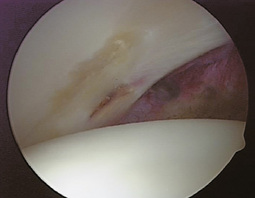
Microvascular studies have confirmed that the vascular supply of the acetabular labrum comes via the obturator artery, the superior gluteal artery, and the inferior gluteal artery, which are the same vessels that supply the bony structure of the acetabulum. These studies also showed no evidence of the penetration of vessels from the underlying acetabular bone into the labral substance. Labral tears most frequently occur on the articular nonvascular white zone, and they will not heal with conservative treatment. These tears are often delaminating tears that are not amenable to suture repair (Figure 13-1).
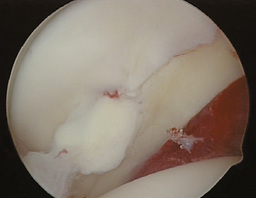
Labral tears are most frequently seen in the anterior acetabular quadrant (more than 90% in most series), and they are common in patients with degenerative hip disease or acetabular dysplasia. A common finding even with mild acetabular dysplasia is hypertrophy of the anterior labrum, which makes this area more susceptible to tearing. Because of the avascularity and degenerative nature of these lesions, they too are usually not amenable to suture repair (Figure 13-2). Posterior labral tears are most frequently seen after a posterior hip dislocation. Lateral tears are usually associated with additional labral and acetabular lesions.
Outcomes
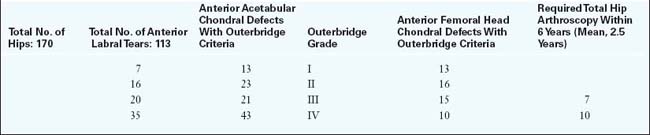
Surgical outcomes are directly dependent on the extent of articular surface involvement. More than 90% of patients will have an excellent result if the labral tear is addressed and if the femoral and acetabular chondral surfaces are intact. If there is a grade I or II chondral lesion of either the adjacent acetabular chondral surface or the femoral head, 70% to 80% will have a good to excellent result. Conversely, if the articular cartilage involvement is full thickness and diffuse on the femoral head and the acetabulum, 70% to 80% of cases are associated with a poor result during follow up, and 40% to 50% will require total joint arthroplasty within 2 years of arthroscopy. Table 13-1 shows arthroscopic results at 2 to 5 years of follow up for 170 patients with hips with mild to moderate dysplasia.
Glick J.M. Hip arthroscopy using the lateral approach. Instr Course Lect.. 1988;37:223-231.
McCarthy J., Noble P., Aluisio F.V., Schuck M., Wright J., Lee J.R.N. Anatomy, pathologic features, and treatment of acetabular labral tears. Clin Orth Rel Res.. 2003;406(1):38-47.
McCarthy J.C., Lee J. Hip arthroscopy: indications and technical pearls. Clin Orthop Relat Res.. 2005;441:180-187.
McCarthy J.C., Lee J.A. Acetabular dysplasia: a paradigm of arthroscopic examination of chondral injuries. Clin Orthop.. 2002:122-128.
McCarthy J.C., Lee J.A. Hip arthroscopy: indications, outcomes, and complications. Instr Course Lect.. 2006;55:301-308.
McCarthy J.C., Noble P.C., Schuck M.R., Wright J., Lee J. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop.. 2001:25-37.
Sampson T.G. Complications of hip arthroscopy. Clin Sports Med.. 2001;20(4):831-835.