CHAPTER 19 Arthroscopic Femoral Osteoplasty
Introduction
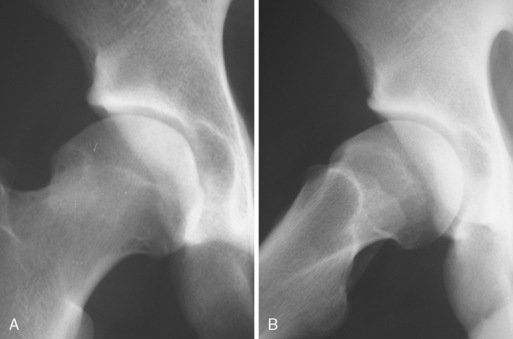
In 1995, Ganz first described femoroacetabular impingement (FAI), and, in 1999, it was introduced into the English literature. Although the first case was pincer impingement as a result of acetabular overcoverage after a periacetabular osteotomy, further investigations by Professor Ganz and his group led to the recognition of a second type of impingement: cam impingement. This type of impingement is the result of loss of the femoral head–neck offset, which causes the joint to function like a mechanical cam device. The anatomy of cam impingement has been previously described as a pistol grip deformity or a tilt deformity (Figure 19-1). Many investigators have attributed this anatomy to subclinical slipped capital femoral epiphysis (SCFE), and certainly the residuals of an unreduced SCFE can result in cam impingement. Beaule and colleagues demonstrated in a computed-tomography–based study that cam impingement can occur without SCFE, which suggests that this condition is not the result of a subclinical SCFE. Wagner and colleagues demonstrated that the bone of the cam lesion is not reactive nor does it involve any inflammation; thus it is not likely the result of the impingement or arthritis. Because the deformity occurs at or near the femoral head physeal scar, it may be genetically predetermined or the result of stresses applied during development. Either way, this pistol grip deformity has been associated with premature osteoarthritis of the hip. It has also been suggested that cam impingement results in premature or idiopathic arthritis of the hip. However, Bardakos and Villar have shown that only two thirds of patients with cam impingement show radiographic progression of arthritis at 10-year follow up.
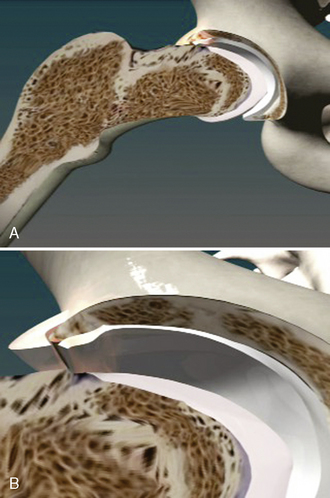
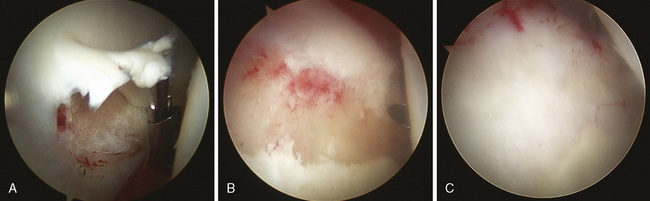
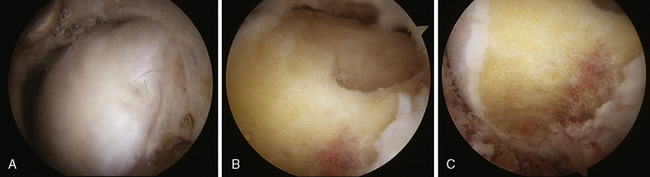
The anatomy of cam impingement can frequently be seen among those patients with idiopathic arthritis, although this is still a controversial subject. The suggestion that impingement results in hip arthritis is also likely when studying the pathologic findings of symptomatic impingement patients without arthritis, particularly of those with labral tears and chondral lesions that are thought to progress to arthritis when untreated. The majority of patients in Ganz’s series had a combination of cam and pincer impingement, which has been confirmed in other published series as well as my own experience of several hundred patients with symptomatic FAI. Beck and colleagues found that the demographics and pathology do correlate with the different subtypes of impingements. Particularly, for those with isolated types of impingements, the cam type is the most common (17%). It tends to occur in 19-year-old males, whereas those with isolated pincer impingement are 40-year-old active females. For those with isolated cam impingement, the common pathologic findings initially are focal, deep chondral delamination lesions (anterolaterally and extending about 1 cm from the acetabular edge) (Figure 19-2). At first the labrum is intact, but it eventually separates from the acetabular articular cartilage edge before degenerating. The labrum often separates from the acetabulum and the articular cartilage, and the articular cartilage delaminates from the bony acetabulum (Figure 19-3). Alternatively, those with pincer impingement tend to have intrasubstance crushing of the labrum, and the articular cartilage damage extends only a couple of millimeters from the acetabular edge (Figure 19-4). Although the greatest depth of penetration of articular cartilage damage in pincer impingement is also anterolateral, the damage tends to be more global and to extend around the circumference of the acetabulum. In addition, there is often posterior acetabular (62%) and femoral head (31%) articular cartilage damage as a result of the contrecoup phenomenon of the femoral head levering against the anterior acetabulum as the patient tries to obtain hip motion, which results in shearing forces posteriorly (see Figure 19-4). It has been my experience that one type of impingement will predominate the intra-articular pathologic findings.
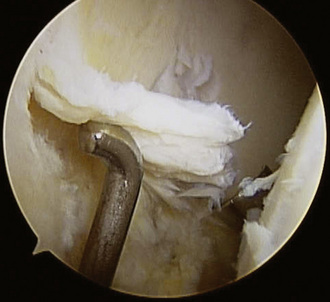
Figure 19–2 Arthroscopic view of the chondral delamination of the acetabulum associated with cam impingement.
Indications
Although some believe that FAI results in arthritis and thus that surgery should be performed to prevent the arthritis, that has not been the approach used in our practice, because there is no evidence at this point that arthritis can be prevented. I certainly believe that having the anatomy of impingement does put the patient at risk for chondral injury, labral injury, and, potentially, arthritis. However, on the basis of my experience with patients who are more than 60 to 70 years old with the anatomy of FAI but no evidence of arthritis or hip symptoms in combination with my extensive experience of cadaveric research involving specimens 80 to 90 years old with the anatomy of obvious cam and combined impingement without evidence of arthritis, I have concluded that not everyone with the anatomy of FAI will develop osteoarthritis (Figure 19-5). It is my belief that the anatomy of FAI does put patients at potential risk for joint damage. However, it likely requires the individual to be involved in activities that require greater hip range of motion with or without pivoting (e.g., martial arts, soccer, running, golf) to result in impingement. After the tissues start breaking down, patients develop symptoms, because the labrum is a structure that is richly innervated. It is as soon as patients have confirmed intra-articular pain that surgery is indicated. Intra-articular anesthetic guided by fluoroscopy or ultrasound and that is given by itself or with contrast when performing magnetic resonance arthrography is a useful diagnostic test to confirm that the joint is the source of pain. Thus, the goal of surgery is to relieve intra-articular hip pain that is the result of impingement.
History and physical examination
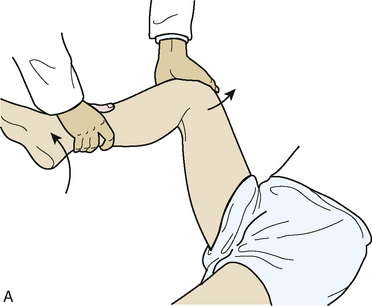
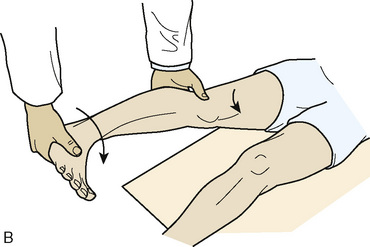
Although a complete discussion of the evaluation of the hip is beyond the scope of this chapter, a brief discussion of the general concepts is appropriate. First, evaluation includes the inspection of the gait and of the skin around the hip. Patients are assessed for hip weakness and tightness with the use of the Trendelenburg and Ober tests. Hip range of motion is assessed while the patient is supine. Evaluation of hip adduction and abduction, as well as internal and external rotation, should be performed in hip flexion and extension. Also, hip motions evaluated include flexion, extension, and flexion contracture. There is usually limited hip internal rotation, particularly when the hip is in flexion, among patients with impingement. Furthermore, patients frequently have pain when the hip is flexed to 90 degrees, adducted, and internally rotated; this is known as the impingement test (Figure 19-6). The labral stress test and the resisted straight-leg raise are tests that commonly result in hip pain among patients with labral tears and symptomatic impingement (Figure 19-7). These tests are often positive among patients with both cam and pincer types of FAI, and they may also be positive among patients with other sources of intra-articular hip pain.
Imaging and diagnostic tests
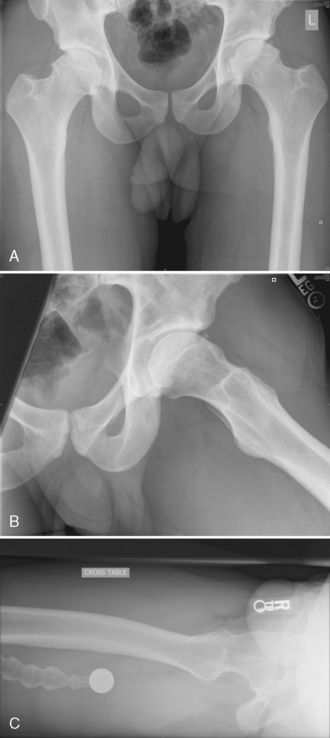
Plain radiographs are extremely valuable for the assessment of patients with hip pain that is the result of hip impingement. The standard imaging series for patients with hip pain includes an anteroposterior pelvic view with the coccyx centered 1 cm to 3 cm above the pubic symphysis and a true cross-table lateral radiograph (Figure 19-8). A frog-leg lateral view will demonstrate a lateral projection of the proximal femur and thus can be used for cam impingement assessment; however, this is not a lateral view of the acetabulum, so it has limited usefulness (see Figure 19-8, B). A cross-table lateral view, a Dunn view, and a modified Dunn view are true lateral views of the hip that can provide more information about the acetabulum (see Figure 19-8, C). The femoral head is generally symmetric, particularly the head–neck offset. A loss of the sphericity of the femoral head–neck region may be consistent with cam impingement (see Figure 19-8, A through C). This can be seen as a flattening of the concave surface of the lateral femoral neck and the appearance that the femoral head is not centered over the femoral neck. Leunig and colleagues demonstrated that, for patients with hip dysplasia, the apex of the femoral head is approximately 1 cm beyond the low point of the femoral neck, whereas in patients with impingement this distance was only 3 mm. In some situations, there may be a bump on the anterolateral surface of the femoral neck that may project beyond the femoral head or have a sharp transition or even a hook appearance at the head–neck junction. The alpha angle was originally described by Notzli and colleagues to quantify the head–neck offset on radially generated axial magnetic resonance imaging cuts of the femoral neck and head. These authors demonstrated that, in their normal population, the alpha angle averaged 42 degrees, whereas in those patients with impingement, this angle averaged 74 degrees. Most surgeons use 50 degrees or 55 degrees as their cutoff point for defining cam impingement. This angle has also been used when evaluating plain radiographs and computed tomography scans, although it has not been validated for these modalities. Additional plain radiographs may demonstrate a short femoral neck or a femoral neck–shaft angle that is varus, which may result in cam-type impingement. Untreated or residual deformity from SCFE or Legg-Calvé-Perthes disease may be seen on plain films, and this may result in cam impingement. Pincer impingement may also be seen on plain radiographs in association with coxa profunda, protrusio, retroversion, or relative retroversion of the superior acetabulum and arthritic changes.
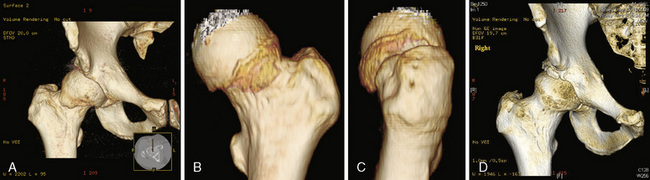
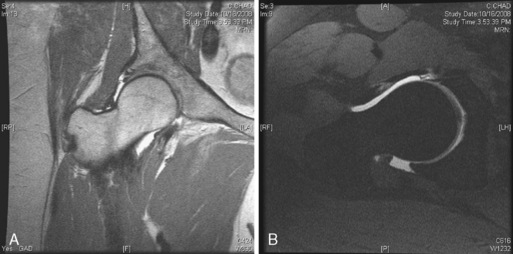
Computed tomography scans, particularly three-dimensional ones, are particularly useful for demonstrating the bony anatomy associated with cam impingement (Figure 19-9). Magnetic resonance imaging, particularly magnetic resonance arthrography, is beneficial for demonstrating the cam lesion by allowing for a way to measure the alpha angle and to demonstrate labral tears, edema, or cysts within the femoral neck (these are often seen with impingement); this type of imaging can occasionally demonstrate chondral lesions (Figure 19-10). Local anesthetic is usually introduced with the contrast used for magnetic resonance arthrography to determine whether the pain is temporarily relieved within the joint, which confirms the source of pain as being intra-articular.
Surgical technique
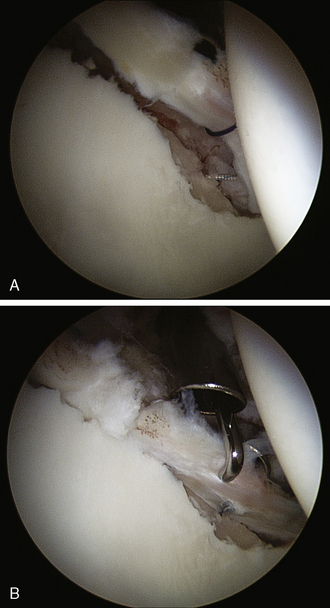
The goals of surgery are to relieve the abutment between the femoral head–neck junction and the acetabular rim and to treat the associated pathology (i.e., labral tears and chondral lesions; Figure 19-11, A through D). Although this may be done with the patient in the supine or lateral position, my preference is the supine position, which is described in Chapter 9 of this book.
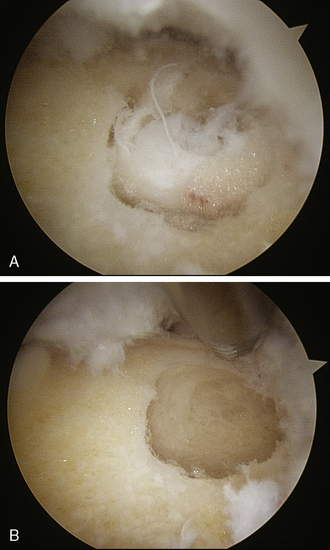
Chondral flaps are removed, and chondral defects and lesions are debrided to a stable edge. If the lesion is sufficiently large enough, a microfracture is performed (Figure 19-12, A through C). Our experience has been that femoral head chondral lesions do not do as well postoperatively as acetabular lesions do. However, when there are chondral lesions of the acetabular articular surface, the results of hip arthroscopy in general, including FAI surgery, are also less predictable as compared with patients in whom the articular cartilage is intact.
Labral tears are addressed next. If the labrum is intact and there is combined impingement, then an anterior portal at the junction of the anterosuperior iliac spine and the greater trochanter is made. An arthroscopic knife is then introduced to detach the labrum at the site of acetabular overcoverage or pincer impingement. A traction suture may be used to retract the detached labrum. The acetabuloplasty may then be performed with the use of a motorized burr. After other pathology has been addressed—including synovectomy, chondroplasty, and microfracture—the labrum is reattached with the use of suture anchors (Figure 19-13). If there is a labrochondral separation, which occurs more commonly with cam impingement, and if the labrum has minimal or no obvious intrasubstance damage, then this may be repaired with the use of suture anchors. Healing occurs from the acetabular bony blood supply and capsule. If there is significant intrasubstance damage and tearing of the labrum, then a partial labrectomy is carried out; there is limited blood supply within the labrum, and, as a result, the capacity to heal is limited. Partial labrectomy may be performed with the use of meniscal-type biters, shavers, or radiofrequency devices.
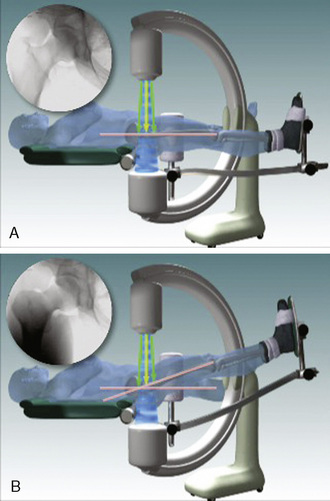
Although many surgeons prefer to perform peripheral compartment arthroscopy with the hip flexed 20 degrees to 45 degrees to further relax the anterior capsule, I prefer to perform cam surgery decompression with the hip in neutral flexion and extension. When the extremity is in neutral flexion and extension, it is easier to get a truer fluoroscopic image, because the fluoroscope beam can be made perpendicular to the axis of the femur (Figure 19-14). Because fluoroscopy beams diverge, there is inherent distortion, which would be magnified if the central fluoroscopic beam is not perpendicular to the proximal femur; this may result in inadequate or excessive bony resection. While there are benefits to peripheral compartment arthroscopy in the neutral flexion-extension position, the trade-off, which the author accepts, is that it is necessary to perform a partial capsulectomy of the anterolateral capsule to allow for adequate visualization.
To perform peripheral compartment arthroscopy with the patient in the neutral flexion and extension position, the standard anterolateral portal is used along with a proximal anterolateral portal that is 3 cm to 4 cm proximal to the standard anterolateral portal (Figure 19-15). The blunt trocar and the sheath for the arthroscopic camera are introduced via the anterolateral portal to the apex of the femoral head–neck deformity. The trochar is exchanged for the arthroscope within the cannula. The scope and cannula are maintained on the capsule and bone at the apex of the cam deformity. Next, the arthroscopic motorized shaver is introduced through the proximal anterolateral portal. With the use of triangulation, the shaver is brought to the tip of the camera in its sheath (Figure 19-16). At this point, the camera and the shaver are lying on the capsule directly over the apex of the bony deformity laterally; this is seen on the fluoroscopic monitor, which is projecting an anteroposterior view of the hip (see Figure 19-16). The shaver then is used to clear some of the soft tissue over the capsule. The shaver tip soon becomes visible, and the shaver is used to make a capsulotomy of the anterolateral capsule. This is enlarged as a partial capsulectomy to a size of 1 cm to 1.5 cm in diameter (Figure 19-17). This is generally performed with the use of a 30-degree arthroscopic lens and a 5.0-mm aggressive shaver, with the fluoroscopic monitor used for guidance. A radiofrequency device may also be used to perform the partial capsulectomy. Glick has shown that larger capsulectomies of the anterolateral capsule are safe and not associated with hip instability. Furthermore, he has shown that this capsule ultimately heals.

Figure 19–16 Fluoroscopic image of the trocar in the anterolateral portal and the shaver at the location of the maximal deformity.
After the partial capsulectomy is completed, the shaver is introduced into the peripheral compartment. A partial synovectomy is performed to allow for the adequate visualization of the anterior, lateral, and posterior femoral head, with its cam deformity; the extra-articular acetabular rim; the labrum; and the capsular reflection on the acetabulum, in addition to many other peripheral compartment structures (see Figure 19-17). The lateral synovial fold with its retinacular vessels is also visualized, as is the medial synovial fold and the zona orbicularis. The hip can be flexed, adducted, and rotated to demonstrate the impingement arthroscopically, either with the traction boot attached to the fracture table or by removing it from the traction device.
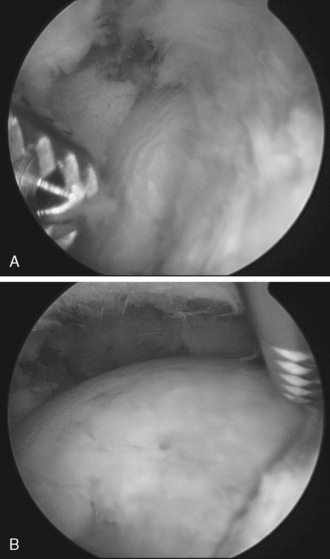
With the use of a motorized burr, the femoral head–neck offset is restored when the surgeon removes the excessive bone. Not all cam impingement patients have the same anatomy, because the bumps differ: some may be lateral, some may be anterior, and most are anterolateral. Thus, the same operation (i.e., the location and amount of bone removed) is not performed on every patient. The surgery must be tailored to the patient’s pathology. The goal is to restore the normal anatomy and offset for the patient (Figure 19-18). Bony resection and visualization may be enhanced by exchanging the scope with the shaver or burr so that the camera is introduced in the proximal anterolateral portal, whereas the burr is introduced from the standard anterolateral portal. The hip may be rotated, flexed, abducted, or adducted to help with bony resection.
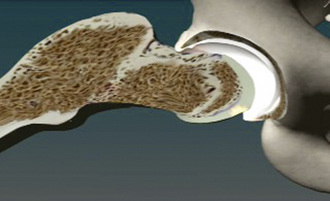
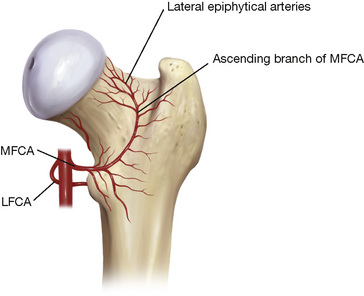
Fortunately, cam lesions are almost exclusively anterior, anterolateral, or lateral. The blood supply to the femoral head, which is supplied by the posterior circumflex vessels, travels within the lateral synovial fold and the femoral neck posterolaterally, which is a safe distance from the resection (Figure 19-19). Injury to these vessels may result in avascular necrosis of the femoral head, although I am not aware of any reported cases of this condition after FAI surgery.
Occasionally cysts of the femoral head–neck junction are seen arthroscopically. These cysts, which were originally thought to be normal variants, are likely the result of the abutment of the femoral neck against the labrum; they are seen in a third of patients with FAI. Thus, the arthroscopic visualization and decompression of these femoral neck cysts help to confirm the location of the impingement and the adequacy of the bony resection (Figure 19-20).
Technical Pearls
Results and outcomes
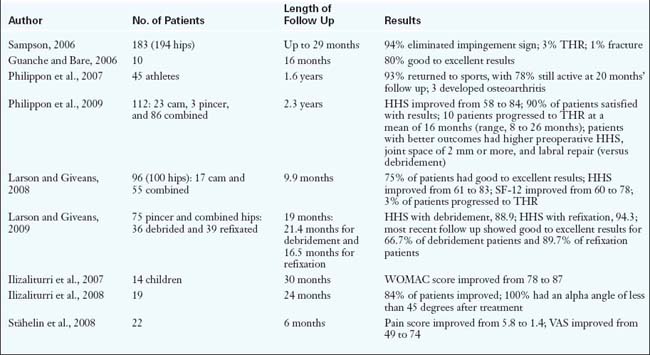
Table 19-1 reports the results of the arthroscopic treatment of FAI. A common theme that correlates with the results of the open surgical treatment studies is that concomitant chondral damage—and particularly arthritis—is a poor prognostic finding, with a larger proportion of failures occurring in this group of patients.
Annotated references and suggested readings
Bardakos N.V., Vanconcelos J.C., Villar R.N. Early outcome of hip arthroscopy for femoroacetabular impingement: the role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg. 2008;90(B):1570-1575.
Bardakos N.V., Villar R.N. Predictors of progression of osteoarthritis in femoroacetabular impingement. A radiological study with a minimum of ten years. J Bone Joint Surg. 2009;91(B):162-169.
Bartlett C.S., DiFelice G.S., Buly R.L., Quinn T.J., Green D.S., Helfet D.L. Cardiac arrest as a result of intraabdominal extravasation of fluid during arthroscopic removal of a loose body from the hip joint of a patient with an acetabular fracture. J Orthop Trauma. 1998;12:294-299.
Beaule P.E., Zaragoza E., Motamedi K., Copeland N., Dorey F.J. Three dimensional computed tomography of the hip in the assessment of femoroacetabular impingement. J Orthop Res. 2006;23:1286-1292.
Beck M., Kalhor M., Leunig M., Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage. J Bone Joint Surg. 2005;87B:1012-1018.
Beck M., Leunig M., Parvizi J., Boutier V., Wyss D., Ganz R. Anterior femoroacetabular impingement: Part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67-73.
Brunner A., Horisberger M., Herzog R.F. Evaluation of a computed tomography–based navigation system prototype for hip arthroscopy in the treatment of femoroacetabular cam impingement. Arthroscopy. 2009;25:382-391.
Byrd J.W., Jones K.S. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467:739-746.
Byrd J.W., Jones K.S. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578-587.
Clarke M.T., Arora A., Villar R.N. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res. 2003;406:84-88.
Funke E.L., Munzinger U. Complications in hip arthroscopy. Arthroscopy. 1996;12:156-159.
Ganz R., Gill T.J., Gautier E., et al. Surgical dislocation of the adult hip: a technique with full access to femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg. 2001;83-B:1119-1124.
Ganz R., Parvizi J., Beck M., Leunig M., Notzli H., Siebenrock K. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120.
Glick J.M. Complications of hip arthroscopy by the lateral approach. In: Sherman O.H., Minkoff J., editors. Current management of orthopaedics: arthroscopic surgery. Baltimore: Williams & Wilkins; 1990:1-9.
Goodman D.A., Feighan J.E., Smith A.D., Latimer B., et al. Subclinical slipped capital femoral epiphysis. J Bone Joint Surg. 1997;79A:1489-1497.
Guanche C.A., Bare A.A. Arthroscopic treatment of femoroacetabular impingement. Arthroscopy. 2006;22:95-106.
Haupt U., Volkle D., Waldherr C., Beck M. Intra- and retroperitoneal irrigation liquid after arthroscopy of the hip joint. Arthroscopy. 2008;24:966-968.
Ilizaliturri V.M.Jr, Nossa-Barrera J.M., Acosta-Rodriguez E., Camacho-Galindo J. Arthroscopic treatment of femoroacetabular impingement secondary to paediatric hip disorders. J Bone Joint Surg Br. 2007;89(B):1025-1030.
Ilizaliturri V.M.Jr, Orozco-Rodriguez L., Acosta-Rodríguez E., Camacho-Galindo J. Arthroscopic treatment of cam-type femoroacetabular impingement: preliminary report at 2 years minimum follow-up. J Arthroplasty. 2008;23:226-234.
Ito K., Minka M.A.II, Leunig M., Werlen S., Ganz R. Femoroacetabular impingement and the cam-effect. An MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg. 2001;83B:171-176.
Jäger M., Wild A., Westhoff B., Krauspe R. Femoroacetabular impingement caused by a femoral osseous head–neck bump deformity: clinical, radiological, and experimental results. J Orthop Sci. 2004;9:256-263.
Johnston T.L., Schenker M.L., Briggs K.K., Philippon M.J. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24:669-675.
Kim K.C., Hwang D.S., Lee C.H., Kwon S.T. Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res. 2006;456:128-132.
Kim Y.T., Azuma H. The nerve endings of the acetabular labrum. Clin Orthop Relat Res. 1995;320:176-181.
Larson C.M., Giveans M.R. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369-376.
Larson C.M., Giveans M.R. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540-546.
Lavigne M., Parvizi J., Beck M., Siebenrock K.A., Ganz R., Leunig M. Anterior femoroacetabular impingement. Part I. techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61-66.
Leunig M., Beck M., Kalhor M., Kim Y., Werlen S., Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236:237-246.
Leunig M., Podeszwa D., Beck M., Werlen S., Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;418:74-80.
Mardones R.M., Gonzalez C., Chen Q., Zobitz M., Kaufman K.R., Trousdale R.T. Surgical treatment of femoroacetabular impingement: evaluation of the effect of the size of the resection. J Bone Joint Surg. 2005;87(A):273-279.
Murray R.O. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810-824.
Myers S.R., Eijer H., Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:81-92.
Nötzli H.P., Wyss T.F., Stoecklin C.H., Schmid M.R., Treiber K., Hodler J. The contour of the femoral head–neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg. 2002;84B:556-560.
Philippon M.J., Briggs K.K., Yen Y.M., Kuppersmith D.A. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg. 2009;91(B):16-23.
Philippon M.J., Maxwell R.B., Johnston T.L., Schenker M., Briggs K.K. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041-1047.
Philippon M., Schenker M., Briggs K., Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908-914.
Safran M.R. Evaluation of the hip: history, physical examination and imaging. Op Tech Orthop Sports Med. 2005;13:2-12.
Sampson T.G. Arthroscopic treatment of femoroacetabular impingement: a proposed technique with clinical experience. Instr Course Lect. 2006;55:337-346.
Sampson T.G. Complications of hip arthroscopy. Clin Sports Med. 2001;20:831-835.
Sharma A., Sachdev H., Gomillion M. Abdominal compartment syndrome during hip arthroscopy. Anesthesia. 2009;64:567-569.
Stähelin L., Stähelin T., Jolles B.M., Herzog R.F. Arthroscopic offset restoration in femoroacetabular cam impingement: accuracy and early clinical outcome. Arthroscopy. 2008;24:51-57.
Stulberg S.D., Cordell L.D., Harris W.H., Ramsey P.L., MacEwen G.D. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St. Louis, MO: CV Mosby; 1975:212-228.
Sussmann P.S., Ranawat A.S., Lipman J., Lorich D.G., Padgett D.E., Kelly B.T. Arthroscopic versus open osteoplasty of the head-neck junction: a cadaveric investigation. Arthroscopy. 2007;23:1257-1264.
Tanzer M., Noiseux N. Osseous abnormalities and early osteoarthritis. The role of hip impingement. Clin Orthop Relat Res. 2004;29:170-177.
Wagner S., Hofstetter W., Chiquet M., et al. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11:508-518.
Wenger D.E., Kendell K.R., Miner M.R., Trousdale R.T. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res. 2004;426:145-150.
Wyss T.F., Clark J.M., Weishaupt D., Nötzli H.P. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152-158.