CHAPTER 20 Arthroscopic-Assisted Treatment of Distal Radius Fractures
The advent of wrist arthroscopy in the early 1990s marked the beginning of a novel and valuable adjunct in the treatment of distal radius fractures.1 Anatomical reduction, stable internal fixation, and preservation of soft tissues are cornerstone concepts in fracture reconstruction. Distal radius fractures represent a unique subset of upper extremity injuries because they often involve not only articular margins but also surrounding soft tissue structures critical to normal wrist function. As arthroscopic technology has evolved at a rapid pace, so, too, has the utility of wrist arthroscopy in the treatment of various subtypes of distal radius fractures.
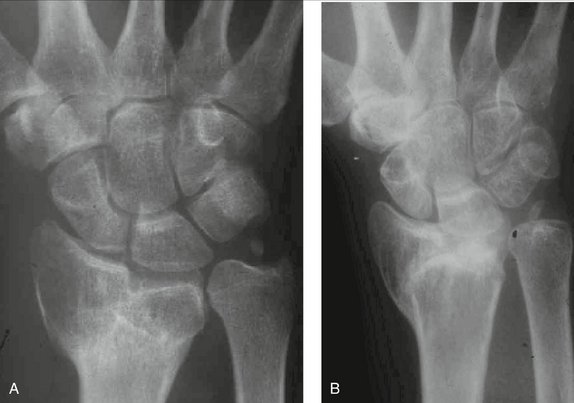
Precise reduction of the distal radial articular surface is critical in preventing the late sequelae of post-traumatic arthrosis. Numerous studies have shown that a poor result is likely if more than 1 mm of articular incongruity is present at the radiocarpal joint (Figs. 20-1 to 20-3).2–6 Subchondral hematomas in the radiocarpal joint have also been shown to cause the early onset of mild osteoarthritis and worse outcomes after 1 year, even without a fracture line as demonstrated by arthroscopy.7 Arthroscopic irrigation and débridement of hematoma may therefore ultimately improve outcome by removing a possible impetus for early post-traumatic degenerative changes.
ARIF affords a well-lit, magnified view of the distal radial joint surface with minimal morbidity. It has been shown to be superior to C-arm and plain radiographs for assessing both displacement between articular fragments as well as the diagnosis of soft tissue lesions.8,9 In a study performed by Edwards and coworkers of intra-articular distal radial fractures that underwent closed manipulation and percutaneous pinning followed by sequential assessment of reduction by C-arm, radiography, and wrist arthroscopy, 33% of cases judged to have had optimal reduction by C-arm and radiography were found to have an articular displacement of more than 1 mm by adjunctive arthroscopy.8 It has also been shown that arthroscopic-assisted reduction and external fixation of distal radius fractures permits a more thorough inspection of the ulnar-sided components of the injury when compared with fluoroscopic-assisted reduction and external fixation of distal radius fractures alone. In addition, a prospective cohort study showed that at follow-up examination, patients who underwent arthroscopic-assisted procedures had a greater degree of supination, flexion, and extension than patients undergoing fluoroscopic-assisted surgery.10 It is now recognized that intraoperative fluoroscopic imaging does not provide sufficient precision to visualize a 1-mm step-off in the radial articular surface despite often satisfactory postoperative radiographs.1,11
Indications and Contraindications
Although the main indication for ARIF of a distal radius fracture is an intra-articular step-off of more than 1 mm, arthroscopy is particularly useful in the management of unstable or displaced intra-articular fractures as well as comminuted articular fractures. Additional fracture patterns amenable to ARIF include radial styloid fractures, lunate die-punch fractures, three-part T fractures, and Melone four-part fractures.12 Other reasons to perform arthroscopy may include radiographic signs of concomitant injury, including diastasis of intercarpal joint spaces, subluxation of the distal radioulnar joint (DRUJ), or a broken carpal arch. ARIF may be contraindicated in the setting of forearm compartment syndrome, untreated median nerve compression, severe soft tissue injury, open joint injuries, unreduced carpal dislocations, infection, and complex regional pain syndrome.13
Timing of Surgery, Setup, and Portals
Before introducing the arthroscope, a pneumatic tourniquet (set at 250 mm Hg) is applied to the upper arm and an Esmarch bandage is wrapped around the forearm to diminish fluid extravasation into the muscle compartments. Lactated Ringer’s solution is used for irrigation because of its rapid absorbability.14
The operating room setup and arthroscopic portals are virtually identical to those used in an elective wrist arthroscopy. Either a horizontal or a vertical arthroscopic setup may be used (Fig. 20-4).15 Swelling often makes it difficult to palpate the extensor intervals, so the use of bony landmarks including the bases of the second and third metacarpals, Lister’s tubercle, radial styloid, and distal ulna is useful. Traction provides ligamentotaxis, which aids in fracture fragment reduction. A useful technique to avoid iatrogenic cartilage damage during the introduction of arthroscopic instrumentation is the use of a 20-gauge needle in the proposed 3-4 portal before making a skin incision.14 If the needle passes unobstructed without engaging bone, the portal is likely in the correct position. Fluoroscopy can also aid in needle placement and portal establishment.
The arthroscopic sheath is usually introduced in the 3-4 portal, and an outflow cannula is established in the 6-R portal. The first image obtained on entry into the joint is usually that of fibrin clot and debris. Lavage is particularly useful and nearly always necessary to clear the joint and provide unobstructed visualization for precise fragment manipulation and reduction. Washing out fracture hematoma and debris may also contribute to the increased range of motion and functional outcome associated with ARIF.16,17
Midcarpal arthroscopy offers significant information to the arthroscopic examination, particularly in the setting of soft tissue injuries suspected with distal radius fractures. Hofmeister and associates showed that a pathological process leading to additional surgical intervention was found on midcarpal examination in more than 60% of patients undergoing arthroscopy for evaluation of soft tissue injuries in the setting of distal radius fractures.18
Surgical Technique
Two-Part Radial Styloid Fractures
Most radial styloid fractures can also be reduced by closed manipulation. Adequate reduction may be evaluated fluoroscopically, arthroscopically, or by a combination of the two (Figs. 20-5 to 20-8). Because radial styloid fractures have a propensity for rotation, K-wire joysticks can be used to manipulate fracture segments. The K-wires may be inserted through a 14-gauge needle, drill sleeve, or drill tap to protect the surrounding neurovascular structures (radial artery and superficial branch of the radial nerve). Arthroscopic assessment of adequate reduction of the articular surface is best evaluated by placing the scope in the 4-5 portal. Once adequate reduction is obtained, the K-wires may be driven across the fracture or another means of fixation, such as a cannulated screw, may be used for fixation (Fig. 20-9). Arthroscopic assistance is also useful in assessing for associated soft tissue injuries in the setting of radial styloid fractures. Scapholunate tears have been identified in up to 50% of radial styloid fractures, and arthroscopic assistance is therefore useful in assessing for these intercarpal injuries.15
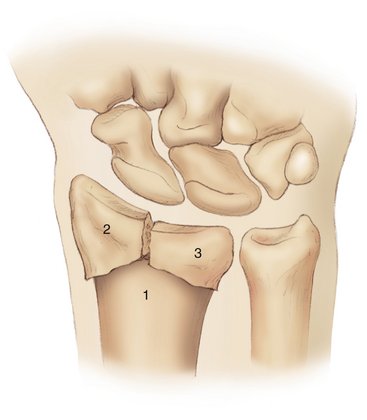
Three-Part Fractures
The arthroscopic-assisted approach to management of three-part fractures (Figs. 20-10 and 20-11) includes preliminary reduction of the radial styloid as previously described. The reduced styloid segment may then be used as a landmark to reduce the medial fragment (Fig. 20-12). Articular gaps may be reduced with the aid of a bone tenaculum, and depressed articular fragments may be elevated with the aid of a bone awl or a percutaneously placed Steinman pin. In select cases, bone grafting may be required.19,20 Once again, arthroscopic assistance allows superior assessment of articular surface reduction and assessment of associated soft tissue injuries.21
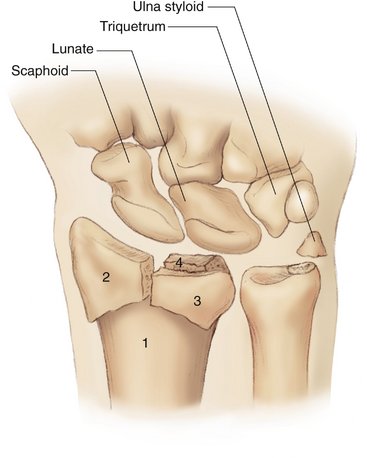
Four-Part Fractures
Melone four-part fractures are characterized by further splitting of the medial segment into volar and dorsal fragments (Fig. 20-13).22 Initial traction allows ligamentous reduction of fracture segments. Attention is first directed toward reduction of the radial styloid, which then serves as a guide for further fragment reduction. A limited open volar incision is usually required to allow adequate mobilization and reduction of the volar fragment. Buttress plate fixation (usually a 2.7-mm condylar plate) allows stabilization of the volar fragment, which may then be used as a fulcrum to reduce the dorsal fragment. Arthroscopic visualization again assists in evaluating adequate reduction of the dorsal fragment.
Management of Associated Injuries
Distal radius fractures exhibit a high incidence of associated injuries, including chondral and soft tissue injuries to the DRUJ, scapholunate interosseous ligament, lunotriquetral interosseous ligament, as well as the soft tissue structures on the ulnar side of the wrist, including the triangular fibrocartilage complex (TFCC). Geissler and colleagues reported that as many as 68% of patients with intra-articular fractures of the distal end of the radius had associated soft tissue injuries of the wrist.23 The most commonly associated injury was a tear of the TFCC (49%), followed by injury to the scapholunate interosseous ligament (32%) and injury to the lunotriquetral interosseous ligament (15%). Twenty percent of patients had multiple soft tissue injuries, and chondral lesions of the carpal bones occurred in 23% to 44% of patients with displaced distal radius fractures. Subsequent studies have demonstrated similar results.15,19,24 Arthroscopy, therefore, allows the treating surgeon to promptly identify and treat associated injuries that may otherwise be missed altogether or diagnosed at a later date requiring secondary reconstruction.
Chondral Lesions
Numerous studies have shown that distal radius fractures evaluated arthroscopically revealed cartilage lesions in both the carpus and distal radius articular surfaces in as many as 18% to 44% (average 27%) of patients.1,7,23,25–27 These lesions include subchondral hematomas, cartilage impaction lesions, as well as chondral fractures. The significance of chondral injury was demonstrated by Lindau, who showed that in one third of patients with dislocated distal radius fractures and chondral defects, early onset of mild osteoarthritis was found in the same area as the identified lesion and worse outcomes were seen at 1-year follow-up.7
Scapholunate Injuries
Intercarpal ligaments play a crucial role in the biomechanics of normal wrist function.28 If a complete rupture of the scapholunate or lunotriquetral intercarpal ligaments remains untreated, the resulting chronic alteration in wrist kinematics will lead to a predictable pattern of wrist arthrosis. Early primary treatment clearly yields superior results; therefore, early precise diagnosis is critical.13 Arthroscopy allows direct visualization and magnification of the carpus and is currently the preferred imaging modality of many surgeons to evaluate for internal derangement of the wrist.29,30
In the setting of distal radius fractures, scapholunate interosseus ligament injuries have been reported to occur in 18% to 54% (average 31%) of patients undergoing arthroscopy.1,15,19,23,25–27 Geissler and colleagues described a widely accepted arthroscopic classification system of tears of the intracarpal ligaments.23 Grade I tears represent attenuation/hemorrhage of the ligament with no incongruence of carpal alignment. Grade II tears, as seen from the midcarpal space, represent partial tears of the ligament and add the element of incongruency to grade I. Grade I and II tears have the potential to progress to degenerative wrist disease, but there is no current consensus regarding the optimal treatment, which could include either immobilization or arthroscopic pin fixation for 6 to 8 weeks in an effort to promote ligament healing.
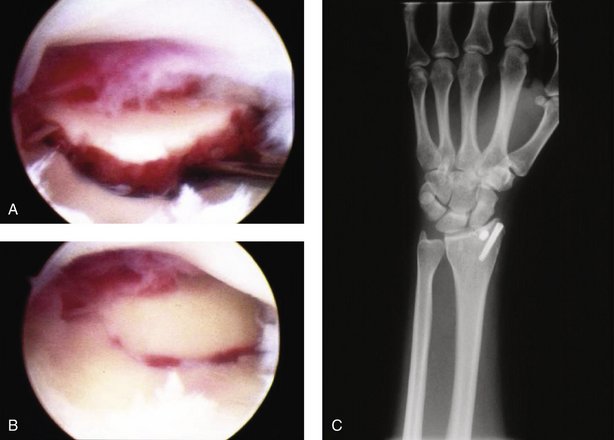
Grade III tears are characterized by incongruence or step-off of carpal alignment when viewed from both the radiocarpal and midcarpal joints. A small arthroscopic probe (1 mm) may be passed through a gap between the carpal bones demonstrating a complete tear of the intracarpal ligament. Grade IV lesions represent gross instability of carpal bones with incongruence and the ability to pass a 2.7-mm arthroscope through the gap between the carpal bones—a “drive-through lesion” (Figs. 20-14 to 20-16).
In studies that grade scapholunate injuries associated with distal radius fractures, grade II tears are the most commonly reported subtype of scapholunate lesion (roughly 50%). Overall, scapholunate tears are associated with radial styloid and lunate impaction fractures, dorsal displacement of the radius greater than 20 degrees, and static dorsal intercalated segment instability (DISI) on prereduction films. When carpal incongruence is apparent through both radiocarpal and midcarpal portals, and a probe can be passed from the radiocarpal to the midcarpal joint through the scapholunate ligament (grade III tears and greater), ARIF may be indicated. This is best performed by scapholunate ligament débridement and transfixion with K-wires (Fig. 20-17). Grade III and IV tears requiring pinning are reported to occur in 25% to 37% of patients (Figs. 20-18 and 20-19).19,23 In some cases, direct arthroscopic repair is not possible and treatment options could include open repair, open repair combined with capsulodesis, or stabilization with tendon transfer.31
Lunotriquetral Injuries
Lunotriquetral ligament injuries are reported in 12% to 15% of patients undergoing arthroscopy in the management of distal radius fractures. These injuries may be associated with a basi-ulnar styloid fracture or volar intercalated segment instability (VISI) pattern on the prereduction radiograph. Geissler and colleagues reported lunotriquetral tears in a series of 9 of 60 patients (15%).23 Seven of these 9 patients (77%) had grade III complete tears. The other 2 patients had partial tears of the lunotriquetral ligament. In our series, only 5% of patients with identified lunotriquetral tears were considered unstable enough to require pinning with K-wires (Fig. 20-20), but other series report lunotriquetral transfixation in up to 75% of patients with identified lunotriquetral tears in the setting of distal radius fractures.19,26
Concurrent Injuries
Roughly 20% of patients may have combined soft tissue injuries in association with arthroscopically evaluated distal radius fractures. Combined injuries most commonly involve TFCC and scapholunate injuries, followed by TFCC and lunotriquetral injuries, and scapholunate and lunotriquetral injuries.19,26 Slade and coworkers have reported combined fractures of the scaphoid and distal radius treated by percutaneous and arthroscopic techniques.32 They recommend percutaneous reduction of the scaphoid fracture and provisional stabilization with a guidewire placed along its central axis, percutaneous/arthroscopic reduction and rigid fixation of the distal radius fracture to permit early motion, and, lastly, fixation of the scaphoid fracture with implantation of a cannulated headless compression screw. Fractures of the ulnar styloid are frequently associated with distal radius fractures as well. Arthroscopy helps to provide a treatment rationale in approaching management of the ulnar styloid fracture. Loss of the trampoline effect by a probe of the TFCC indicates laxity of the articular disc and may be indicative of DRUJ instability. If there is no demonstrable laxity of the TFCC and a stable DRUJ, the ulnar styloid fracture likely does not need to be stabilized. If, on the other hand, there is laxity of the articular disc and/or DRUJ instability, the ulnar styloid fracture should be fixed with pins or screws.
Complications
Complications of ARIF have been minimal in reported case series. A small percentage of patients may have settling of the fracture fragments resulting in loss of volar tilt. Five to 10 percent of patients may develop complications related to percutaneous pin placement, including loosening, infection, and sensory nerve irritation, but these findings may not be directly related to ARIF itself.19 In addition, the development of complex regional pain syndrome in two patients after ARIF has been reported.1
Outcomes
There is now enough scientific evidence to validate the effectiveness and safety of ARIF in the management of distal radius fractures. Unfortunately, there are no prospective randomized double-blinded studies comparing ARIF with open reduction and internal fixation (ORIF) without arthroscopic assistance. Several studies have, however, compared results of ARIF versus ORIF in the treatment of distal radius fractures.17,23,29 These studies uniformly describe increased range of motion, better outcomes, and better articular reduction with arthroscopic assistance when compared with ORIF without arthroscopic assistance.
Several concepts must be considered when assessing outcomes with respect to the use of arthroscopy in the management of selected distal radius fractures. The orthopaedic literature has proved that there is a direct relationship between the quality of anatomical reconstruction (which implies the recognition of all injuries) and the subsequent stability of that reconstruction. A stable construct allows for preservation of motion, minimizes the risk of post-traumatic arthrosis, and finally optimizes long-term functional outcome. Multiple studies have shown that the use of arthroscopy is effective in not only identifying and evaluating distal radius fractures and their associated injuries but also facilitating anatomical reduction and reconstruction.17,19
1. Cognet JM, Bonnomet F, Ehlinger M, et al. Arthroscopy-guided treatment of fractures of the distal radius: 16 wrists. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:515-523.
2. Axelrod TS, McMurtry RY. Open reduction and internal fixation of comminuted, intra-articular fractures of the distal radius. J Hand Surg [Am]. 1990;15:1-11.
3. Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647-659.
4. Trumble TE, Culp RW, Hanel DP, et al. Intra-articular fractures of the distal aspect of the radius. Instr Course Lect. 1999;48:465-480.
5. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg [Am]. 1994;19:325-340.
6. Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg [Am]. 1991;16:375-384.
7. Lindau T, Adlecreutz C, Aspenberg P. Cartilage injuries in distal radial fractures. Acta Orthop Scand. 2003;74:327-331.
8. Edwards CC, Haraszti CJ, McGillivary GR, Gutow AP. Intra-articular distal radius fractures: arthroscopic assessment of radiographically assisted reduction. J Hand Surg [Am]. 2001;26:1036-1041.
9. Kordasiewicz B, Pomianowski S, Orlowski J, Rapala K. Interosseous ligaments and TFCC lesions in intraarticular distal radius fractures—radiographic versus arthroscopic evaluation. Ortop Traumatol Rehabil. 2006;8:263-267.
10. Ruch DS, Vallee J, Poehling GG, et al. Arthroscopic reduction versus fluoroscopic reduction in the management of intra-articular distal radius fractures. Arthroscopy. 2004;20:225-230.
11. Nijs S, Broos PL. Fractures of the distal radius: a contemporary approach. Acta Chir Belg. 2004;104:401-412.
12. Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg [Am]. 1994;19:325-340.
13. Wiesler ER, Chloros GD, Mahirogullari M, Kuzma GR. Arthroscopic management of distal radius fractures. J Hand Surg [Am]. 2006;31:1516-1526.
14. Geissler W, Freeland A. Arthroscopic management of intra-articular distal radius fractures. Hand Clin. 1999;15:455-466.
15. Lindau T, Arner M, Hagberg L. Intra-articular lesions in distal fractures of the radius in young adults: a descriptive arthroscopic study in 50 patients. J Hand Surg [Br]. 1997;22:638-643.
16. Geissler WB. Intra-articular distal radius fractures: the role of arthroscopy. Hand Clin. 2005;21:407-416.
17. Doi K, Hattoi Y, Otsuka K, et al. Intra-articular fractures of the distal aspect of the radius: arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am. 1999;81:1093-1110.
18. Hofmeister EP, Dao KD, Glowacki KA, Shin AY. The role of midcarpal arthroscopy in the diagnosis of disorders of the wrist. J Hand Surg [Am]. 2001;26:407-414.
19. Culp RW, Osterman AL, Kaufmann RA. Wrist arthroscopy: operative procedures. In: Green DP, editor. Operative Hand Surgery. New York: Elsevier, 2005.
20. Chen AC, Chan YS, Yuan LJ, et al. Arthroscopically assisted osteosynthesis of complex intra-articular fractures of the distal radius. J Trauma. 2002;53:354-359.
21. Levy HJ, Glickel SZ. Arthroscopic assisted internal fixation of volar intra-articular wrist fractures. Arthroscopy. 1993;9:122-131.
22. Melone CP. Articular fractures of the distal radius. Orthop Clin North Am. 1984;15:217-236.
23. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-365.
24. Hanker GJ. Radius fractures in the athlete. Clin Sports Med. 2001;20:189-201.
25. Mathoulin C, Sbihi A, Panciera P. Interest in wrist arthroscopy for treatment of articular fractures of the distal radius: report of 27 cases. Chir Main. 2001;20:342-350.
26. Shih JT, Lee HM, Hou YT, Tan CM. Arthroscopically-assisted reduction of intra-articular fractures and soft tissue management of distal radius. Hand Surg. 2001;6:127-135.
27. Rose S, Frank J, Marzi I. Diagnostic and therapeutic significance of arthroscopy in distal radius fracture. Zentralbl Chir. 1999;124:984-992.
28. Mayfield JK, Johnson RP, Kilcoyne RK. Carpal dislocations: pathomechanics and progressive perilunar instability. J Hand Surg [Am]. 1980;5:226-241.
29. Weiss AP, Akelman E, Lambiase R. Comparison of the findings of triple-injection cinearthrography of the wrist with those of arthroscopy. J Bone Joint Surg [Am]. 1996;78:348-356.
30. Cooney WP. Evaluation of chronic wrist pain by arthrography, arthroscopy, and arthrotomy. J Hand Surg [Am]. 1993;18:815-822.
31. Walsh JJ, Berger RA, Cooney WP. Current status of scapholunate interosseous ligament injuries. J Am Acad Orthop Surg. 2002;10:32-42.
32. Slade JF3rd, Taksali S, Safanda J. Combined fractures of the scaphoid and distal radius: a revised treatment rationale using percutaneous and arthroscopic techniques. Hand Clin. 2005;21:427-441.