Chapter 38 Aquatic Therapy for the Arthritic Knee
INTRODUCTION
Water has been used for healing, spiritual, and religious purposes since at least 2400 bc.15 Water was used by the people of Asia to combat fevers as early as 1500 BC. Hippocrates (460–375 BC) used water for relief of muscle spasms and joint pain.23 For many years, water exercise was dismissed as a medical intervention and considered to be purely recreational. The advent of spas in Europe and around the world moved water-based interventions into the leisure and recreation category, making reimbursement for water-based medical interventions difficult.
Despite a history spanning over 4000 years, a resurgence of aquatics as an intervention has occurred in the past quarter century. The Aquatic Section of the American Physical Therapy Association was organized as recently as 1992. Throughout this history, many different terms have been used to describe rehabilitation that takes place in the water. Some of these terms include hydrotherapy, aquatic therapy, spa therapy, water therapy, water gymnastics, balneotherapy, and pool therapy. Currently, the term balneotherapy is still distinguished from other forms of hydrotherapy. Balneotherapy refers to the use of hot-water or thermal treatments to decrease pain and stiffness and promote muscle relaxation. Balneotherapy often uses minerals, salts, or sulfur treatments, mud packs, and water jets to achieve these goals. Hydrotherapy is a general term covering any type of water intervention, which might include balneotherapy or exercise. For the purposes of this chapter, the focus remains on the use of exercise in water for the treatment of knee arthritis. For further information on balneotherapy, the reader is referred to Verhagen and coworkers.36
SCIENTIFIC BASIS
Buoyancy
Buoyancy is the upward thrust experienced during immersion that is in direct opposition to gravity. Buoyancy is used to unload the lower extremity from the effects of gravity, making it a useful tool for those with knee arthritis. Archimedes’ principle states that an immersed body at rest experiences an upward thrust equal to the weight of the same fluid volume it displaces.6
Buoyancy is related to a person’s specific gravity (SG), which varies with body composition. Any object with an SG less than 1.0 g/cm2 will float, whereas any object with an SG greater than 1.0 g/cm2 will sink. This property forms the basis of underwater weighing to determine body composition. Because lean body mass is heavier than fat mass, those with a high lean body mass tend to sink whereas those with a greater fat mass float. This fact makes it difficult to know precisely how much weight-bearing any given individual is achieving at a given water depth. Harrison and Bulstrode20 performed studies on the percentage of weight-bearing during static standing in various water depths ranging from the hips to the neck. The authors found considerable variability in the amount of weight-bearing with immersion at various depths. This variation might have been partly due to using a fixed-depth pool and only nine subjects. However, the disparity may also be the result of differences in body composition and body fat distribution among individual study subjects, suggesting that a weight-bearing prescription is difficult in this medium. A follow-up study by Harrison and associates21 showed that, compared with static standing, fast walking increased weight-bearing forces up to 76%. Understanding Archimedes’ principle highlights the difficulties in assigning a specific percentage of weight-bearing at any given depth: the weight on the limb will vary with body composition and speed of movement.
The moment of buoyancy is also important in exercise prescription. As with moments of gravity on land, the moment of buoyancy increases with increasing lever arm length and nearer the parallel. If the movement is in an upward direction, the same direction as the force of buoyancy, the activity is considered to be buoyancy assisted. If the movement is toward the pool bottom in opposition to buoyancy, it is considered to be buoyancy resisted. Movements parallel to the bottom that are neither assisted nor resisted by buoyancy are considered buoyancy-supported exercises. For example, in a standing position, a straight leg lift forward would be assisted by buoyancy, whereas the return motion back to the neutral position would be buoyancy resisted. In a supine position, hip abduction and adduction would be buoyancy-supported activities. An important application of this information is used in strengthening hip extensor muscles. In a standing position, the motion of hip extension from neutral to 15° extension (the normal range of hip extension) occurs through such a small range of motion (ROM), with a short moment arm, and is buoyancy assisted, making the exercise little more than a gluteal isometric exercise (Fig. 38-1). However, the motion from 90° hip flexion returning to neutral is also hip extension, but is now moving through a larger range with a longer moment arm against the upward force of buoyancy, making this an effective hip extensor muscle–strengthening exercise (Fig. 38-2).
Hydrostatic Pressure
Pascal’s law states that a fluid exerts pressure equally on an object at a given depth.6 Hydrostatic pressure increases with a greater depth of immersion owing to the weight of the volume of fluid overhead. The increased hydrostatic pressure close to the bottom of the pool assists venous return to the heart and prevents fluid accumulation in the lower extremities. This is useful for patients with knee or ankle arthritis, who tend to experience swelling with exercise. The increased venous return to the heart also affects the cardiorespiratory system. The hydrostatic pressure when the body is immersed to the neck produces an increase in heart volume, intrapulmonary blood volume, right atrial pressure, left ventricular end-diastolic volume, stroke volume, and cardiac output.2,9 Heart rate is unchanged or decreased compared with similar land-based activities.2 Peripheral circulation and vital capacity are decreased.9 This cardiopulmonary response is significant for patients with cardiorespiratory conditions and for those who are trying to achieve training heart rates in deep-water exercise.19 These changes have been noted in individuals both with and without cardiac disease.10,11 Aerobic exercise in neck-deep water will result in heart rates that are approximately 17 to 20 beats/min lower than comparable land-based exercise.3,18,31,34
Viscosity and Hydrodynamics
The viscosity of a fluid is its resistance to adjacent fluid layers sliding freely by one another.6 Viscosity causes a resistance to flow when a body is moving through the water. As such, viscosity is clinically insignificant when a body is stationary. The viscous quality of water allows it to be used effectively for resistance because of its hydrodynamic properties, or fluid mechanics. The key hydrodynamic properties are turbulence and drag.33 Turbulent flow occurs when the speed of movement of an object (or person or body part) reaches a critical velocity or when the flow of water encounters an object (or person or body part).4 In turbulent flow, resistance is proportional to the velocity squared, and increasing the speed of movement significantly increases the resistance.27 Eddies are formed in the wake behind the moving body, creating drag that is greater in the unstreamlined object than in a streamlined object (Figs. 38-3 and 38-4).
Several areas of research provide evidence for these variables. A study by Law and Smidt25 examined the impact of surface area and velocity on force production. Hydrotone (Hydro-Tone Fitness Systems, Inc., Huntington Beach, CA) bells were used at different speeds and angles to assess the impact on force production. Results showed a 50% increase in force production at fast speeds. Force also increased at fast speeds when the bells were oriented at 45° compared with 0°. Orientation had no impact on force production when performed at slow speeds. Therefore, both speed and surface area influence force production when using viscosity. Another study using the Hydrotone boots showed increased drag compared with a barefoot condition.28
A third study examined electromyographic (EMG) data from the shoulder musculature during arm elevation at three different speeds (30°/sec, 45°/sec, and 90°/sec) on land and in the water.24 The percentage of maximum voluntary contraction of the deltoid and rotator cuff musculature was consistently higher on land at the slowest speeds, but higher in the water at 90°/sec, highlighting the positive relationship among viscosity, speed, and force generation.
Poyhonen and colleagues27–29 performed several research studies on the hydrodynamics of knee flexion and extension exercises in water and on land in barefoot and increased surface area conditions. The authors found that increasing the surface area of the lower leg significantly increased the level of water resistance. They also found that the EMG activity of the knee flexors and extensors was similar between barefoot and increased surface area conditions despite the increased drag due to the Hydrotone Boot.
Research in the cardiopulmonary effects of speed on measures of exertion also supports the positive relationship between speed and work in the water. Whitley and Schoene38 examined walking on land and in the water at four different speeds. Heart rates were significantly higher after water-walking versus treadmill-walking at all four speeds. In addition, heart rates rose significantly with each increasing speed in water-walking, suggesting increasing cardiopulmonary workloads at increasing speeds. Cassady and Nielsen8 measured oxygen consumption during calisthenic arm and leg exercises at three different speeds on land and in the water. They also found increasing heart rate with increasing speed of exercise in the water. The higher metabolic cost of exercises at a faster speed supports the theory of increased work at faster speeds in the water.
CLINICAL RESEARCH
New clinical research has shown the effectiveness of aquatic rehabilitation for patients with musculoskeletal problems, particularly those with knee arthritis. A study examining outcomes following a water-based program for patients with lower limb osteoarthritis found that group-based water exercise classes over 1 year produced significant reductions in pain and improvements in function.12 A randomized, controlled trial (RCT) compared the effects of a water-based resistance program with a land-based program on function and strength in patients with osteoarthritis of the hip or knee.16 The authors found improvements in strength and function in both the land- and the water-based groups as compared with the control group. Compliance rates were 84% for water therapy and 75% for land therapy. In a similar study, Wyatt and coworkers39 examined changes in function following a land-based or an aquatic exercise program in patients with knee osteoarthritis. Both groups showed significant improvements in measures of ROM, thigh girth, pain scales, and 1-mile walk test. However, the aquatic group had significantly lower pain levels than the land group. Silva and associates32 followed 64 patients with knee osteoarthritis randomly assigned to a land-based or a hydrotherapy program. Both land and water exercises reduced knee pain and increased function, but the hydrotherapy group had significantly lower knee pain scores before and after the 50-foot walk test. The results reinforce the notion that patients can improve strength and function effectively in either a land or an aquatic environment. The key is the ability to provide a comprehensive program, whether on land, in the water, or some combination of both.
Recently, Hinman and colleagues22 performed an RCT randomly assigning 71 participants with hip or knee osteoarthritis to 6 weeks of aquatic physical therapy or no physical therapy. Those in the aquatic physical therapy program had less pain and joint stiffness and greater physical function, quality of life, and hip muscle strength than the control group. Nearly 75% of participants reported improvements in pain and function compared with 17% in the control group. More importantly, 84% of participants continued the aquatic program independently at the conclusion of the study.
Whereas the previous study compared aquatic physical therapy with no physical therapy, Fransen and coworkers17 compared hydrotherapy with Tai Chi or a control group in an RCT of 152 patients with hip or knee osteoarthritis. Results showed that both hydrotherapy and Tai Chi participants improved in the pain and physical function subscales of the Western Ontario and McMaster Osteoarthritis Index (WOMAC), but only the hydrotherapy group achieved significant improvements in the physical performance measures of the Short Form-12-item questionnaire (SF-12). In addition, compliance with the hydrotherapy classes was higher than that with Tai Chi.
An RCT of the effects of a water-based program on balance, fear of falling, and quality of life was performed in community-dwelling older women with osteopenia or osteoporosis.14 The intervention group received a 10-week water-based and self-management program. The intervention group showed significant improvement over the control group in balance and quality of life, but not in fear of falling.
Although structured aquatic physical therapy for patients with knee arthritis is relatively new, there is evidence supporting the clinical effectiveness and cost-effectiveness of this intervention in this population. A Cochrane Review examining the effectiveness of aquatic physical therapy for the treatment of hip and knee osteoarthritis is ongoing.5
APPLICATIONS
Mobility
Key muscles to be stretched in patients with knee arthritis include the gastrocnemius and soleus muscles as well as the quadriceps, hamstring, lateral hip muscles (iliotibial band), and gluteal/buttock muscles (Figs. 38-5 to 38-7). As with stretching exercises on land, the intensity should be subjectively between “low” and “medium” and should be pain-free. The patient should feel stretching in the muscle of interest and not in the joint itself. The patient should be able to hold the stretches for 60 seconds without an increase in pain.4 Repeat the stretches for two or three repetitions.

FIGURE 38-5 Hamstring stretching using a noodle. Other stationary equipment in the pool can also be used for stretching.
Dynamic mobility is easily accomplished in the pool. Dynamic mobility has been advocated as an appropriate means to increase functional mobility, because it requires not only static flexibility but also strength, balance, and neuromotor coordination.26 Dynamic mobility activities in the pool take place in a gravity-lessened environment, which decreases joint-loading forces. The water’s viscosity also slows movement and increases the reaction time for patients with balance difficulties. This property makes the pool a safe environment for such individuals.
Other dynamic mobility activities include marching in place and marching across the pool. Vary the amount of hip and knee flexion based upon patient needs. Marching does not need to proceed in a straight line, but can be on a diagonal to encourage more functional movement patterns. Proprioceptive neuromuscular facilitation (PNF) patterns also encourage functional movement patterns in the lower extremity. Cueing the patient appropriately can emphasize motion at the knee joint when tolerated. For closed chain dynamic mobility, perform squats for hip, knee, and ankle mobility in shallow water or fully flex the hips and knees by flexing and extending these joints at a ladder (Figs. 38-8 and 38-9). These closed chain activities can be progressed by asking the patient to lunge during ambulation (Fig. 38-10).
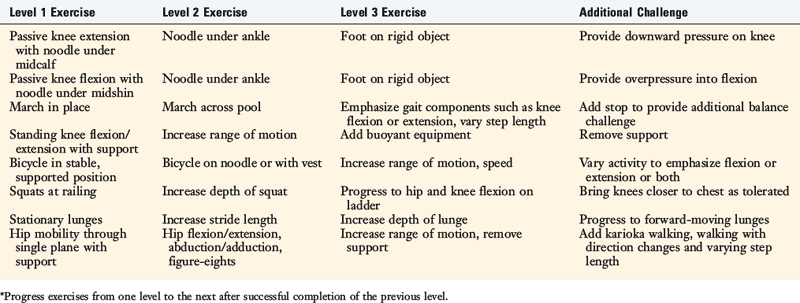
Dynamic mobility can also be performed non–weight-bearing. Bicycling or running with a belt or a noodle is a good way to perform repeated hip and knee flexion and extension. The range of movement can be modified as needed for any given patient. Similarly, deep-water cross-country skiing requires repeated non–weight-bearing sagittal plane mobility, with greater hip motion and less knee motion. These repeated movements provide lubrication via mobility, but lack the weight-bearing component necessary for articular cartilage lubrication (Table 38-1).37
Exercise Using Buoyancy
Strengthening exercises can also use buoyancy as resistance. Adding buoyant equipment to the foot or ankle will increase the challenge of these exercises. Straight leg lifts in the sagittal or frontal planes will result in concentric and eccentric contractions of the muscle groups positioned in opposition to buoyancy. For example, lifting the leg forward and back down will result in eccentric and concentric contractions of the hip extensor muscles if sufficient buoyant equipment is used. If the amount of buoyant equipment is inadequate, the muscle contractions become alternating concentric contractions of the hip flexor muscles and hip extensor muscles. Therefore, the relative amounts of muscle strength and buoyant equipment will determine which muscle groups are working and in what type of muscle contraction. These straight leg lifts strengthen the core hip muscles isotonically while challenging the muscles at the knee isometrically. To challenge these muscles directly, perform buoyancy-resisted hamstring curls in a standing position with the hip flexed to 90° (Fig. 38-11). Buoyancy-resisted quadriceps exercises are performed in a standing position with the knee moving from extension to flexion (Fig. 38-12). Realize that while the moving limb is working in an open chain, the opposite limb is working in a closed chain to stabilize the body against the hydrodynamic forces created by the moving limb. This principle is one of the strengths of working in the aquatic medium.
Functional movement patterns can be trained using buoyant equipment. The same PNF patterns used for mobility can be used for strengthening using buoyant equipment. For example, place a Wet Vest strap (Hydro-Fit, Inc., Eugene, OR) around the ankle and perform PNF diagonals, alphabet writing, or other functional movement patterns with the leg straight. This type of movement provides resistive exercise to muscles throughout the entire leg. Place a noodle under the bottom of a foot and press down as in a leg press for a buoyancy-resisted leg press activity (Fig. 38-13).
Exercise Using Viscosity
Open or closed chain exercises using viscosity provide an opportunity to strengthen lower extremity muscles isotonically. It is important to consider how the exercises are performed to ensure that the structures of interest are being challenged. A study of the hydrodynamic responses to single and repeated knee flexion and extension in the water found high levels of antagonist activity with the repeated activity and lower levels with the single-repetition activity.29 This is an important issue for those wanting to provide both concentric and eccentric muscle contractions during aquatic rehabilitation. Whereas concentric and eccentric contractions of a single muscle group can be achieved using buoyancy-resisted exercise (such as a hamstring curl), this same exercise using viscosity produces reciprocal concentric contractions. A standing hamstring curl with the hip at 90° of flexion will produce reciprocal concentric contractions of the quadriceps and hamstring muscles. However, research by Poyhonen and associates28 suggested that the muscle activity is influenced by the surface area, speed, and limb orientation. During both the flexion and the extension phases of a knee flexion and extension activity in water, the agonist EMG activity decreased with a concurrent increase in the antagonist EMG during the final portion of the ROM. This finding suggests that the moment of the moving water produces lift that tends to “carry” the limb through the final ROM, requiring antagonist activation to decelerate the limb at end ROM. This is more evident in the extension phase of seated knee extension than in the knee flexion phase owing to the additional lift from buoyancy. Therefore, the quadriceps muscles will be activated through a greater ROM if performed in standing and the hip in neutral than in a seated or standing position with the hip at 90°. Similarly, if the goal is to facilitate hamstring muscle activation and minimize quadriceps muscle activation near full knee extension (as in anterior cruciate ligament injuries), then the 90° hip flexion position would be preferable.
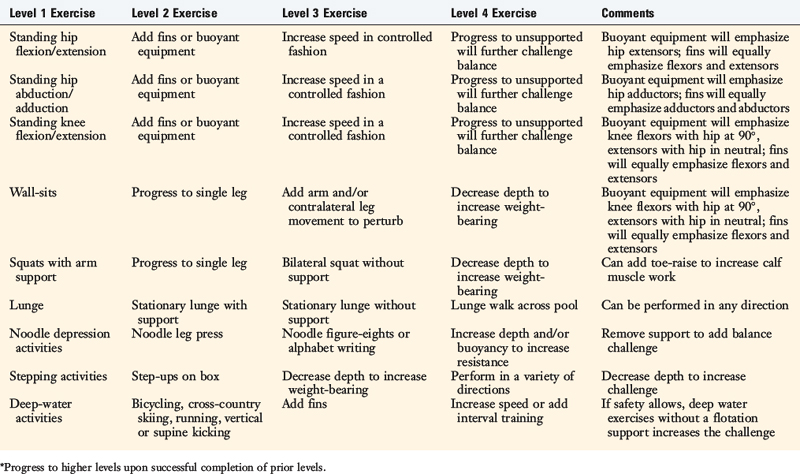
Progress activities using viscosity as resistance by increasing the speed and/or surface area of the exercise. Flippers or fins are good choices for increasing the surface area. Flippers tend to work best in the sagittal plane, whereas Aquafins (The Hygienic Corporation, Akron, OH) can be placed in any plane, providing resistance in the sagittal plane, frontal plane, or on any diagonal in between. Other resistive equipment, such as a Hydro Boot provides a larger surface area for greater resistance.29 Leg kicks, knee exercises, or walking activities can be performed with resistive fins around the ankle. Different components of the activity can be emphasized depending upon how the exercise is cued. For example, during backward walking, emphasizing the knee flexion component will challenge the hamstring and gastrocnemius muscles whereas stressing the hip extension component will challenge the hamstring and gluteal muscles. Generate more resistance by positioning the arms with increased surface area. For example, walk forward with the arms held at 90° abduction or increase the challenge by walking forward while simultaneously horizontally adducting the shoulders. Be aware of the additional stress this will place on the shoulders (Table 38-2).
Balance and Stabilization
The hydrodynamic forces of water provide excellent opportunities for activities to challenge the core muscles and balance. A study of balance training on land and in water found both mediums resulted in improvements in the center of pressure variables.30 No differences were found between the water and the land, suggesting that balance training can be equally effective when performed in water. Exercises can be stationary or moving and can be challenged in a variety of different ways. Whereas strength is important, it is only one component of a program to enhance balance. Muscle activation patterns and knowledge of position in space also contribute to good balance.
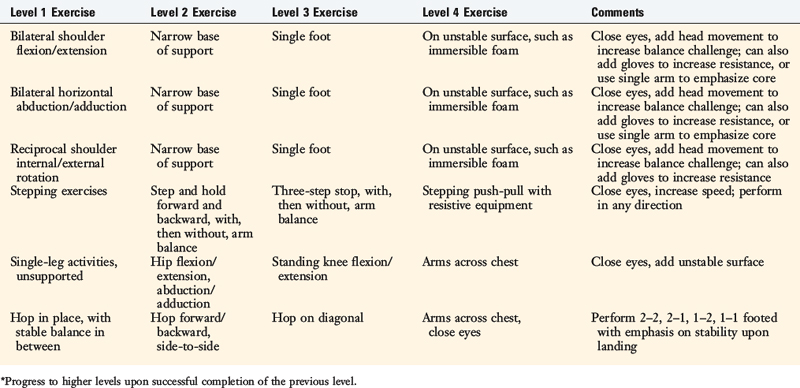
Patients can use their arms to create forces that are resisted by their trunk and core muscles. Reciprocal shoulder flexion and extension produce rotational forces that are resisted by the core muscles. Turning the palms to the direction of movement increases surface area and increases the challenge. Likewise, symmetrical, bilateral shoulder internal and external rotation also creates rotational forces resisted by the trunk. Anterior-posterior sway is produced with any bilateral anterior-posterior movement of the arms such as flexion/extension or horizontal abduction/adduction. Increase the challenge of these exercises by increasing the exercise speed or surface area or by decreasing the base of support by bringing the feet closer together. Further increase the challenge by removing the bilateral symmetry. For example, performing shoulder horizontal abduction/adduction with a single arm minimizes the anterior-posterior sway and produces trunk rotation (Fig. 38-14).
Other balance exercises use movements of the arms or opposite leg while stabilizing on a single leg. A stepping motion with a concurrent pushing and pulling motion with resistive equipment makes an excellent core strengthening and balance exercise. In single-leg stance, pushing a ball down works on stability of the entire lower extremity. To increase the challenge, these exercises can be performed on an unstable base such as Therafoam (The Hygienic Corporation, Akron, OH) submerged in the water (Table 38-3).
Cardiopulmonary
Regular aerobic exercise is an important component of general fitness and weight loss. The American College of Sportsmedicine1 and the American Heart Association recommend performing moderately intense cardiopulmonary activity 30 minutes a day, 5 days a week, or performing vigorously intense cardiopulmonary activity 20 minutes a day, 3 days a week. These organizations also recommend regular strength-training exercises. For patients with arthritis or complex problems at the knee, many of the traditional cardiopulmonary-training activities are too painful. Most of these activities involve some weight-bearing through the knee. Walking, running, elliptical trainers, stair-steppers, and ski machines all require weight-bearing through the knee. Bicycling places lower weight-bearing loads across the knee than other cardiopulmonary-training activities, but still places large demands on this joint.
Research has shown that subjects exercising in the water can achieve a sufficient training stimulus.7,13,35 D’Acquisto and colleagues13 and Campbell and coworkers7 found that controlling the frequency, intensity, and duration of shallow water exercise resulted in a training response sufficient to meet the American College of Sportsmedicine’s guidelines in younger and older women. Takeshima and associates35 found that exercising three times per week for 12 weeks resulted in an increase in peak volume of oxygen consumption (VO2). Improvements in muscle strength, power, flexibility, agility, and subcutaneous fat were also found. All of these changes are positive for people who have complex knee problems.
Training parameters in the water are basically the same as those on land. Manipulating the frequency, intensity, and duration to meet the American College of Sportsmedicine’s guidelines1 follows the same thought process as those on land. One important issue is skill level in the water. Unskilled deep-water exercisers report higher rates of perceived exertion and have higher lactate levels than skilled deep-water runners. As patients become skilled and comfortable with the new techniques, the exertion levels and heart rate will decrease. Exercise in deep water will result in a heart rate approximately 20 beats/min lower than comparable land-based exercise owing to the effects of hydrostatic pressure.34
1 American College of Sportsmedicine. Guidelines for exercise testing and prescription. Physical Activity and Public Health Guidelines. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2006.
2 Arborelius M., Balldin U., Lilja B., Lundgren C. Hemodynamic changes in man during immersion with the head above water. Aerospace Med. 1972;43:592-598.
3 Avellini B., Shapiro Y., Pandolf K. Cardio-respiratory physical training in water and on land. Eur J Appl Physiol. 1983;50:255-263.
4 Bandy W., Irion J. The effect of time of static stretch on the flexibility of the hamstring muscles. Phys Ther. 1994;74:845-852.
5 Bartels E., Lund H., Hagen K., et al. Aquatic exercise for the treatment of knee and hip osteoarthritis. Review. Cochrane Database Syst Rev. 2005;4:CD005523.
6 Beiser A., editor. Basic physical principles and their application. Physics. Menlo Park, CA: Benjamin/Cummings, 1978.
7 Campbell J., D’Acquisto L., D’Acquisto D., Cline M.G. Metabolic and cardiovascular responses to shallow water exercise in young and older women. Med Sci Sports Exerc. 2003;35:675-681.
8 Cassady S., Nielsen D. Cardiorespiratory responses of healthy subjects to calisthenics performed on land versus in the water. Phys Ther. 1992;72:532-538.
9 Christie J., Sheldahl L., Tristani F. Cardiovascular regulation during head-out immersion exercise. J Appl Physiol. 1990;69:657-664.
10 Cider A., Sunnerhagen K., Schaufelberger M., Andersson B. Cardiorespiratory effects of warm water immersion in elderly patients with chronic heart failure. Clin Physiol Funct Imaging. 2005;25:313-317.
11 Cider A., Svealv B., Tang M., et al. Immersion in warm water induces improvement in cardiac function in patients with chronic heart failure. Eur J Heart Fail. 2006;8:308-313.
12 Cochrane T., Davey R., Matthes Edwards S. Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis. Health Technol Assess. 2005;9(31):1-114.
13 D’Acquisto L., D’Acquisto D., Renne D. Metabolic and cardiovascular responses in older women during shallow water exercise. J Strength Cond Res. 2001;15:12-19.
14 Devereux K., Robertson D., Briffa N. Effects of a water-based program on women 65 years and over: a randomised controlled trial. Aust J Physiother. 2005;51:102-108.
15 Finnerty G., Corbitt T., editors. Hydrotherapy. New York: Frederick Ungar, 1960.
16 Foley A., Halbert J., Hewitt T., Crotty M. Does hydrotherapy improve strength and physical function in patients with osteoarthritis: a randomised controlled trial comparing a gym-based and a hydrotherapy-based strengthening program. Ann Rheum Dis. 2003;62:1162-1167.
17 Fransen M., Nairn L., Winstanley J., et al. Physical activity for osteoarthritis management: a randomized controlled clinical trial evaluating hydrotherapy or Tai Chi classes. Arthritis Rheum. 2007;57:407-414.
18 Hall J., Macdonald I., Maddison P., O’Hare J. Cardiorespiratory responses to underwater treadmill walking in healthy females. Eur J Appl Physiol Occup Physiol. 1998;77:278-284.
19 Hall J., Skevington S., Maddison P., Chapman K. A randomized and controlled trial of hydrotherapy in rheumatoid arthritis. Arthritis Care Res. 1996;9:206-215.
20 Harrison R., Bulstrode S. Percentage weightbearing during partial immersion in the hydrotherapy pool. Physiother Pract. 1987;3:60-64.
21 Harrison R., Hillman M., Bulstrode S. Loading the lower limb when walking partially immersed: implications for clinical practice. Physiother Pract. 1992;78:164-166.
22 Hinman R., Heywood S., Day A. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Phys Ther. 2007;87:32-43.
23 Irion J. Historical overview of aquatic rehabilitation. In: Ruoti R., Morris D., Cole A., editors. Aquatic Rehabilitation. Philadelphia: Lippincott; 1997:3-13.
24 Kelly B., Roskin L., Kirkendall D., Speer K. Shoulder muscle activation during aquatic and dry land exercises in nonimpaired subjects. J Orthop Sports Phys Ther. 2000;30:204-210.
25 Law L., Smidt G. Underwater forces produced by the Hydro-Tone bell. J Orthop Sports Phys Ther. 1996;23:267-271.
26 Mandelbaum B., Silvers H., Watanabe D. Effectiveness of a neuromuscular training on the incidence of knee injury in female athletes: 2-year follow-up. Am J Sports Med. 2005;33:1003-1010.
27 Poyhonen T., Keskinen K., Hautala A., Malkia E. Determination of hydrodynamic drag forces and drag coefficients on human leg/foot model during knee exercise. Clin Biomech. 2000;15:256-260.
28 Poyhonen T., Keskinen K., Kyrolainen H., et al. Neuromuscular function during therapeutic knee exercise under water and on dry land. Arch Phys Med Rehabil. 2001;82:1446-1452.
29 Poyhonen T., Kyrolainen H., Keskinen K., et al. Electromyographic and kinematic analysis of therapeutic knee exercises under water. Clin Biomech. 2001;16:496-504.
30 Roth A., Miller M., Ricard M., Ritenour D. Comparisons of static and dynamic balance following training in aquatic and land environments. J Sport Rehabil. 2006;15:299-311.
31 Shono T., Fujishima K., Hotta N., et al. Physiological responses and RPE during underwater treadmill walking in women of middle and advanced age. J Physiol Anthropol Appl Human Sci. 2000;19:195-200.
32 Silva L., Valim V., Pessanha A., et al. Hydrotherapy versus conventional land-based exercise for the management of patients with osteoarthritis of the knee: a randomized clinical trial. Phys Ther. 2008;88:12-21.
33 Skinner A., Thomson A., editors. Duffield’s Exercise in Water. London: Bailliere Tindall, 1983.
34 Svedenhag J., Seger J. Running on land and in water: comparative exercise physiology. Med Sci Sports Exerc. 1992;24:1155-1160.
35 Takeshima N., Rogers M., Watanabe E. Water-based exercise improves health-related aspects of fitness in older women. Med Sci Sports Exerc. 2002;33:544-551.
36 Verhagen A., Bierma-Zeinstra S., Cardoso J., et al. Balneotherapy for rheumatoid arthritis. Cochrance Database Syst Rev. (1):2003. CD000518
37 Walker J. Connective tissue plasticity: Issues in histological and light microscopy studies of exercise and aging in articular cartilage. J Orthop Sports Phys Ther. 1991;14:189-212.
38 Whitley J., Schoene L. Comparison of heart rate responses: water walking versus treadmill walking. Phys Ther. 1987;67:1501-1504.
39 Wyatt F., Milam S., Manske R., Deere R. The effects of aquatic and traditional exercise programs on persons with knee osteoarthritis. J Strength Cond Res. 2001;15:337-340.