2 Applied Anatomy of the Normal and Aging Spine
KEY POINTS
The Vertebrae
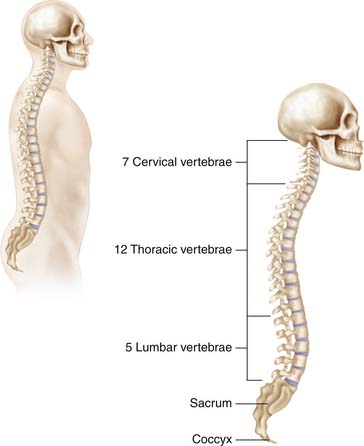
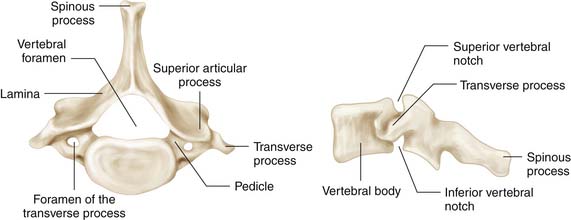
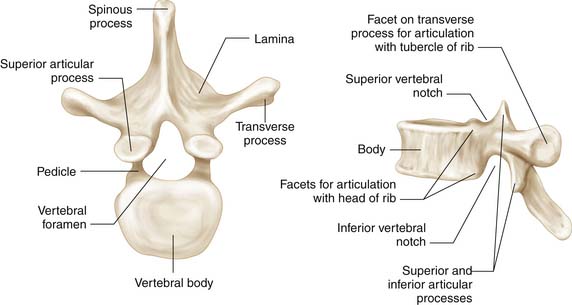
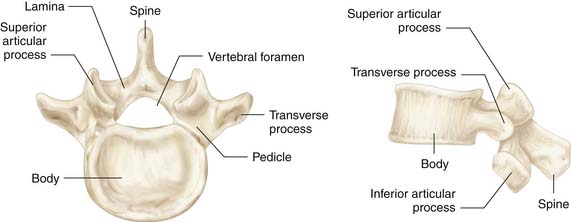
The articulations of the spine are based on synovial and fibrocartilaginous joints. The overall morphology of the vertebral column has a basic similarity, with the exception of the first two cervical vertebrae and the sacrum. A vertebra consists of a cylindrical ventral body of trabecularized cancellous bone and a dorsal vertebral arch that is much more cortical. From the cervical to the lumbar spine, there is a significant increase in the size of the vertebral bodies. An exception is the sixth cervical vertebra, which is usually shorter in height than the fifth and seventh vertebrae. In the thoracic spine, the vertebral body has facets for rib articulations. The posterior aspect of the vertebra starts with a posterior apex or spinous process. This process then flows into flat lamina that arch over the spinal canal and attach to the main body through a cylindrical pillar or pedicle. The transverse processes are found at the junction of the confluence of the laminae and pedicles and extend laterally. In the upper six cervical vertebrae, this component is part of the bony covering of the vertebral arteries. In the thoracic spine, the transverse process articulates with ribs. A mature and robust transverse process is found in the lumbar spine, with the remnant neural arch structure forming a mammillary process (Figure 2-1).
There are points of articulation between the individual vertebral segments between an inferior and ventral facing facet and a superior and dorsal facing facet. It is a diarthrodial, synovial joint. The shape of the facets is coronally oriented in the cervical spine, thus allowing for flexion-extension, lateral bending, and rotation. The facets are sagitally oriented in the lumbar spine and thus resist rotation, while allowing for some flexion and some translational motion.1 Lateral to these joints are mamillary bony prominences upon which muscles can originate and insert.
The portion of the posterior arch most subject to stress by translational motion is the pars interarticularis, which lies between the superior and inferior articular facets of each mobile vertebra. Clinically, fracture of this elongated bony segment in the C2 vertebra results in the hangman’s fracture; in the lower lumbar spine, it results in isthmic spondylolisthesis. The shear forces often result in ventral displacement of the superior articular facet, pedicle, and vertebral body and in maintenance of the attachments of the inferior articular facets and relationships to the lower vertebrae.2 In cadaveric studies, the L5 pars region was particularly susceptible to fracture, given its smaller cross-sectional area of 15 mm2 compared to the L1 and L3 vertebrae, which had over a fourfold increase.3
Cervical Vertebrae
Forward flexion and rotation are largely attributed to the first two cervical vertebrae. The atlas is the first cervical vertebra. It is a bony ring with an anterior and posterior arch connected with relatively two large lateral masses. The superior articular facet of the lateral mass is sloped internally to accommodate the occipital condyles. The inferior portion is sloped externally to articulate with the axis. This inferior articulation allows for rotational freedom while limiting lateral shifts. The posterior arch of C1 is grooved laterally to fit the vertebral arteries as they ascend from the foramen transversarium of C1 to penetrate the posterior atlanto-occipital membrane within 20 to 15 mm lateral to the midline. It is recommended that one remain within 12 mm lateral to midline during dissection of the posterior aspect of the ring.4 The anterior arch connects the two lateral masses, and the anterior tubercle in the most ventral portion is the site of attachment for the longus colli. The ventral side of the anterior arch has a synovial articulation with the odontoid process. The odontoid is restrained at this site with thick transverse atlantal ligaments that attach to the lateral masses (Figure 2-2).
Thoracic Vertebrae
The thoracic vertebrae are heart-shaped and have dual articulations for both ribs as well as for the superior and inferior vertebrae. The transverse diameter of the pedicles is smallest from T3 to T6. At T1, the transverse diameter is larger, with an average of 7.3 mm in men and 6.4 mm in women.5 The first thoracic vertebra has a complete facet on the side of the body for the first rib head and an inferior demifacet for the second rib head. The ninth to twelfth vertebrae have costal articulations with their respective ribs. The last two ribs are smaller and do not attach to the sternum. The thoracic facets are rotated 20 degrees forward on the coronal plane and 60 degrees superiorly on the sagittal plane (Figure 2-3).
Lumbosacral Spine
The lumbar vertebrae are much larger in overall relative proportion. The articular facets are concave and directed approximately 45 degrees medially on the coronal plane. The fourth transverse process tends to be smallest in comparison to the proximal lumbar segments. The fifth transverse process is the most robust (Figure 2-4).
Loss of normal bone within the vertebrae is characteristic of osteoporosis. Primary osteoporosis affects the trabecular bone and is associated with vertebral compression fractures. This is most commonly seen in postmenopausal women, secondary to the sensitivity of the skeleton to estrogen loss.6 Secondary osteoporosis affects the trabecular and cortical bone and is a result of aging and prolonged calcium deficiency.
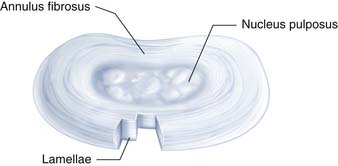
Intervertebral Disc
The fibrocartilaginous nature of the disc provides mobility while maintaining relative structural orientation in the spine. The disc is most commonly divided into the outer annulus fibrosus and the inner nucleus pulposus. The annulus is a concentric mesh that surrounds the nucleus and resists tensile forces. The individual lamella can run obliquely or in a spiral manner in relation to the spinal column. Furthermore, there can be alterations in the direction of the fibers. On a sagittal section, the fibers are pointed slightly to the nucleus pulposus in its proximity, find a vertical orientation moving outward, and then finally bow out at its periphery. The fibers of the nucleus and inner lamellae are interposed into the cancellous bone of the vertebrae. The outer rings penetrate as Sharpey fibers with dense attachments into the verterbral periosteum and the anterior and posterior longitudinal ligaments (Figure 2-5).
Disc degeneration with aging may be a component of the enzymatic activity resulting in an active breakdown of collagen, proteoglycans, and fibronectin. Proteoglycans are diminished with aging.7 Aggrecan is degenerated by various enzymes including cathepsins, matrix metalloproteinases, and aggrecanases. Various mutations in genes can result in a genetic predisposition to disc degeneration, including defects of genes involving vitamin D receptor,8 collagen IX,9 collagen II, and aggrecan.
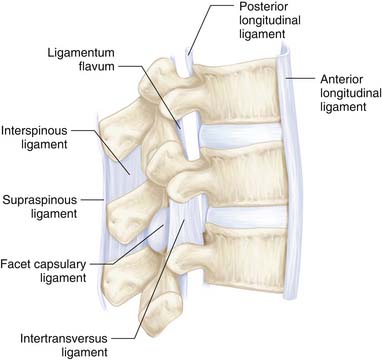
Ligaments
The dorsal lamina articulate with the adjacent segments through the ligamentum flavum, interspinous ligaments, supraspinous ligaments, and intertransverse ligaments. The ligamentum flavum attaches superiorly on the ventral side of the lamina, laterally on the base of the articulating facets, and inferiorly on the superior aspect of the lamina. With aging, the fibers may lose some of the material properties allowing for redundancy and laxity with extension. The ligamentum is a dual-layered structure that flows along both sides of the spine, with a central deficiency. The spinous processes are connected by the oblique interspinous ligaments. The supraspinous ligament connects the apices of the spinous processes. In the cervical spine, this structure is known as the ligamentum nuchae (Figure 2-6).
Intraspinal Ligaments
The anterior longitudinal ligament drapes ventrally from the axis to the sacrum. Superficial layers span multiple segments with the deep layer spanning one spinal segment. In a similar fashion, the posterior longitudinal ligament (PLL) has superficial and deep layers. The deep layer forms a dense central vertical strap with lateral attachments to the disc. Disc protrusions are likely more frequent posterolaterally, secondary to the stronger tether centrally. The peridural membrane is an additional layer between the PLL and the dura.10
The Nerve Roots
Due to the differential growth of the lower segments of the spine in relation to the more cranial segments, the dorsal and ventral roots converge to form the spinal nerve at a more oblique angle toward the intervertebral foramen more distally. In the cervical region, the root and the spinal nerve are at the same level as the disc and the intervertebral foramen. In the lumbar spine, the contributing roots for the nerve are descending to the next lower foramen. A posterolateral disc herniation will affect the nerve root of the respective lower foramen. The spinal nerves typically are in close proximity to the underside of the respective pedicle with narrower margins in the cervical and thoracic spine, and approximately 0.8 to 6.0 mm in the lumbar spine.11 The lumbosacral root ganglia are usually in the intraforaminal region with variations medial and lateral to the foramina.
Anatomic variations can exist, with prevalence from 4% to 14% in various reports. Apart from anomalous levels of origin, there can be interconnections and divisions between nerves both intradural and extradural. Furthermore, the origins of the motor segments from within the ventral horn may allow for contributions to more than one nerve root. The description of the furcal nerve is most commonly applied to the cross-connection between the fourth and fifth lumbar nerve roots.12 This is relevant because of the interconnections of the femoral and obturator nerves of the lumbar plexus to the lumbosacral trunk of the sacral plexus. Compression can result in mixed neurologic findings warranting careful investigation into the underlying pathology.
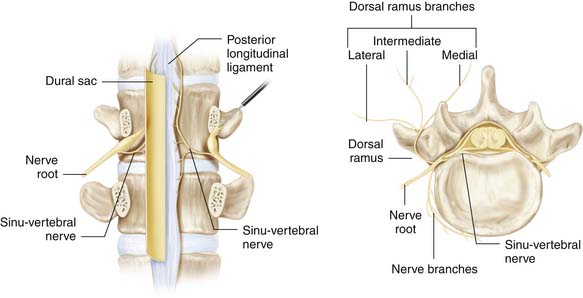
Innervation of the Spine
Emanating from the dorsal root ganglion are rami communicantes that connect to the autonomic ganglion. Sinuvertebral nerves emanate from the rami communicantes close to the spinal nerve and enter back into the spinal canal to divide into branches than may innervate the posterior longitudinal ligament, and possibly, the dorsolateral aspects of the disc.13 Branches may innervate more than one disc level, leading to the nonspecific locations of back pain. Afferent pain fibers are well documented within the histologic analysis of the sinuvertebral nerve. Meningeal fibers of these pain afferents to the ventral aspect of the dura may allow for explanations of back pain with dural distortion. There are intraspinal ligaments of Hoffman which normally tether the dura ventrally. Adhesions in the ventral aspect of the dura can also be acquired, resulting in a more anchored structure susceptible to external compression (Figure 2-7).
Nutritional Support for the Vertebra and Disc
An important variation is the contribution of segmental arteries in the lower thoracic or upper lumbar region to form a large radicular artery of Adamkiewicz, which joins the anterior spinal artery at the level of the conus medullaris.14 Although the disc has no direct arterial supply, disc nutrition is dependent on the diffusion principles, size, and charge of particles. Specifically, the central aspect of the disc has a collective negative charge and is reliant on effective glucose transport from the vasculature of the endplates. Alterations of the precarious nutritional diffusion with age and pathologic processes can initiate a degenerative cascade.
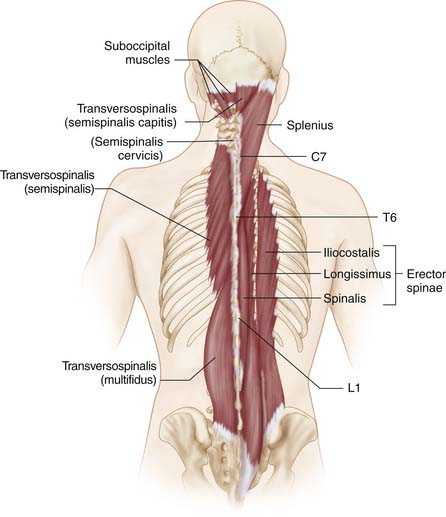
Muscular Anatomy
The muscles that are involved in spinal motion are the largest in the body. The strength of contraction is related to size, fiber type, and number but not limited to these factors. Other factors that may be pertinent to the competence of the muscular system with aging include the effect of neural stimulation, hormones, and conditioning. In the lumbar spine, the spinalis muscle goes between the spinous processes. The multifidi go upward and span two to four segments. The longissimus inserts into the tips of the spinous processes. The iliocostalis inserts into the ribs, and is the most lateral of the posterior lumbar spine intrinsic musculature. The psoas major acts anteriorly and is an important stabilizer in standing and sitting postures. As there are altered use patterns and conditioning with age, important stabilizers are affected, contributing to spinal deformity and altered motion (Figure 2-8).
Pathologic Changes in Aging
With aging, degenerative processes can result in the common pathologies of spinal stenosis, spondylolisthesis, spondylosis, diffuse idiopathic skeletal hyperostosis, and degenerative scoliosis. These changes will be discussed in greater detail in the following chapters. Anatomic changes in the normal joints and perineural structures result in slowly progressive narrowing and compression of the nerves. In the cervical spine, spinal stenosis can be both central and foraminal. Central compression can result in spondylotic myelopathy. Degenerative changes of the facet joints can result in joint laxity and instability. Such pathologic subluxation can give rise to degenerative spondylolisthesis. Arthritic changes can result in mechanical irritation and pain. The cluster of changes in the spinal complex can also result in a scoliotic collapse or adult degenerative scoliosis.
Spinal Stenosis
Local pain and discomfort can result from pathologic changes in the caliber of the spinal canal both centrally and at the foraminal level. Direct mechanical compression of the dural sac and the nerve roots can result in pain and extremity weakness. Pain in the axial region can arise from pathologic changes to the sinuvertebral nerve and posterior primary ramus. Cervical stenosis is most commonly acquired or a result of degenerative spondylotic changes. As the intervertebral discs collapse, the annular bulge can narrow the canal. Furthermore, posterior buckling of the ligamentum flavum can contribute to cord compression. Osteophytes may form both centrally and foraminally, exacerbating the compression. In the lumbar spine, similarly, the stenosis may be both central and/or lateral. Lateral recess stenosis is usually the result of hypertrophy of the superior articulating facet. Foraminal stenosis can result from direct osteophytic growth, facet subluxation, or a vertical disc collapse. Degenerative synovial cysts can often result in compression and can mimic symptoms of spinal stenosis (Figure 2-9).
Spondylolisthesis
Degenerative spondylolisthesis is most commonly a result of the pathologic degeneration of the facet joints. Asymmetry of this degeneration can result in a rotational deformity, along with translation. The L4-5 level is the most common level and can result in entrapment of the L4 root. The root can be caught between the inferior articulating facet of L4 and the body of L5 (Figure 2-10).
Diffuse Idiopathic Skeletal Hyperostosis (DISH)
DISH predominantly affects middle-aged men and is characterized by prolific bone formation around the spine and in the extremities. Associated diseases are diabetes mellitus and gout. The most commonly affected area is the thoracolumbar spine. Often large spurs form on the anterolateral aspect of the vertebral body and flow into a contiguous bar. This is more common on the right side. The most common complaint is stiffness. The facet joints and sacroiliac joints are largely spared in this entity (Figure 2-12).
Degenerative Scoliosis and Kyphosis
Scoliosis, as a subset in patients with no preexisting scoliosis at the time of skeletal maturity, can be a disease of the degenerative cascade, osteoporosis, trauma, and/or iatrogenic from prior surgical intervention. Although any curve has the potential for progression, large curves greater than 60 degrees tend to progress with greater probability. One of the greatest risk factors for kyphosis is osteoporosis and the ensuing compression fracture (Figure 2-11).
1. Van Schaik J.P.J., Verbiest H., et al. The orientation of the laminae and facet joints in the lower lumbar spine. Spine. 1985;10:59-63.
2. Francis W.R., Fielding J.W. Traumatic spondylolisthesis of the axis. Orthop. Clin. North Am.. 1978;9:1011-1027.
3. McColloch J.A., Transfelt E.E. Macnab’s backache. Baltimore: Williams & Wilkins; 1997.
4. Benzel E.C. Anatomic consideration of the C2 pedicle screw placement (letters to the editor). Spine. 21, 1996. 2301–2301
5. Scoles P.V., Linton A.E., Latimer B., et al. Vertebral body and posterior element morphology: the normal spine in middle life. Spine. 1988;13:1082-1086.
6. Riggs B.L., Melton L.J.III. Evidence for two distinct syndromes of involutional osteoporosis. Am. J. Med.. 1983;75:899-901.
7. Lyons G., Eisenstein S.M., Sweet M.B. Biochemical changes in intervertebral disc degeneration. Biochim. Biophys. Acta. 1981;673:443-453.
8. Kawaguchi Y., Kanamori M., Ishihara H., et al. The association of lumbar disc disease with vitamin D receptor gene polymorphism. J. Bone Joint Surg. Am.. 2002;84:2022-2028.
9. Kimura T., Nakata K., Tsumaki N., et al. Progressive generation of the articular cartilage and intervertebral discs: an experimental study in transgenic mice bearing a type IX collagen mutation. Int. Orthop. 1996;20:177-181.
10. Dommissee G. Morphological aspects of the lumbar spine and lumbosacral regions. Orthop. Clin. North Am. 1975;6:163-175.
11. Ebraheim N.A., Xu R., Darwich M., et al. Anatomic relations between the lumbar pedicle and the adjacent neural structures. Spine. 1997;15:2338-2341.
12. McCulloch J.A., Young P.H. Essentials of spinal microsurgery. Philadelphia: Lippincott-Raven; 1998.
13. Humzah M.D., Soames R.W. Human intervertebral disc: structure and function. Anat. Rec.. 1988;229:337-356.
14. Milen M.T., Bloom D.A., Culligan J., et al. Albert Adamkiewicz (1850-1921)—his artery and its significance for the retroperitoneal surgeon. World J. Urol. 1999;17:168-170.