Anticholinergics
Perspective
Anticholinergic agents are divided into three main groups: antimuscarinics, affecting the muscarinic acetylcholine (ACh) receptors; neuromuscular blockers, blocking nicotinic ACh receptors; and ganglionic blockers, affecting ACh sympathetic and parasympathetic nicotinic ganglia (Fig. 150-1). This chapter refers only to antimuscarinic agents, and the terms anticholinergic and antimuscarinic are used interchangeably. The prototypical anticholinergic agents are the naturally occurring belladonna alkaloids—atropine (racemic mixture of D– and L-hyoscyamine), scopolamine (L-hyoscine), and hyoscyamine—found in many plant members of the Solanaceae family. Atropine is the major alkaloid of Atropa belladonna, an important pharmaceutical source of that drug. Datura stramonium, or Jimson weed, contains scopolamine, grows in almost all climates, and is often involved in plant-related belladonna poisoning.1,2 Other plants that have antimuscarinic agents include henbane (Hyoscyamus niger) and mandrake (Mandragora officinarum).
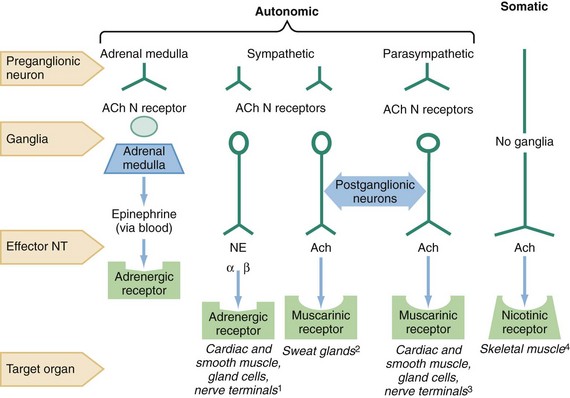
Figure 150-1 The sites of nicotinic and muscarinic acetylcholine receptors. Ach, acetylcholine; N, nicotinic; NE, norepinephrine; NT, neurotransmitter.1 Causing tachycardia, hypertension, diaphoresis, mydriasis.2 Causing diaphoresis.3 Causing bradycardia, diarrhea, diaphoresis, urination, miosis, bronchospasm, bronchorrhea, lacrimation, salivation.4 Causing fasciculations.
Physicians (and Renaissance-era Italian women) have used belladonna alkaloids for hundreds of years as mydriatics (Box 150-1).3 The belladonna alkaloids and their synthetic congeners are used today as pupillary dilators (atropine, homatropine, tropicamide, cyclopentolate), as antispasmodics (dicyclomine), to decrease gastric secretions (propantheline), to prevent motion sickness (scopolamine), and to treat asthma (ipratropium, tiotropium) and bradycardia (atropine). Atropine and glycopyrrolate are used to dry airway secretions and to block vagal responses to laryngoscopy and endotracheal intubation. The significant central nervous system (CNS) effects of scopolamine also facilitate the induction of perioperative amnesia.
Many other drugs with anticholinergic activity cause side effects in addition to their main pharmacologic action. Some examples are the tricyclic antidepressants, drugs that are structurally related to the tricyclics (such as carbamazepine and cyclobenzaprine), the phenothiazines, and the antihistamines (H1 blockers). In patients with significant toxicity from any of these drugs, these antimuscarinic side effects provide valuable diagnostic clues (Box 150-2; see also Box 150-1).
Accidental and intentional poisoning by anticholinergic drugs occurs commonly with over-the-counter antihistamines such as diphenhydramine and cyclizine. Poisoning from drugs with only anticholinergic effects rarely results in death when adequate supportive care is provided. However, the impaired sweating with an anticholinergic overdose may result in fatal hyperthermia in the agitated or seizing patient.4,5 Patients taking therapeutic doses of anticholinergics are at increased risk of death from heatstroke when they are exercising or exposed to heat. Finally, deaths from trauma or drowning caused by perceptual distortion are also attributed to anticholinergics.6
Poisonings with belladonna alkaloids are common. Deliberate ingestions of seeds or teas brewed from the leaves of the ubiquitous Jimson weed for their hallucinogenic effects occur in many cultures,1 and it remains popular as a recreational stimulant among teenagers.7 Commercially available herbal teas contaminated with atropine and smoking of herbal cigarettes cause inadvertent poisoning.8,9 A cluster of poisonings occurred in Oslo when the difficult-to-detect drug scopolamine was disguised as Rohypnol tablets and given to known illicit drug users.10 The tainting of heroin with anticholinergics leading to a complex toxidrome has also been reported in drug users in several eastern states of the United States.4,5 Although the reason for this tainting was never explained, it may have been an attempt to reproduce an old combination of scopolamine and morphine used in obstetric anesthesia called the twilight sleep.11
Principles of Disease
Atropine and atropine-like drugs inhibit muscarinic ACh receptors both centrally and peripherally at the end-organ sites of the parasympathetic nervous system (see Fig. 150-1). Although the term anticholinergic is commonly used, the most precise term to describe the pharmacologic action of these drugs is antimuscarinic. These drugs do not block the effects of ACh on nicotinic receptors in the ganglia or at the neuromuscular junction, with the exception of the synthetic quaternary amines. Muscarinic receptors affect smooth muscle function in the eye, intestinal tract, and bladder and also regulate sweat, salivary, and mucosal gland activity. Cardiac cholinergic receptors associated with vagal nerve fibers affect heart rate and conduction through the atrioventricular node. Muscarinic receptors in the CNS appear to be involved in new information storage, general perceptive and cognitive functions, and motor coordination.12–14
Generalized inhibition of muscarinic receptors by atropine results in tachycardia, pupillary dilation, loss of accommodation, inability to sweat, drying of mucosal surfaces, gastrointestinal paralysis, and urinary retention. In the CNS, muscarinic inhibition causes stimulation, seizures, coma, choreoathetosis, memory impairment, and perceptual and cognitive dysfunction.12–17 The mnemonic “hot as a hare, red as a beet, blind as a bat, dry as a bone, mad as a hatter” describes the more florid manifestations of the antimuscarinic syndrome. With increasing doses, CNS depression follows the initial CNS stimulation. In adults, CNS depression can predominate without an initial CNS stimulation. Antimuscarinic effects occur in a predictable order with salivation, bronchial secretions, and sweating suppressed first, followed by mydriasis and tachycardia. The organs least sensitive to antimuscarinic drugs are the bladder and the gastrointestinal tract. Patients with anticholinergic toxicity often do not exhibit all the signs and symptoms described in the toxidrome. Instead, many patients present with just a few symptoms; tachycardia (68% of patients) and decreased secretions (75% of patients) are the most common.18
Poisoning by anticholinergics has been reported after ingestion, smoking, and topical absorption.19 Systemic absorption is common after use of eye drops.19,20 Anticholinergics are generally rapidly absorbed and widely distributed throughout the body. However, with plant and seed ingestions or after an overdose, the onset of symptoms can be delayed. Prolonged anticholinergic toxicity is also reported, which may indicate slowed gastrointestinal absorption of the ingested drug or residual drug in the gastrointestinal tract.21,22
Clinical Presentation
The diagnosis of acute anticholinergic poisoning is suggested by the characteristic anticholinergic toxidrome. Mydriasis, dry mucous membranes, absence of axillary sweat, flushed skin, fever, tachycardia, decreased or absent bowel sounds, and urinary retention suggest muscarinic blockade.18,23 The patient is often alert but may be nonsensical, agitated, or incoherent. Violent agitation is rare. Visual hallucinations are common. Central motor effects may be manifested as myoclonus or choreoathetoid movements. Children are more sensitive than adults to the CNS stimulant effects and more likely to have seizures, typically preceded by signs of CNS irritability or depression. Massive ingestions in both adults and children are associated with coma and cardiovascular collapse,22,24 but wide-complex tachycardia due to sodium channel blockade is rare.25,26
The agitated patient may have an elevated temperature due to increased motor activity and impaired heat exchange. In such cases, death from hyperthermia supersedes the morbidity of the anticholinergic drug itself.27 The hyperthermic patient may have hepatic necrosis, rhabdomyolysis with myoglobinuric renal failure, cerebral edema, and disseminated intravascular coagulation.
Patients with chronic anticholinergic poisoning are more difficult to diagnose. They have organic mental symptoms that may be incorrectly attributed to dementia or underlying psychiatric illness.16,28,29 Significant peripheral anticholinergic signs are typically absent. Two likely settings for chronic anticholinergic toxicity are (1) the elderly patient taking anticholinergic drugs for parkinsonism or other chronic diseases and (2) the psychiatric patient receiving neuroleptic therapy and prescribed another anticholinergic drug.12,16 Resolution of behavioral or cognitive symptoms after withdrawal of the offending drug confirms the diagnosis.
Differential Diagnosis
The differential diagnosis of the comatose, psychotic, delirious, or febrile patient is extensive, and serious alternative diagnoses should be considered and excluded.30,31 Diagnoses to consider include toxicity and withdrawal from a variety of drugs, metabolic disorders, CNS infections, and other neurologic diseases.31
The physical examination findings can help refine this broad differential diagnosis. Patients with excessive sympathetic stimulation from cocaine or amphetamines exhibit hyperthermia, tachycardia, and dilated pupils but classically have diaphoresis compared with the “dry” anticholinergic effects; diaphoresis can be absent in severely dehydrated patients. Marked nystagmus, diaphoresis, small pupils, and extreme agitation suggest phencyclidine poisoning. Lithium or monoamine oxidase inhibitor toxicity usually has tremors and significant hyper-reflexia or clonus, which are not characteristic of anticholinergic poisoning.32 Patients with serotonin syndrome often present with agitation but often have diaphoresis, rigidity, and a tremor that is more prominent in the lower extremities.33,34 Neuroleptic malignant syndrome and malignant hyperthermia can also be similar, but these patients display rigidity and hyperthermia as prominent physical examination features.34,35
Except for sinus tachycardia, electrocardiographic abnormalities from a pure anticholinergic overdose are unusual and suggest a cardiotoxic agent, such as a tricyclic antidepressant, carbamazepine, or a phenothiazine, for which the antimuscarinic side effects are of less importance. Rarely, diphenhydramine ingestions have been associated with sodium channel blockade, causing prolonged QRS on the electrocardiogram and possibly leading to ventricular arrhythmias.25,26 Peaked T waves from hyperkalemia due to rhabdomyolysis can occur.36
Diagnostic Strategies
Mildly symptomatic patients with well-established histories and consistent symptoms do not need routine laboratory testing. In the seriously poisoned patient, serum electrolyte values, renal function, and creatine kinase and glucose concentrations may be abnormal. Arterial blood gas measurements document disorders of oxygenation and ventilation and detect metabolic acidosis but usually are not needed. Blood glucose and oxygen saturation measurements are important in the initial assessment of any patient with altered mental status.37–39 An electrocardiogram should be performed early because certain anticholinergic medications, such as tricyclic antidepressants and diphenhydramine, can block sodium channels to cause QRS widening.40
Management
In the emergency department, many patients with anticholinergic poisoning have no clear history of exposure. The patient is often unable to provide a history because of the delirium. The diagnosis is often suggested solely on the basis of the findings on physical examination fitting the antimuscarinic/anticholinergic toxidrome (Box 150-3). The general treatment of these poisoned patients proceeds with consideration of the broader differential diagnosis of the acutely agitated, febrile, or comatose patient and meticulous supportive care.30
Agitation
The need for titrated sedation with a benzodiazepine, cooling, and hydration takes precedence over specific toxicologic concerns in critically ill patients. Physical restraint alone is detrimental and is used only briefly to permit rapid pharmacologic intervention.41 Agitation is best controlled by titration of intravenous benzodiazepines. Intramuscular lorazepam or midazolam should be used only when an intravenous route is not available and attempts to establish that route may result in needle sticks or other injuries. Haloperidol and droperidol may facilitate intravenous placement but theoretically lower the seizure threshold and have additional anticholinergic effects.42,43 Pharmacologic restraint prevents self-injury, worsening of the hyperthermia, and development of myoglobinuric renal failure from muscle injury as well as permits a more thorough physical examination and diagnostic procedures. Paralysis and intubation should be undertaken if other clinical imperatives (e.g., refractory shock, coingestants) require it.
Hyperthermia
Deaths of agitated patients can be associated with unrecognized hyperthermia. The patient’s core temperature should be measured with a flexible rectal probe. Aggressive temperature reduction with ice water or evaporative cooling with mist and fans should be the first priority in the severely hyperthermic patient. Antipyretic agents and simple cooling blankets are ineffective. Intravenous benzodiazepines should be used to prevent shivering, which can hinder adequate cooling. Dantrolene, a drug that decreases rigidity caused by abnormal calcium fluxes in muscle tissue in malignant hyperthermia, has no role in treatment of hyperthermic patients who do not have muscle rigidity.44
Drug Removal
Routine decontamination of the patient with anticholinergic poisoning is not necessary.45 Activated charcoal does adsorb diphenhydramine and phenothiazines; however, there is no evidence that it improves outcome, and it should not be used to decontaminate patients poisoned with a relatively benign drug.45
Physostigmine as an Antidote
The role of physostigmine in the management of anticholinergic overdoses has been controversial.46 In the absence of anticholinergic blockade, physostigmine itself can precipitate cholinergic excess, causing seizures, muscle weakness, bradycardia, bronchoconstriction, lacrimation, salivation, bronchorrhea, vomiting, and diarrhea. Even in documented cases of anticholinergic toxicity, seizures have been reported after the rapid administration of physostigmine.47 Asystole has occurred after physostigmine for tricyclic antidepressant overdose,48 so a conduction delay (QRS > 0.10 second) or suggestion of tricyclic antidepressant ingestion is generally considered a contraindication to physostigmine administration.49,50
Physostigmine reverses delirium in 87% and agitation in 96% of patients with anticholinergic overdose.51 Whereas benzodiazepines controlled agitation in 24% of patients, they do not reverse delirium.51 Physostigmine is primarily used for patients with anticholinergic signs and symptoms with suspected anticholinergic overdose who have a normal QRS on the electrocardiogram.23,52 The reversal of coma or severe agitation and normalization of mental status obviate the need for further diagnostic evaluation.
Physostigmine has been used to treat anticholinergic delirium with a host of pharmaceuticals for which the anticholinergic effect is a side effect and not the main pharmacologic action of that drug and with other ingestions, such as benzodiazepines, γ-hydroxybutyrate (GHB), and narcotics. Currently, its use for nonanticholinergic presentations is not recommended and potentially dangerous.53,54 Relative contraindications include reversible airway disease, peripheral vascular disease, bladder or intestinal obstruction, intraventricular conduction delays, and atrioventricular blocks. There is little information on its use during pregnancy.
Disposition
Patients who are alert or have symptoms and vital signs that normalize during observation in the emergency department do not require hospital admission. The onset of symptoms after most anticholinergic ingestions is rapid, and 4 hours of observation is adequate to exclude significant toxicity in an asymptomatic patient. Patients who have ingested D. stramonium seeds should be observed for 8 hours because of delayed absorption.55 Predischarge measures can include psychiatric assessment; exclusion of other toxins, including documentation of a nontoxic acetaminophen level; and assessment of a child’s home situation.
References
1. Spina, SP, Taddei, A. Teenagers with Jimson weed (Datura stramonium) poisoning. CJEM. 2007;9:467–468.
2. Al-Shaikh, AM, Sablay, ZM. Hallucinogenic plant poisoning in children. Saudi Med J. 2005;26:118–121.
3. Nickalls, RW, Nickalls, EA. The first use of physostigmine in the treatment of atropine poisoning. A translation of Kleinwachter’s paper entitled “Observations on the effect of Calabar bean extract as an antidote to atropine poisoning.”. Anaesthesia. 1988;43:776–779.
4. Hamilton, RJ, et al. A descriptive study of an epidemic of poisoning caused by heroin adulterated with scopolamine. J Toxicol Clin Toxicol. 2000;38:597–608.
5. Wang, HE. Street drug toxicity resulting from opiates combined with anticholinergics. Prehosp Emerg Care. 2002;6:351–354.
6. Gowdy, JM. Stramonium intoxication: Review of symptomatology in 212 cases. JAMA. 1972;221:585–587.
7. Bronstein, AC, et al. 2009 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 27th Annual Report. Clin Toxicol (Phila). 2010;48:979–1178.
8. Cheng, SW, et al. Anticholinergic poisoning from a large dose of Scopolia extract. Vet Hum Toxicol. 2002;44:222–223.
9. Göpel, C, Laufer, C, Marcus, A. Three cases of angel’s trumpet tea–induced psychosis in adolescent substance abusers. Nord J Psychiatry. 2002;56:49–52.
10. Vallersnes, OM, et al. Epidemic of poisoning caused by scopolamine disguised as Rohypnol tablets. Clin Toxicol (Phila). 2009;47:889–893.
11. From the Centers for Disease Control and Prevention. Scopolamine poisoning among heroin users—New York City, Newark, Philadelphia, and Baltimore, 1995 and 1996. JAMA. 1996;276:92–93.
12. Katz, IR, et al. Screening for cognitive toxicity of anticholinergic drugs. J Clin Psychiatry. 1985;46:323–326.
13. Tune, L, et al. Association of anticholinergic activity of prescribed medications with postoperative delirium. J Neuropsychiatry Clin Neurosci. 1993;5:208–210.
14. Tune, LE, et al. Serum levels of anticholinergic drugs and impaired recent memory in chronic schizophrenic patients. Am J Psychiatry. 1982;139:1460–1462.
15. Drachman, DA. Memory and cognitive function in man: Does the cholinergic system have a specific role? Neurology. 1977;27:783–790.
16. Moreau, A, Jones, BD, Banno, V. Chronic central anticholinergic toxicity in manic depressive illness mimicking dementia. Can J Psychiatry. 1986;31:39–41.
17. Potamianos, G, Kellett, JM. Anti-cholinergic drugs and memory: The effects of benzhexol on memory in a group of geriatric patients. Br J Psychiatry. 1982;140:470–472.
18. Patel, RJ, et al. Prevalence of autonomic signs and symptoms in antimuscarinic drug poisonings. J Emerg Med. 2004;26:89–94.
19. Alpay, A, et al. The local vasoconstriction of infant’s skin following instillation of mydriatic eye drops. Eur J Clin Pharmacol. 2010;66:1161–1164.
20. Lim, DL, Batilando, M, Rajadurai, VS. Transient paralytic ileus following the use of cyclopentolate-phenylephrine eye drops during screening for retinopathy of prematurity. J Paediatr Child Health. 2003;39:318–320.
21. Fahy, P, et al. Serial serum drug concentrations and prolonged anticholinergic toxicity after benztropine (Cogentin) overdose. Am J Emerg Med. 1989;7:199–202.
22. Freedberg, RS, et al. Cardiogenic shock due to antihistamine overdose. Reversal with intra-aortic balloon counterpulsation. JAMA. 1987;257:660–661.
23. Sopchak, CA, et al. Central anticholinergic syndrome due to Jimson weed physostigmine: Therapy revisited? J Toxicol Clin Toxicol. 1998;36:43–45.
24. Krenzelok, EP, Anderson, GM, Mirick, M. Massive diphenhydramine overdose resulting in death. Ann Emerg Med. 1982;11:212–213.
25. Jang, DH, et al. Status epilepticus and wide-complex tachycardia secondary to diphenhydramine overdose. Clin Toxicol (Phila). 2010;48:945–948.
26. Sharma, AN, et al. Diphenhydramine-induced wide complex dysrhythmia responds to treatment with sodium bicarbonate. Am J Emerg Med. 2003;21:212–215.
27. Torline, RL. Extreme hyperpyrexia associated with central anticholinergic syndrome. Anesthesiology. 1992;76:470–471.
28. Moore, AR, O’Keeffe, ST. Drug-induced cognitive impairment in the elderly. Drugs Aging. 1999;15:5–28.
29. Leentjens, AF, van der Mast, RC. Delirium in elderly people: An update. Curr Opin Psychiatry. 2005;18:325–330.
30. Jones, J, Dougherty, J, Cannon, L. Diphenhydramine-induced toxic psychosis. Am J Emerg Med. 1986;4:369–371.
31. Perrone, J, Band, RA, Mathew, R. Agitation complicating procedural sedation with etomidate. Am J Emerg Med. 2006;24:511–512.
32. Waring, WS. Management of lithium toxicity. Toxicol Rev. 2006;25:21–30.
33. Isbister, GK, Buckley, NA, Whyte, IM. Serotonin toxicity: A practical approach to diagnosis and treatment. Med J Aust. 2007;187:361–365.
34. Nisijima, K, Shioda, K, Iwamura, T. Neuroleptic malignant syndrome and serotonin syndrome. Prog Brain Res. 2007;162:81–104.
35. Hadad, E, Weinbroum, AA, Ben-Abraham, R. Drug-induced hyperthermia and muscle rigidity: A practical approach. Eur J Emerg Med. 2003;10:149–154.
36. Akhtar, S, et al. Atropine-induced rhabdomyolysis: An uncommon and potentially fatal adverse drug reaction. J Postgrad Med. 2010;56:42–43.
37. Olsen, RQ, Regis, JT. Delirious deficiency. Lancet. 2010;376:362.
38. Lee, DC, et al. Low plasma thiamine levels in elder patients admitted through the emergency department. Acad Emerg Med. 2000;7:1156–1159.
39. SF, Li, et al. Vitamin deficiencies in acutely intoxicated patients in the ED. Am J Emerg Med. 2008;26:792–795.
40. Boehnert, MT, Lovejoy, FHJr. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med. 1985;313:474–479.
41. Hick, JL, Smith, SW, Lynch, MT. Metabolic acidosis in restraint-associated cardiac arrest: A case series. Acad Emerg Med. 1999;6:239–243.
42. Holubek, WJ, Dodge, K, Hoffman, RS. Management of acute undifferentiated agitation in the emergency department. Acad Emerg Med. 2006;13:585.
43. Rossi, J, Swan, MC, Isaacs, ED. The violent or agitated patient. Emerg Med Clin North Am. 2010;28:235–256.
44. Amsterdam, JT, et al. Dantrolene sodium for treatment of heatstroke victims: Lack of efficacy in a canine model. Am J Emerg Med. 1986;4:399–405.
45. Buckley, NA, Eddleston, M. The revised position papers on gastric decontamination. Clin Toxicol (Phila). 2005;43:29–30.
46. Teoh, R, Page, AV, Hardern, R. Physostigmine as treatment for severe CNS anticholinergic toxicity. Emerg Med J. 2001;18:412.
47. Newton, RW. Physostigmine salicylate in the treatment of tricyclic antidepressant overdosage. JAMA. 1975;231:941–943.
48. Pentel, P, et al. Late complications of tricyclic antidepressant overdose. West J Med. 1983;138:423–424.
49. Schmidt, W, Lang, K. Life-threatening dysrhythmias in severe thioridazine poisoning treated with physostigmine and transient atrial pacing. Crit Care Med. 1997;25:1925–1930.
50. Suchard, JR. Assessing physostigmine’s contraindication in cyclic antidepressant ingestions. J Emerg Med. 2003;25:185–191.
51. Burns, MJ. The pharmacology and toxicology of atypical antipsychotic agents. J Toxicol Clin Toxicol. 2001;39:1–14.
52. Arnold, SM, et al. Two siblings poisoned with diphenhydramine: A case of factitious disorder by proxy. Ann Emerg Med. 1998;32:256–259.
53. Rupreht, J, et al. Physostigmine versus naloxone in heroin-overdose. J Toxicol Clin Toxicol. 1983;21:387–397.
54. Bania, TC, et al. Jimson weed extract as a protective agent in severe organophosphate toxicity. Acad Emerg Med. 2004;11:335–338.
55. Salen, P, et al. Effect of physostigmine and gastric lavage in a Datura stramonium–induced anticholinergic poisoning epidemic. Am J Emerg Med. 2003;21:316–317.








