Chapter 79 Anterior Knee Problems After Anterior Cruciate Ligament Reconstruction
Anterior Knee Problems Related To the Graft
Patellar Tendon and Hamstring Tendon Autografts
The impact of patellar tendon graft harvesting on knee symptoms is well documented. An increased incidence of anterior knee problems such as pain and loss of sensitivity was found in patients in whom a patellar tendon autograft was harvested from the “healthy” contralateral knee, and therefore this procedure should be avoided because additional problems and morbidity are transferred onto the healthy contralateral knee.1
The gold standard thus far for ACL reconstruction is the mid-third bone–patellar tendon–bone (BPTB) autograft. However, it has been associated with significant (in 40% to 60% of patients) anterior knee symptoms,2–7 and therefore the use of four-strand hamstring tendon graft is increasing in popularity because these problems seem to be less frequent.
In the literature, results are conflicting in the comparison of the two most popular grafts (patellar and hamstring tendon) regarding the incidence of anterior knee pain.8–10
However, three meta-analyses concluded that ACL reconstructed knees with patellar tendon are more prone to developing anterior knee symptoms and extension deficit than the hamstring tendon group.11–13
In a study with a long-term follow-up,7 kneeling pain was found to persist even at 7 years postoperatively and was more common and more severe in the patellar tendon group (54%) than the hamstring tendon group (20%). Similarly, the incidence of donor site symptoms in any form was more than doubled in the patellar tendon group compared with the hamstring tendon group, and the incidence of extension deficit increased over time in the patellar tendon group, probably secondary to development of osteoarthritic changes.7
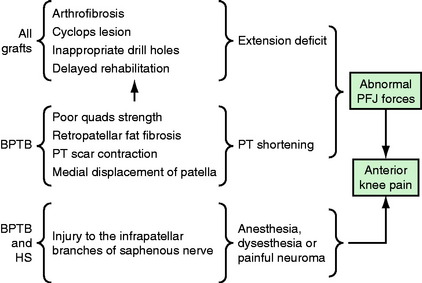
But what causes anterior knee problems after patellar tendon harvest?
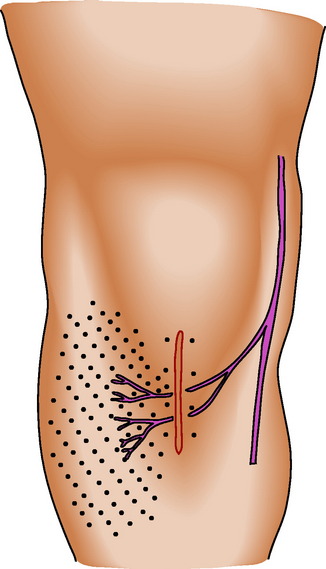
Harvesting trauma, patellar tendonitis, tendon changes during the repair process of the tendon gap, vascular damage of the retropatellar fat pad, and proprioceptive loss of the extension mechanism are all possible causes.14 Patellar tendon shortening is another important factor for development of anterior knee pain. It has been demonstrated with a magnetic resonance imaging (MRI) study15 that significant patellar tendon shortening (with a mean of 9.7%) occurs after harvesting BPTB graft compared with the contralateral nonoperated control knee 1 year after ACL reconstruction (Fig. 79-1).
In contrast, harvesting of hamstring tendons resulted in a nonsignificant shortening of the patellar tendon of 2.6% (Fig. 79-2). Using an Insall-Salvati ratio less than 0.74 as the MRI criterion for patella baja diagnosis,16 12.5% of the patients in the BPTB group and 3% in the hamstring group were found to develop patella baja after surgery. This shortening was not of clinical importance, as it was not associated with anterior knee pain in the short-term follow-up. However, one other study with longer follow-up (average 7 years) has clearly shown that severity of patellofemoral joint arthritis and anterior knee symptoms correlate with the amount of patellar tendon shortening17 (Fig. 79-3).
Central patellar tendon harvesting has been found to cause a slight medial displacement of the patella,18 and this alteration in position causes high contact forces in the medial patellofemoral joint.14 A solution to this may be the use of the medial third of the patellar tendon, which does not influence the patellofemoral angle and causes an insignificant lateral patellar displacement.18
Anterior knee pain does occur after hamstring ACL reconstruction, despite the fact that the anterior structures of the knee remain intact. The reason for this is not clear, but it is known that the patellofemoral joint can be the source of pain after almost any surgery to the knee, even if the patellofemoral extension mechanism is not directly involved. The incidence of anterior knee pain after hamstring graft for ACL reconstruction in the literature is less than 23%.19–22 Evaluation of the pain with diagrams has shown that it is more diffuse and is not related to the skin incision for tendon harvesting or tibial tunnel drilling.19 In contrast, anterior knee pain after patellar tendon harvesting is more well localized, and palpation reveals trigger points that are usually over the inferior pole of the patella or the tibial tuberosity or above the patellar tendon donor site.14,23
There are conflicting reports in the literature on whether grafting the patella and tibial tunnel bone defects after BPTB harvesting reduces23,24 or does not reduce25 the incidence of anterior knee symptoms. There is also a report that patella grafting increases the incidence of painful spurs at the inferior pole of the patella.26 Similar arguments exist regarding whether suturing the patellar tendon gap facilitates tendon healing or is a cause of patellar tendon shortening.27 Patellar fracture is another important issue unique in BPTB grafts, and its incidence varies from 0.2%28 to 2.3%.29
Patellar tendon rupture is another rare complication that may occur after patellar tendon harvest. Devascularization and an alteration in tendon healing and remodeling are possible causes of this complication.30
Central Quadriceps Tendon
In a recent study, less than 10% of patients with quadriceps tendon graft suffered anterior knee pain in various activities, and only 6% complained of kneeling pain.31 Donor site irritation over the proximal patellar border was observed in several patients but did not last more than 6 months, and quadriceps strength 1 year postoperatively was comparable with that of other autografts in the literature.31 The risk of patellar fracture must be lower than that of patellar tendon graft because the bone in the proximal patellar pole is more dense.32 Injury of infrapatellar branches of the saphenous nerve is not a problem because the incision does not cross them.
Allografts
Some studies comparing patellar tendon autograft versus allograft in ACL reconstruction failed to show any difference in the incidence of anterior knee pain between the two groups.33,34 Others found a significant reduction in anterior knee pain with allografts, such as 14% versus 46%35 and 14.4% versus 55.8%.36
In a study comparing patellar tendon autograft versus allograft with long-term follow-up (5 years), it was found that the autograft group experienced more pain during the first 3 postoperative months, which relates to the larger incision required and the resulting bony defect.37 At 2 and 5 years there was no difference in the pain. Moreover, both in the short and long terms, there was no difference in the range of motion and quadriceps strength.
However, incision site complaints (tenderness, irritation, numbness) are less common in the allograft group when compared with the autologous BPTB group.33
Anterior Knee Problems Related to the Procedure
The infrapatellar branch of the saphenous nerve has two main trunks, superior and inferior,38 coursing laterally and slightly distally, respectively (Fig. 79-4). Incisions close to the tibial tubercle and over the patellar tendon may damage these branches with consequent anesthesia, dysesthesia, or painful neuroma formation.39 A significant correlation exists between disturbed anterior knee sensitivity and subjective anterior knee pain as well as discomfort during knee walking.40,41 Moreover, there is an association between injury of these sensory branches and development of reflex sympathetic dystrophy.37 The importance of infrapatellar branches can be appreciated by reports of prepatellar neuralgia after direct blows to the anterior knee.42,43
Patients should be informed of these potential complications. The area of anesthesia is variable but always lateral to the incision. It is not only the incision for graft harvesting that puts in danger these sensory branches; the incision for the medial portal can damage them as well.38,39 Therefore some propose a horizontal rather than vertical incision for the portals to minimize the risk of nerve damage.38 Another maneuver to avoid damage of these nerves is placing the anterior midline skin incision with the knee held in 90 degrees of flexion. In this way the inferior branch moves farther distally and the risk of inadvertent damage is lessened.38
When harvesting patellar tendon autograft with a small midline incision, every effort should be made to identify and protect these sensory nerve branches. Alternative techniques have been described for subcutaneous patellar tendon harvesting using two horizontal incisions,44 one horizontal incision at the midlevel of the patellar tendon,23 and two vertical41 incisions. This way the infrapatellar branches are avoided, making these incisions less likely to become a source of pain.
Injury to these branches can occur not only during patellar tendon harvesting but with hamstring tendon as well. Anterior knee sensory changes were found to be as high as 50% (at a minimum of 24 months postoperatively) following hamstring ACL reconstruction.19 The inadvertent injury of the sensory nerve branches may occur during the skin incision, the dissection for the tendons, tendon stripping (as the saphenous nerve courses superficial to gracilis), and tibial tunnel drilling.19 However, it seems that the more distal the location of the area of disturbed sensitivity (as occurs after hamstring tendon harvesting), the less discomfort will result.45 In contrast with patellar tendon harvesting, the area of sensory changes is more proximal and thus more bothersome.
Proper placement of the drill holes at the isometric point is a prerequisite to achieve full range of motion postoperatively.40 It has been found in a study that after BPTB ACL reconstruction, patients with patellofemoral joint arthritis tended to have more anterior placement of the femoral tunnel and more posterior placement of the tibial tunnel than those without patellofemoral joint arthritis.17
Arthrofibrosis after ACL reconstruction may result from an exaggerated inflammatory response, synovitis, or a sympathetic algodystrophy and will cause range-of-motion deficit.10
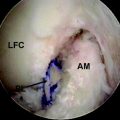
Formation of a “Cyclops” lesion is another reason for extension deficit and anterior knee pain.46 This lesion is usually formed anterolaterally to the tibial tunnel placement of the graft. Arthroscopic débridement of the nodule can improve extension.
Anterior Knee Problems Related to Rehabilitation
An operation performed too early (i.e., before regaining full range of motion) is a well-known cause of postoperative range of motion deficit. For this reason we support a rather delayed reconstruction, not less than 2 months after the injury, to allow for posttraumatic synovitis to settle or the knee to regain full range of motion without effusion.47,48
Reduced strength and loss of range of motion are correlated with anterior knee pain after ACL reconstruction using all kinds of grafts.49 Thereby every effort should be made postoperatively to achieve full range of motion and regain quadriceps and hamstrings muscle strength. Loss of hyperextension can be a significant cause of anterior knee discomfort after ACL reconstruction.50–53 The reason for anterior knee symptoms in loss of extension is the resultant increase of patellofemoral joint reaction forces. It is not only loss of extension that can cause anterior knee symptoms but loss of flexion as well, although this has been more controversial.52,54 Patients with both flexion and extension deficits have more anterior knee pain than patients with an extension deficit alone.40 The reason for anterior knee symptoms in loss of flexion is the decreased muscle strength in both flexor and extensor mechanisms40 (Fig. 79-5).
1 Mastrokalos DS, Springer J, Siebold R, et al. Donor site morbidity and return to the preinjury activity level after anterior cruciate ligament reconstruction using ipsilateral and contralateral patellar tendon autograft: a retrospective, nonrandomized study. Am J Sports Med. 2005;33:85-93.
2 Corry I, Webb M, Clingeleffer A, et al. Arthroscopic reconstruction of the anterior cruciate ligament. Am J Sports Med. 1999;27:444-454.
3 Eriksson K, Anderberg P, Hamberg P, et al. A comparison of quadruple semitendinosus and patellar tendon grafts in reconstruction of the anterior cruciate ligament. J Bone Joint Surg. 2001;83B:348-354.
4 Shaieb M, Kan D, Chang S, Marumoto J, et al. Prospective randomised comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:214-220.
5 Feller JA, Webster KE. A randomised comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564-573.
6 Forster MC, Forster IW. Patellar tendon or four-strand hamstring? A systematic review of autografts for anterior cruciate ligament reconstruction. Knee. 2005;12:225-230.
7 Roe J, Pinczewski LA, Russell VJ, et al. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction differences and similarities. Am J Sports Med. 2005;33:1337-1345.
8 Spindler KP, Kuhn JE, Freedman KB, et al. Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring. Does it really matter? A systematic review. Am J Sports Med. 2004;32:1986-1995.
9 Herrington L, Wrapson C, Matthews M, et al. Anterior cruciate ligament reconstruction, hamstring versus bone-patella tendon-bone grafts: a systematic literature review of outcome from surgery. Knee. 2005;12:41-50.
10 Biau DJ, Tournoux C, Katsahian S, et al. Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. Br J Med. 2006;332:995-1001.
11 Yunes M, Richmond JC, Engels EA, et al. Patellar versus hamstring tendons in anterior cruciate ligament reconstruction: a metaanalysis. Arthroscopy. 2001;17:248-257.
12 Freedman KB, D’Amato MJ, Nedeff DD, et al. Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2-11.
13 Thompson J, Harris M, Grana WA. Patellofemoral pain and functional outcome after anterior cruciate ligament reconstruction: an analysis of the literature. Am J Orthop. 2005;34:396-399.
14 Breitfuss H, Frohlich R, Povacz P, et al. The tendon defect after anterior cruciate ligament reconstruction using the midthird patellar tendon: a problem for the patellofemoral joint? Knee Surg Sports Traumatol Arthrosc. 1996;3:194-198.
15 Hantes M, Zachos V, Bargiotas K, et al. Patellar tendon length after anterior cruciate ligament reconstruction. A comparative magnetic resonance imaging study between patellar and hamstring tendon autografts. Knee Surg Sports Traumatol Arthrosc. 2007;15:712-719.
16 Shabshin N, Schweitzer ME, Morrison WB, et al. MRI criteria for patella alta and baja. Skeletal Radiol. 2004;33:445-450.
17 Jarvela T, Paakkala T, Kannus P, et al. The incidence of patellofemoral osteoarthritis and associated findings 7 years after anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. Am J Sports Med. 2001;29:18-24.
18 Moebius U, Georgoulis AD, Papageorgiou CD, et al. Alterations of the extensor apparatus after anterior cruciate ligament reconstruction using the medial third of the patellar tendon. Arthroscopy. 2001;17:953-959.
19 Spicer DD, Blagg SE, Unwin AJ, et al. Anterior knee symptoms after four-strand hamstring tendon anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2000;8:286-289.
20 Sgaglione NA, Del Pizzo W, Fox JM, et al. Arthroscopically assisted anterior cruciate ligament reconstruction with the pes anserine tendons. Comparison of results in acute and chronic ligament deficiency. Am J Sports Med. 1993;21:249-256.
21 Otero AL, Hutcheson LA. A comparison of the doubled semitendinosus/gracilis and central third of the patellar tendon autografts in arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 1993;9:143-148.
22 Corry IS, Webb JM, Clingeleffer AJ, et al. Arthroscopic reconstruction of the anterior cruciate ligament. A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. Am J Sports Med. 1999;27:444-454.
23 Tsuda E, Okamura Y, Ishibashi Y, et al. Techniques for reducing anterior knee symptoms after anterior cruciate ligament reconstruction using a bone-patellar tendon-bone autograft. Am J Sports Med. 2001;29:450-456.
24 Muellner T, Kaltenbrunner W, Nikolic A, et al. Shortening of the patellar tendon after anterior cruciate ligament reconstruction. Arthroscopy. 1998;14:592-596.
25 Boszotta H, Prunner K. Refilling of removal defects: impact on extensor mechanism complaints after use of a bone-tendon-bone graft for anterior cruciate ligament reconstruction. Arthroscopy. 2000;16:160-164.
26 Kohn D, Sander-Beuermann A. Donor-site morbidity after harvest of a bone-tendon-bone patellar tendon autograft. Knee Surg Sports Traumatol Arthrosc. 1994;2:219-223.
27 Brandsson S, Faxen E, Eriksson BI, et al. Closing patellar tendon defects after anterior cruciate ligament reconstruction: absence of any benefit. Knee Surg Sports Traumatol Arthrosc. 1998;6:82-87.
28 Viola R, Vianello R. Three cases of patella fracture in 1,320 anterior cruciate ligament reconstructions with bone-patellar tendon-bone autograft. Arthroscopy. 1999;15:93-97.
29 Brown CH. ACL Surgery. Graft options: patellar tendon, hamstrings tendons, quadriceps tendon, and allografts. In: Sim FH, editor. American Academy of Orthopaedic Surgeons 2001 instructional course lectures. Park Ridge, IL: American Academy of Orthopaedic Surgeons; 2001:447-458.
30 Marumoto JM, Mitsunaga MM, Richardson AB, et al. Late patellar tendon ruptures after removal of the central third for anterior cruciate ligament reconstruction: a report of two cases. Am J Sports Med. 1996;24:698-701.
31 Lee S, Seong SC, Jo H, et al. Outcome of anterior cruciate ligament reconstruction using quadriceps tendon autograft. Arthroscopy. 2004;20:795-802.
32 West RV, Harner CD. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005;13:197-207.
33 Peterson RK, Shelton WR, Bomboy AL. Allograft versus autograft patellar tendon anterior cruciate ligament reconstruction: a 5-year follow-up. Arthroscopy. 2001;17:9-13.
34 Shelton WR, Papendick L, Dukes AD. Autograft versus allograft anterior cruciate ligament reconstruction. Arthroscopy. 1997;13:446-449.
35 Bach BRJr, Aadalen KJ, Dennis MG, et al. Primary anterior cruciate ligament reconstruction using fresh-frozen, nonirradiated patellar tendon allograft: minimum 2-year follow-up. Am J Sports Med. 2005;33:284-292.
36 Gorschewsky O, Klakow A, Riechert K, et al. Clinical comparison of the Tutoplast allograft and autologous patellar tendon (bone-patellar tendon-bone) for the reconstruction of the anterior cruciate ligament: 2- and 6-year results. Am J Sports Med. 2005;33:1202-1209.
37 Poehling GG, Pollock FEJr, Koman LA. Reflex sympathetic dystrophy of the knee after sensory nerve injury. Arthroscopy. 1988;4:31-35.
38 Tifford CD, Spero L, Luke T, et al. The relationship of the infrapatellar branches of the saphenous nerve to arthroscopy portals and incisions for anterior cruciate ligament surgery. An anatomic study. Am J Sports Med. 2000;28:562-567.
39 Mochida H, Kikuchi S. Injury to infrapatellar branch of saphenous nerve in arthroscopic knee surgery. Clin Orthop. 1995;320:88-94.
40 Kartus J, Magnusson L, Stener S, et al. Complications following arthroscopic anterior cruciate ligament reconstruction. A 2–5-year follow-up of 604 patients with special emphasis on anterior knee pain. Knee Surg Sports Traumatol Arthrosc. 1999;7:2-8.
41 Kartus J, Ejerhed L, Sernert N, et al. Comparison of traditional and subcutaneous patellar tendon harvest. A prospective study of donor site-related problems after anterior cruciate ligament reconstruction using different graft harvesting techniques. Am J Sports Med. 2000;28:328-335.
42 Detenbeck LC. Infrapatellar traumatic neuroma resulting from dashboard injury. J Bone Joint Surg. 1972;54A:170-172.
43 Gordon GC. Traumatic prepatellar neuralgia. J Bone Joint Surg. 1952;34B:41-44.
44 Mishra AK, Fanton GS, Dillingham MF, et al. Patellar tendon graft harvesting using horizontal incisions for anterior cruciate ligament reconstruction. Arthroscopy. 1995;11:749-752.
45 Eriksson K. On the semitendinosus in anterior cruciate ligament reconstructive surgery. Stockholm, Sweden: Karolinska Institutet[thesis.], 2001.
46 Jackson DW, Schaefer PK. Cyclops syndrome: loss of extension following intra-articular anterior cruciate ligament reconstruction. Arthroscopy. 1990;6:171-178.
47 Shelbourne KD, Wilckens JH. Current concepts in anterior cruciate ligament rehabilitation. Orthop Rev. 1990;19:957-964.
48 Aglietti P, Buzzi R, D’Andria S, et al. Patellofemoral problems after intraarticular anterior cruciate ligament reconstruction. Clin Orthop. 1993;288:195-204.
49 Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17:971-980.
50 Harner CD, Irrgang JJ, Paul J, et al. Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20:499-506.
51 Irrgang JJ, Harner CD. Loss of motion following knee ligament reconstruction. Sports Med. 1995;19:150-159.
52 Sachs RA, Daniel DN, Stone ML, et al. Patellofemoral problems after anterior cruciate ligament reconstruction. Am J Sports Med. 1989;17:760-765.
53 Shelbourne KD, Trumper R. Preventing anterior knee pain after anterior cruciate ligament reconstruction. Am J Sports Med. 1997;25:41-47.
54 Stapleton TR. Complications in anterior cruciate ligament reconstructions with patellar tendon grafts. Sports Med Arthrosc Rev. 1997;5:156-162.