Chapter 61 Anterior Cruciate Ligament Injury Combined with Medial Collateral Ligament, Posterior Cruciate Ligament, and/or Lateral-Side Injury
Introduction
A knee dislocation injury is a rare but potentially devastating injury. The definition of knee dislocation includes the grossly unstable knee, with a minimum of two of the four major knee ligaments injured, regardless of a reduced joint line.1 Some authors suggest that any combined anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) injuries be considered a knee dislocation,2 although knee dislocations have been described without cruciate injury.3–5 The injury is commonly attributed to high-velocity motor vehicle accidents and low-velocity sports injuries, with the rate of knee dislocation reported to be 0.001% to 0.013% of all knee injuries.6–8 This may represent an underestimation of this devastating injury, as some knee dislocations spontaneously reduce before the patient receives a physical examination and the patient may suffer other physical injuries that require medical attention.1
Commonly, a knee dislocation involves injury to the ACL, PCL, and either the medial collateral ligament (MCL) or the lateral-side structures of the knee. Of knee dislocations, associated medial-side tears represent approximately 90% of all the injuries, whereas lateral-side injuries represent approximately 10% of the knee dislocation injuries.9
We see almost 10 times more knee dislocations involving the medial side than we do involving the lateral side. Nonoperative treatment of knee dislocations involving the lateral side usually results in a grossly unstable knee and causes severe functional disability for the patient. Because of these occurrences, acute reconstruction of all injured structures with all knee dislocations has been advocated; this recommendation has included knee dislocations involving the medial side.10,11 This approach has resulted in many stable but stiff knees after surgery.
Ligament Healing
Anterior Cruciate Ligament
The ACL does not generally heal after injury.12–15 Lyon et al13 found in a histological study that the cellular composition of the ACL resembles that of fibrocartilage and that it has a poor capacity to heal. The injured ACL pulls completely apart as opposed to tearing interstitially, which diminishes the potential for healing. An incompetent ACL represents a complete tear. Yao et al16 found in a series of 21 partial ACL tears evaluated with magnetic resonance imaging (MRI) and confirmed with arthroscopic evaluation that the ACL tears showed ACL fibers in continuity and the ACL resisted probing. They also found that the MRI was less sensitive for partial tears compared with complete tears. MRI can occasionally demonstrate interstitial femoral-sided tears. These tears may heal spontaneously and can result in functional stability.
Posterior Cruciate Ligament
In contrast to the ACL, PCL injuries have the potential for intrinsic healing (Fig. 61-1). Evaluation with MRI of acute PCL injuries has been found to be 99% to 100% sensitive and specific in documenting acute PCL tears. In contrast, MRI evaluation of chronic PCL laxity is less accurate than that of acute injury because the PCL appears to be healed even when the patient has laxity.17–20 Shelbourne et al19 evaluated 40 patients who had acute PCL injuries with MRI at the time of the acute injury and again at a mean of 3.2 years after injury. Twenty-three patients had isolated PCL tears, and 17 patients had combined PCL and additional ligament injury. The healing of partial and complete tears was graded with MRI. The results showed 37 of 40 PCLs to be healed with continuity. All partial tears and most complete (19 of 22) PCL tears regained continuity. Twelve of 12 combined PCL/MCL injuries healed. In two patients with acute ACL, PCL, and MCL injuries, the MCL and PCL healed without treatment. Location, severity, and associated ligament injuries did not affect healing. The healed PCL demonstrated abnormal morphology in 25 of the 37 cases on follow-up.19 In a recent follow-up study at a mean of 4.6 years after knee dislocations to the lateral side, the PCL in 16 of 16 patients appeared healed on the MRI and no patient had more than 1+ laxity upon examination.21 Tewes et al20 evaluated follow-up MRIs on 13 patients with high-grade PCL injury at an average of 20 months postinjury. Their results showed 10 of 13 patients (77%) had regained MRI continuity of the PCL, although with an abnormal appearance. They could not correlate functional or clinical status with degree of clinical laxity.20 The time to obtain healing after acute PCL injury is yet unknown. However, Shelbourne et al22 described a firm endpoint and a painless posterior drawer at follow-up examination of acute PCL injuries about 2 weeks postinjury.
Medial Collateral Ligament
The MCL is an extraarticular ligament with an intrinsic ability to heal. In contrast to the ACL, the MCL is made up of fibroblast-type cells with the potential to heal.13 Animal studies indicate the MCL can heal with scar tissue with strength and stiffness similar to that of native MCL.23,24 This intrinsic capacity to heal has also been observed clinically with isolated MCL injury.25,26 The ability of injured ligaments to heal may also be affected by extrinsic factors such as surgical apposition, immobilization, and early protected range of motion.27,28 Prolonged immobilization may adversely affect the mechanical properties by loss of collagen fiber orientation and decreased strength of the bone ligament junction.29,30 Long et al31 found in a rabbit model that the ultimate load of rabbit MCL treated with intermittent passive motion was four times greater than immobilized ligament, with improvements in matrix organization and collagen concentration. The location of MCL injury has also been found to affect healing potential. Proximal tears, which have a more pronounced blood supply, tend to heal rapidly and may lead to knee stiffness. Distal tears seem to heal more slowly, and patients usually do not develop range of motion problems.32,33
Clinical Examination
Listening carefully to the patient explain how the injury occurred and the position of the limb at the time of the injury combined with a thorough physical examination should allow the physician to arrive at a diagnosis. Evaluation of the uninjured extremity will establish a baseline and gain the patient’s confidence. Initial evaluation may be difficult because the patient will probably have pain, swelling, muscle spasm, and limited knee motion and will be apprehensive. The physician should have a high index of suspicion based on the history of the patient’s injury, especially with a multi-ligamentous knee injury, because 50% of knee dislocations will reduce before evaluation1,32 and capsular tears may prevent the appearance of significant effusion. The complications that arise from not recognizing associated injuries can be devastating. Close follow-up and reexamination are helpful. In addition, imaging studies and vascular surgery consultation may be needed.
Clinical assessment of the ACL can be done using the Lachman test. A positive Lachman test, performed properly, is diagnostic of ACL disruption because the ACL prevents contribution from secondary stabilizers to anterior stability.34,35
The PCL is the primary restraint to posterior instability in the knee.26To determine PCL deficiency, the involved knee should be compared with the noninvolved extremity to determine the proper relationship of the tibia to the femoral condyles. When the PCLs are intact, the anteromedial proximal tibia usually rests 1 cm anterior to the distal femoral condyles with 90 degrees of knee flexion. In patients with PCL deficiency, the anteromedial tibia will “sag” posteriorly in relationship to the femoral condyles.36,37
The most sensitive test for evaluating the PCL is the posterior drawer test at 90 degrees of flexion.38,39 Rubinstein et al39 found the posterior drawer test in conjunction with palpating anterior tibial step-off to be 96% accurate, 90% sensitive, and 99% specific, with an interobserver grade agreement of 81% in diagnosing PCL insufficiency. The posterior drawer test with internal tibial rotation can also provide assessment of medial structures. Posterior tibial translation with posterior drawer testing should decrease with internal rotation of the tibia as the medial capsular structures tighten. In combined PCL/medial-side injury, this reduction in the posterior laxity is lost.
It is difficult to perform ligamentous testing on a patient with an acute knee dislocation. In particular, PCL laxity is difficult to determine because the patient may not be able to bend his or her knee to 90 degrees of flexion. Although MRI is helpful in determining the status of the PCL, treatment should not be determined based on MRI findings. It is important to remember that complete grade III PCL injuries can heal with continuity and little or no laxity when left in situ.19,20 Predictable healing of the torn PCL is more important than any laxity in the healed PCL. The fact that the PCL will heal with continuity is important to our treatment philosophy for knee dislocation injuries.
An MCL injury is diagnosed and graded by physical examination. Palpation along the ligament will localize the site of the injury, which is critical to know in order to determine the treatment and rehabilitation process. The MCL is the primary medial restraint to valgus stress at 30 degrees of knee flexion. Valgus stress testing is preformed at 30 degrees of flexion to isolate the MCL and then again at 0 degrees of flexion to assess the contribution of capsular structures as well as the cruciate ligaments. In greater degrees of knee extension the ACL, PCL, posterior capsule, and posterior oblique ligaments assume a greater responsibility in preventing medial joint opening.40 Grading of MCL injury is based on tenderness, laxity, and the presence of a firm endpoint. A grade I injury has tenderness, no laxity with valgus stress testing at 30 degrees of knee flexion, and a firm endpoint. A grade II injury is similar but reveals some medial laxity and the presence of a firm endpoint. A grade III injury represents a complete disruption of the MCL with no palpable endpoint on valgus stress testing.
A lateral-side knee injury usually appears differently than an isolated ACL injury. The knee has a mild effusion, but the lateral side of the leg appears swollen with ecchymosis from the lateral capsule avulsion that allows the hemarthrosis to dissipate into the lateral leg (Fig. 61-2, A, B). Lateral stability is evaluated with varus stress applied to the knee at 0 and 30 degrees of flexion. Grade 1 laxity involves tenderness over the lateral structures but no laxity and a good endpoint. Grade 2 lateral laxity involves tenderness and increased laxity with varus stress, but a good endpoint is felt. Grade 3 laxity involves tenderness and increased laxity with varus stress, and no endpoint is felt.
Associated Neurovascular Injury
Vascular injury with high-velocity knee dislocation has been reported to be as high as 40% in some series.41 Shelbourne et al in a series of low-velocity sports injuries found a vascular injury rate of 4.8% (1 of 21).42 Peroneal nerve injuries have been reported in 14% to 35% of knee dislocations. Most, if not all, are associated with lateral-side injury. In a series of low-velocity sports injuries, four of 21 (19%) patients presented with peroneal nerve injury.43 All were associated with lateral-side injury. It should be emphasized that if the lateral side is injured, the peroneal nerve should be closely evaluated. Conversely, if the peroneal nerve is injured, careful evaluation of lateral-side structures is advised.
Imaging
Radiographic examination of the injured extremity is imperative to rule out associated fracture or joint subluxation. Initial views should include posteroanterior, lateral, and Merchant views.44 In the delayed setting, a flexed, 45-degree weight-bearing view will give more accurate assessment of tibiofemoral joint space.45 Additionally, a PCL avulsion fracture may be detected.
MRI may provide important information about the injured soft tissues and their site of disruption. MRI can also be used to radiographically evaluate the healing of the PCL. Although healing of the PCL on MRI correlates with clinical healing, there may be residual clinical laxity.19,20
Treatment Philosophy (Principles)
Our treatment principles have evolved over the last 22 years after observing and studying the outcome of injuries to individual structures and their potential to heal when left in situ, as well as the effects of the injuries in combination with other ligament injuries in the knee. Nonoperative treatment of knee dislocations has yielded mixed results, with some patients reporting residual, disabling laxity.10,46 Acute operative repair of multi-ligament injuries can provide knee stability but frequently results in permanent stiffness, primarily when injury to the medial side is involved. Previously, direct repair of all ligaments was advocated, but as ACL reconstruction techniques were developed, there was a shift toward repair of all injured structures in conjunction with ACL reconstruction. As PCL reconstruction techniques have improved, many authors now advocate combined ACL/PCL reconstructions in the acute setting.47,48
We propose different treatment approaches depending on the degree and the combination of injured structures. The initial treatment approach is based on recognizing that the PCL and MCL can heal without surgery, whereas the ACL and lateral structures generally do not. Thus most ligament injuries do not require acute surgery, and in most cases immediate surgery is not desirable because of the increased incidence of arthrofibrosis and long-term loss of motion.49 An understanding of the healing response of individual structures provides an explanation for potential postoperative stiffness associated with acute surgery. The goal of treatment is to provide the patient with a functionally stable knee with full range of motion. In observing a young, athletically active population, we have found that patients who have a stable but stiff knee have disability and would prefer a knee with full range of motion that would allow a functional activity level. Once accurate diagnosis has been made and associated injuries evaluated, the treatment plan for the knee is formalized.
Combined Anterior Cruciate Ligament/Posterior Cruciate Ligament/Medial Collateral Ligament Injury
In 1990, we began using cast immobilization to totally limit valgus stress. The patient is initially placed in a cylinder cast with 20 degrees of flexion, and weight bearing is encouraged. The goal is to prevent valgus stress, allow healing of the MCL, and prevent stress deprivation of the joint surface.29 The cast is changed weekly in order to evaluate ligament healing. Gentle valgus stress testing is performed to check for an endpoint. Once stability is achieved in the MCL with a stable endpoint and the patient is pain free, the cast is discontinued. Typically, proximal MCL injuries take 2 weeks to develop an endpoint, and distal injuries require 4 to 5 weeks of serial casting. Casting usually allows the PCL to heal with a good endpoint on posterior drawer examination. This treatment approach usually results in no medial laxity, acceptable posterior laxity, and ACL deficiency.
Sometimes the ACL and PCL stability will be sufficient to totally avoid surgery. Most of the time, PCL laxity will have improved and be 2+ or less. In a prospective natural history study of patients with acute isolated PCL injuries, the outcome of patients with 1+ PCL laxity did not have better overall subjective, objective, or radiographic results than patients with 2+ PCL laxity.22 Additionally, current surgical techniques have failed to reproducibly restore normal PCL stability.50,51 Therefore surgery to reduce PCL laxity from 2+ to 1+ should not allow improved function or less development of degenerative changes. Until operative techniques can reliably obtain normal PCL stability, and given that 1+ posterior laxity has not been shown to provide better function than 2+ laxity, we recommend nonoperative treatment of PCL laxity of 2+ or less.
We do not recommend a combined ACL/PCL reconstruction be performed acutely because of the high incidence of knee stiffness.52–55 If a PCL reconstruction is indicated, the reconstruction should be delayed until the knee has little swelling and good range of motion and the patient has good leg control. Additionally an antiembolism stocking and continuous passive range of motion device can be used to prepare the patient for surgery. To further reduce operative trauma, we prefer using autogenous patellar tendon graft from the contralateral knee. If ACL deficiency becomes symptomatic, an ACL reconstruction can be performed electively at a later date.
When high-grade MCL laxity is present and fails to heal with the previously described treatment plan, a number of options are available. Multiple longitudinal perforations in the MCL can be done to stimulate healing. We have found this useful in tightening the medial side without compromising postoperative range of motion. Additional options include recessing the femoral attachment, advancing the distal attachment, and reefing the MCL, all of which will retension the MCL.56–58
Combined Anterior Cruciate Ligament, Posterior Cruciate Ligament, and Lateral-Side Knee Injury
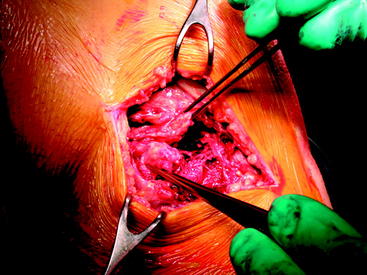
A lateral side knee injury requires semi-urgent treatment. We strive to balance being able to obtain range of motion and decrease swelling with the ability to repair the torn lateral structures. The torn lateral structures retract proximally and begin to heal en masse within 3 weeks after injury (Fig. 61-3).
Some surgeons advise to dissect and repair individual structures.59,60 We prefer to reattach the en masse tissue versus dissecting out each torn structure to take advantage of the body’s healing reaction from the injury.21 This approach is similar to that described by Aglietti et al.56
Lateral-Side Repair
A longitudinal skin incision is made laterally from distal to proximal between the tibial tubercle and fibular head. A pseudomembrane forms over the injured structures when the surgery is performed within 3 weeks of the injury. The underlying structures can be identified once the pseudomembrane is entered. The iliotibial band is usually intact, and the injured structures begin just posterior to the iliotibial band where the lateral capsule attaches to the tibia. A bare area of bone will be exposed on the proximal lateral tibia and fibular head because of the injury. The bare area is easily exposed with blunt finger dissection. The retracted tissue that has healed en masse can be easily seen. The tissue, instead of being dissected into individual structures, is left en masse and repaired back to the lateral capsule attachment site.21 An Ethibond (Ethicon, Somerville, NJ) suture is passed through the tissue mass by using a modified Kesslar stitch. One suture is passed anteriorly, and another is passed posteriorly. The bony attachment site on the tibia is freshened with a curette or bur. A suture anchor is placed if repair to the fibular head is also required. The mass of tissue is advanced to the normal capsular attachment site and fixed with a stable (Fig. 61-4).
Postoperative Rehabilitation
The patient remains in bed with the operative leg in a continuous passive motion (CPM) machine for the first week after surgery. The continuous passive motion machine is set to move from 0 degrees of extension to 30 degrees of flexion. The patient performs specific range of motion exercises 4 to 5 times a day to increase extension and flexion in the knee. If the lateral gastrocnemius muscle was intact, then full extension is allowed; if the muscle was injured, then extension is limited to 0 degrees for 3 to 4 weeks to allow healing. Patients are allowed to weight bear as able but are required to wear the immobilizer for 1 to 2 weeks postoperatively, when good quadriceps muscle control is usually achieved. The rehabilitation process is similar to the rehabilitation after ACL reconstruction.61 Patients must obtain full knee range of motion equal to the contralateral knee, good leg control, and a normal gait before beginning aggressive strengthening exercises. The return to activities is individualized to each patient’s goals and lifestyle.
Summary
1 Good L, Johnson RJ. The dislocated knee. J Am Acad Orthop Surg. 1995;3:284-292.
2 Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma. 1997;11:525-529.
3 Bratt HD, Newman AP. Complete dislocation of the knee without disruption of both cruciate ligaments. J Trauma. 1993;34:383-389.
4 Cooper DE, Speer KP, Wickiewicz TL, et al. Complete knee dislocation without posterior cruciate ligament disruption: a report of four cases and review of the literature. Clin Orthop. 1992;284:228-233.
5 Shelbourne KD, Pritchard J, Rettig AC, et al. Knee dislocations with intact PCL. Orthop Rev. 1992;21:607-611.
6 Kannus P, Jarvinen M. Non-operative treatment of acute knee ligament injuries. Am J Sports Med. 1990;9:244-260.
7 Treiman GS, Yellin AE, Weaver FA, et al. Examination of the patient with a knee dislocation: the case for selective arteriography. Arch Surg. 1992;127:1056-1061.
8 Walker DN, Hardison RR, Schenck RC. A baker’s dozen of knee dislocations. Am J Knee Surg. 1994;7:117-124.
9 Shelbourne KD, Carr DR. Combined anterior and posterior cruciate and medial collateral ligament injury: nonsurgical and delayed surgical treatment. Instr Course Lect. 2003;52:413-418.
10 Kennedy JC. Complete dislocation of the knee joint. J Bone Joint Surg. 1963;45A:889-904.
11 Sisto DJ, Warren RF. Complete knee dislocation. A follow-up study of operative treatment. Clin Orthop. 1985;198:94-101.
12 Hefti FL, Kress A, Fasel J, et al. Healing of transacted anterior cruciate ligament in the rabbit. J Bone Joint Surg. 1991;73A:373-383.
13 Lyon RM, Akeson WH, Amiel D, et al. Ultrastructural differences between the cells of the medial collateral and anterior cruciate ligaments. Clin Orthop. 1991;272:279-286.
14 McDaniel WJJr, Dameron TBJr. Untreated anterior ruptures of the cruciate ligament: a follow-up study. J Bone Joint Surg. 1980;62A:310-322.
15 Warren RF, Marshall JL. Injuries of the anterior cruciate and medial collateral ligaments of the knee: a long term follow-up of 86 cases. Part II. Clin Orthop. 1978;136:197-211.
16 Yao L, Gentili A, Petrus L, et al. Partial ACL rupture: an MRI diagnosis. Skeletal Radiol. 1995;24:247-251.
17 Fischer SP, Fox JM, Del Pizzo W, et al. Accuracy of diagnosis from magnetic resonance imaging of the knee. A multicenter analysis of 1014 patients. J Bone Joint Surg. 1991;73A:2-10.
18 Polly DWJr, Callaghan JJ, Sikes RA, et al. The accuracy of selective magnetic resonance imaging compared with the findings of arthroscopy of the knee. J Bone Joint Surg. 1988;70A:192-198.
19 Shelbourne KD, Jennings RW, Vahey TN. Magnetic resonance imaging of posterior cruciate ligament injuries: assessment of healing. Am J Knee Surg. 1999;12:209-213.
20 Tewes DP, Fritts HM, Fields RD, et al. Chronically injured posterior cruciate ligament. Magnetic resonance imaging. Clin Orthop. 1997;335:224-232.
21 Shelbourne KD, Haro MS, Grag T. Knee dislocation with lateral side injury: Results of an En Masse Surgical repair technique of the lateral side. Am J Sports Med. 2007;35:1005-1117.
22 Shelbourne KD, Davis TJ, Patel DV. The natural history of acute isolated non-operatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1999;27:276-283.
23 Anderson DR, Weiss JA, Takai S, et al. Healing of the medial collateral ligament following a triad injury: a biomechanical and histologic study of the knee in rabbits. J Orthop Res. 1992;10:485-495.
24 Woo SLY, Inoue M, McGurk-Burleson E, et al. Treatment of the medial collateral ligament injury: II. Structure and function of canine knees in response to differing treatment regimes. Am J Sports Med. 1987;15:22-29.
25 Fetto JF, Marchall JL. Medial collateral ligament injuries of the knee. Clin Orthop. 1978;132:206-218.
26 Petermann J, von Garrel T, Gotzen L. Non-operative treatment of acute medial collateral ligament lesions of the knee joint. Knee Surg Sports Traumatol Arthrosc. 1993;1:93-96.
27 Clayton ML, Miles JS, Abdulla M. Experimental investigations of ligamentous healing. Clin Orthop. 1968;61:146-153.
28 Tipton CM, Vailas AC, Matfhes RD. Experimental studies on influence of physical activity on ligaments, tendons and joints: a brief report. Acta Med Scand Suppl. 1986;711:157-168.
29 Amiel D, Akeson WH, Harwood FL, et al. Stress deprivation effect on metabolic turnover of the medial collateral ligament collagen. A comparison between 9- and 12-week immobilization. Clin Orthop. 1983;172:265-270.
30 Woo SLY, Horibe S, Ohland KJ, et al. The response of ligaments to injury. Healing of the collateral ligaments. In: Daniel DM, editor. Knee ligaments: structure, function, injury and repair. New York: Raven Press; 1990:351-364.
31 Long ML, Frank C, Schachar NS. The effects of motion on normal and healing ligaments. Trans Orthop Res Soc. 1982;7:43.
32 DeLee JC, Riley MB, Rockwood CA. Acute straight lateral instability of the knee. Am J Sports Med. 1983;11:404-411.
33 Robins AJ, Newman AP, Burks RT. Postoperative return of motion in anterior cruciate ligament and medial collateral ligament injuries. The effect of medial collateral ligament rupture location. Am J Sports Med. 1993;21:20-25.
34 Jonsson T, Althoff B, Peterson L, et al. Clinical diagnosis of ruptures of the anterior cruciate ligament: a comparative study of the Lachman test and the anterior drawer sign. Am J Sports Med. 1982;10:100-102.
35 Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4:84-93.
36 Clancy WG, Shelbourne KD, Zoellner GB, et al. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure. J Bone Joint Surg. 1983;65A:310-322.
37 Insall JN, Hood RW. Bone block transfer of the medial head of the gastrocnemius for posterior cruciate insufficiency. J Bone Joint Surg. 1982;64A:691-699.
38 Hughston JC, Andrews JR, Cross MJ, et al. Classification of knee ligament instabilities. Part I: the medial compartment and cruciate ligaments. J Bone Joint Surg. 1976;58A:159-172.
39 Rubinstein RAJr, Shelbourne KD, McCarroll FR, et al. The accuracy of the clinical examination in the setting of the posterior cruciate ligament injuries. Am J Sports Med. 1994;22:550-557.
40 Grood ES, Noyes FR, Butler DL, et al. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg. 1981;63A:1257-1269.
41 Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg. 1977;59A:236-239.
42 Shelbourne KD, Porter DA, Clingman JA, et al. Low velocity knee dislocation. Orthop Rev. 1991;20:995-1004.
43 Shelbourne KD, Klootwyk TE. Low-velocity knee dislocation with sports injuries. Treatment principles. Clin Sports Med. 2000;19:443-456.
44 Merchant AC, Mercer RL, Jocobsen RH, et al. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg. 1975;56A:1391-1396.
45 Rosenberg TD, Paulos LE, Parker RD, et al. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg. 1988;70A:1479-1483.
46 Meyers MH, Harvey JP. Traumatic dislocation of the knee joint: a study of eighteen cases. J Bone Joint Surg. 1971;53A:16-29.
47 Almekinders LC, Logan TC. Results following treatment of traumatic dislocations of the knee joint. Clin Orthop. 1992;284:203-207.
48 Dedmond BT, Almekinders LC. Operative versus nonoperative treatment of knee dislocations. A meta-analysis. Am J Knee Surg. 2001;14:33-38.
49 Frassica FJ, Sim FH, Staeheli JW, et al. Dislocation of the knee. Clin Orthop. 1991;263:200-205.
50 L’Insalata JC, Harner CD. Treatment of acute and chronic posterior cruciate ligament deficiency: new approaches. Am J Knee Surg. 1996;9:185-193.
51 Noyes FR, Barber-Westin SD. Treatment of complex injuries involving the posterior cruciate and posterolateral ligaments of the knee. Am J Knee Surg. 1996;9:200-214.
52 Harner CD, Irrgang JJ, Paul J, et al. Loss of motion after anterior cruciate ligament reconstruction. Am J Sports Med. 1992;20:449-506.
53 Mohtadi NGH, Webster-Bogaert S, Fowler PJ. Limitation of motion following anterior cruciate ligament reconstruction. A case-control study. Am J Sports Med. 1991;19:620-625.
54 Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292-299.
55 Shelbourne KD, Wilckens JH, Mollabashy A, et al. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19:332-336.
56 Aglietti P, Zaccherotti G, DeBiase P. Combined knee ligament injuries. In: Tria AJ, editor. Ligaments of the knee. New York: Churchill Livingstone; 1995:207-259.
57 Maynard MJ, Warren RF. Surgical and reconstructive technique for knee dislocation. In: Jackson DW, editor. Techniques in orthopaedic surgery—reconstructive knee surgery. New York: Raven Press; 1995:161-183.
58 Stroud CC, Reider B. Medial and posteromedial ligament injuries of the knee. In: Garrett WE, Speer KP, Kirkendall DT, editors. Principles and practice of orthopaedic sports medicine. Baltimore: Lippincott, Williams & Wilkins; 2000:663-674.
59 Harner CD, Waltrip RL, Bennett CH, et al. Surgical management of knee dislocations. J Bone Joint Surg. 2004;86A:262-273.
60 Kurtz CA, Sekiya JK. Treatment of acute and chronic anterior cruciate ligament-posterior cruciate ligament-lateral side knee injuries. J Knee Surg. 2005;18:228-239.
61 Shelbourne KD, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year followup. Am J Sports Med. 1997;25:786-795.