CHAPTER 297 Anterior Cervical Instrumentation
Pathologic processes that compromise the biomechanical integrity of the cervical spine ultimately require management that incorporates rigid internal fixation of the vertebral column. The application of anteriorly based screw-plate systems to facilitate reconstruction of the cervical spine is a relatively recent innovation in the history of spinal surgery and has evolved during the last 20 years. This instrumentation confers immediate segmental stability along the vertebral column and ensures patient compliance by locating the orthosis internally. Its use has been associated with improved fusion and postoperative comfort;1 those who receive the implants tend to return to work more rapidly than patients who do not.2–8 Consequently, anterior cervical screw-plate systems have become an integral part of the surgical armamentarium for achieving vertebral interbody arthrodesis within the subatlantal (C2-C7) cervical spine after procedures involving diskectomy or corpectomy. The past 2 decades have witnessed an intense evolution within this domain of instrumentation, and several anterior cervical screw-plate systems are commercially available. In pursuing the clinical ideal of product versatility, enhanced fusion rates, and ease of application, each new generation of anterior plating system has built on the growing body of biomechanical research and clinical experience. Aggressive advertising espouses the relative benefits of these individual systems.
Indications for Anterior Cervical Screw-Plate Fixation
Anteriorly directed decompressive procedures for the subaxial cervical spine can be performed without grafting material (simple diskectomy), with grafting material (fusion procedure), and with graft material augmented by screw-plate instrumentation (fusion and internal fixation). Even without the placement of grafting material (simple diskectomy), spontaneous interbody arthrodesis is frequently observed. Clinical results reported by the senior author (VKHS) attest to the efficacy of the simple diskectomy procedure in younger patients characterized preoperatively by normal cervical lordosis, stable flexion and extension plain radiographs, absence of significant axial (neck) pain, and degenerative disease limited to one or two levels.9
The rationale for performing internal fixation and fusion of the subaxial cervical spine can be distilled as follows: to restore stability to the structurally compromised spine, to maintain alignment after correction of a deformity, to prevent progression of a deformity, and to alleviate pain.10 Degenerative, neoplastic, infectious or inflammatory, traumatic, and iatrogenic (postsurgical) causes of vertebral column instability, with or without concomitant neural compression, are well-suited for treatment with rigid internal fixation from an anterior surgical approach. Anterior cervical plates function to optimize the environment for osseous union by providing immediate rigid fixation across the span of desired arthrodesis. Internal fixation with screw-plate systems is performed solely in conjunction with a grafting procedure. The proximity of this instrumentation to the fusion substrate functions to resist graft displacement or disruptive micromotion at the graft-vertebral body interface and frequently obviates the need for postoperative bracing with an external orthosis in most cases.
At our institution, absolute criteria for cervical plate instrumentation include procedures that involve any extent of formal corpectomy or patients with posttraumatic spinal instability. In the event of a particularly severe (three-column) injury,11 an isolated anterior construct might not impart sufficient stabilization. In this circumstance, the addition of a posterior fixation procedure (circumferential fusion) to reconstruct the posterior tension band or the use of a rigid external orthosis would be necessary.12–15 Anterior instrumentation and fusion procedures are now routinely performed after any number of levels of anterior cervical discectomy.16–18
Individual patient characteristics can adversely affect the anticipated success of bone healing and provide relative indications for incorporating internal fixation in the operative strategy. Malnutrition, the active use of tobacco, the presence of significant osteoporosis or other disorders that result in poor bone quality, the need for exogenous steroids, and a history of previously unsuccessful fusion efforts (at the same or different vertebral levels) are relative indications for an anterior cervical plate.19,20
Operative Technique
Preoperative Preparation and Positioning
After informed consent for the surgical procedure has been obtained, patients are brought to the operating room wearing antiembolic stockings. Intravenous and intra-arterial access are secured, and a single prophylactic dose of antibiotic is administered 30 minutes before the skin is incised. In patients with evidence of myelopathy or significant compromise of the vertebral canal, baseline evoked potentials (somatosensory and motor) are measured before the patient is intubated or positioned. Muscle relaxants are avoided during surgery to provide an immediate indication of neural irritation. Patients with posttraumatic cervical instability or preexisting myelopathy undergo fiberoptic or awake intubation with the surgeon in attendance. Patients with preexisting myelopathy may receive methylprednisolone in accordance with the NASCIS III protocol immediately before the procedure begins.21 Drug infusion is continued throughout the procedure and is discontinued after surgery when the patient’s neurological examination is stable. A urinary catheter is placed after general anesthesia is induced if the procedure is anticipated to exceed 3 hours. When patients are positioned, bony and soft tissue prominences are carefully padded to prevent pressure sores or peripheral neuropathies.
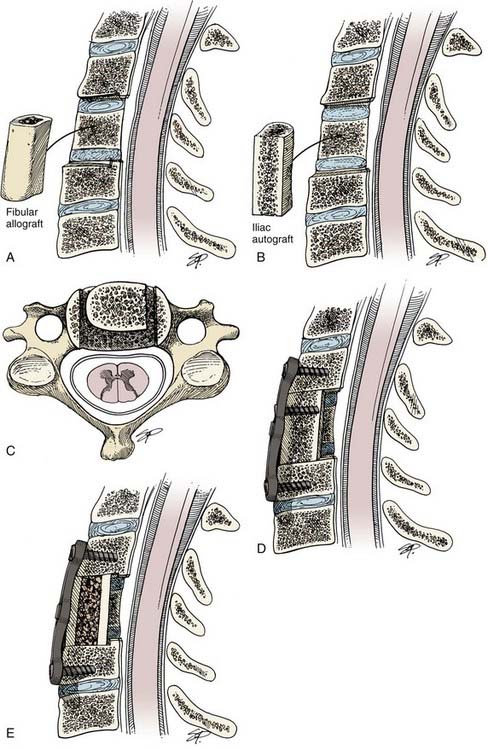
Before surgery patients are counseled regarding the choice of autograft or allograft for their fusion substrate. Given the slightly lower but comparable rate of anterior cervical fusion using fibular allograft instead of autograft (particularly for single-level procedures) and the opportunity to prevent the complications associated with harvesting a tricortical segment of autologous iliac crest, most of our patients choose an allograft fusion procedure.20,22 Among the choices for allograft sources, we prefer fibular allograft given its greater compressive strength compared with tricortical iliac crest allograft.6,20,23,24 An alternative to bone grafts is now available with the emergence of polyetheretherketone (PEEK) implants, which are associated with fusion rates similar to those of bone grafts when used in conjunction with the correct dose of recombinant human bone morphogenic protein-2 placed inside the implant.25
Reported donor site complications after autologous iliac crest harvest include acute and chronic pain, infection, arterial hemorrhage, peripheral nerve injury, pelvic instability, cosmetic deformity, hernia formation, and postoperative hematoma.26 The risk of transplanting HIV-infected bone has been estimated at less than 1 in 1 million when stringent screening criteria are used.6,24,27 If an autograft is to be harvested from the iliac crest, the appropriate hip is elevated with a towel roll. Patient preference determines the side from which the autograft is removed. An intrascapular roll, tape along the lateral aspect of the arms, and soft wrist ties that can be manipulated by the circulating nurse are helpful adjuncts that facilitate intraoperative radiographic visualization of the distal vertebral column.
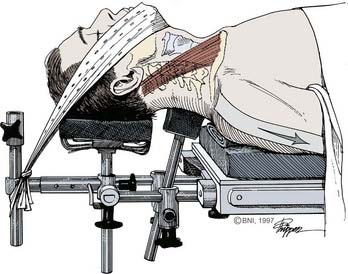
We prefer the Caspar head holder (Aesculap, Center Valley, PA) to support the patient’s head and cervical spine (Fig. 297-1). The head is maintained in a neutral position, and the neck is maintained neutrally or is extended minimally with the assistance of a chin strap. The evoked potentials should be observed carefully for any changes, and intraoperative fluoroscopy should be available to confirm the maintenance of cervical alignment (anatomic or best attainable) after positioning is completed. At our institution, the convenience and cost-effectiveness of using cross-table fluoroscopy from the beginning of the procedure are well-established compared with the relative expense and delays associated with obtaining intraoperative plain film radiographs. The importance of fluoroscopy in confirming the operative level, selecting an appropriately sized cervical plate, directing screw trajectories, assessing final screw positions, and evaluating plate alignment relative to the vertebral column cannot be overstated.
Skin Incision
The operative approach is directed from the side that is most comfortable for the surgeon and usually corresponds to the patient’s right side in a right-handed surgeon. It was thought that the recurrent laryngeal nerve is more susceptible to injury given its relatively anterolateral course outside the tracheoesophageal groove when compared with the left side.28 Consequently, some surgeons may prefer an approach directed from the patient’s left side. However, injury to the thoracic duct has been reported as a complication of approaching the caudal cervical spine from the left side.29 Studies have shown that there is no difference in the incidence of recurrent laryngeal nerve injury associated with a right- or left-sided approach.30,31 If the patient has already undergone a cervical procedure, we pursue operative access from the ipsilateral side. Although this strategy requires contending with scar tissue and altered anatomic planes, it avoids the more daunting possibility of incurring bilateral injury to vagal nerve branches, the unilateral manifestations of which may be subtle and otherwise undetected unless specifically evaluated for after the previous procedure. If a contralateral approach to a previous scar is pursued, we recommend that the patient undergo preoperative examination of the vocal cords by an otolaryngologist to avoid the possibility of bilateral injury to vagal nerve branches.
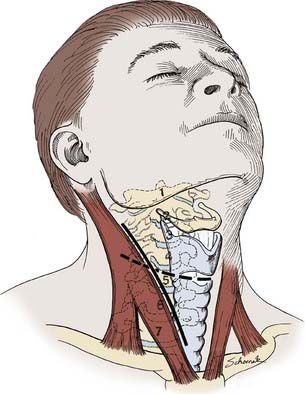
A general orientation along the cervical spine can be estimated by external anatomic landmarks (Fig. 297-2), but intraoperative fluoroscopy ensures a more precise placement of the skin incision and limits the amount of soft tissue dissection necessary to obtain adequate visualization of the targeted segment of the vertebral column. Preoperative use of the fluoroscope to define the most rostral and caudal levels of exposure necessary for decompression and stabilization also assists in selecting the optimal orientation for the incision. We have found that a transverse incision located within a skin crease is cosmetically superior to a longitudinal incision that follows the medial border of the sternocleidomastoid muscle. When extended adequately (beyond the midline and laterally across the sternocleidomastoid muscle) and accompanied by generous undermining of the platysma muscle, a transverse incision rarely fails to provide sufficient access and visualization to enable multiple corpectomies to be performed with an accompanying fusion and plating procedure. However, the longitudinal incision may be more functional in patients with difficult anatomy or in whom a particularly long fusion construct is required.
Soft Tissue Dissection and Exposure of the Vertebral Column
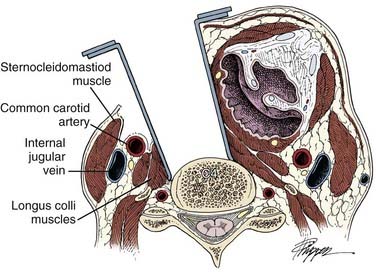
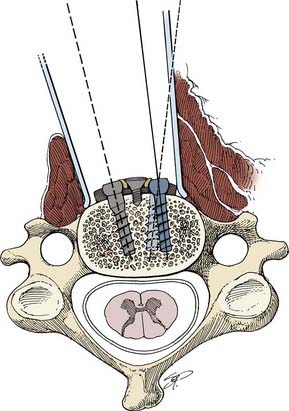
After the patient has been prepared and draped, the skin is sharply incised to the level of the platysma muscle. Hemostasis is obtained with electrocauterization, and the platysma layer is traversed or split longitudinally. Early attention to broad undermining of this subcutaneous muscle is greatly rewarded by the rostral and caudal extents of surgical exposure that can be attained. The underlying sternocleidomastoid muscle and tracheoesophageal bundle are identified, and the avascular plane between these structures is developed with careful, blunt dissection. A trajectory medial to the carotid sheath is followed, and the underlying vertebral column is palpated (Fig. 297-3). Comparing the osteophytic topography to preoperative or intraoperative radiographs can often help orient the surgeon along the cervical column, but fluoroscopy is used for definitive localization along the cervical spine. The prevertebral fascia is opened, and the ventral aspect of the anterior longitudinal ligament is cleaned of overlying soft tissue. The medial insertions of the longus colli muscles are elevated bilaterally from the vertebral column.
Several self-retaining retractor systems are available for enhancing exposure of the anterior vertebral column. Fundamental to all of these retractors is the requirement to seat their laterally directed blades deep to the longus colli musculature to prevent injury to the adjacent tracheoesophageal bundle or carotid artery. Injury to the vagal innervation of the larynx can result in silent aspiration (superior laryngeal branch) or hoarseness (recurrent laryngeal nerve). Apfelbaum and Kriskovich8 have reported that injury to the recurrent laryngeal nerve during anterior cervical surgery is most likely because of compression of the endolaryngeal segment of this nerve against the shaft of the endotracheal tube after the retractor is placed rather than direct injury from dissection. To protect against this neuropraxia, they describe transiently deflating the cuff of the endotracheal tube after placing the self-retaining retractors and then reinflating the cuff to “just seal” pressure. This allows the endotracheal tube to recenter within the larynx and remove pressure from the laryngeal wall. This technique improved the incidence of injury to the recurrent laryngeal nerve, which decreased from 6.4% in 250 patients undergoing anterior cervical plating without this maneuver to 1.7% of the next 650 consecutive patients in whom it was used.
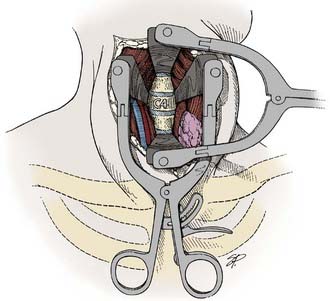
Rostral-caudal exposure can be improved by placing a second retractor perpendicular to the first (Fig. 297-4). Use of the high-speed drill to remove obstructing osteophytes, in conjunction with the superior illumination and magnification offered by the surgical microscope, has significantly diminished the amount of active cervical distraction necessary to confirm adequate neural decompression during a diskectomy procedure. Distraction posts are usually inserted in the vertebrae to improve exposure of the disk space during decompression of the spinal cord and neural foramina. Alternatively, some surgeons maintain vertebral distraction by placing patients in axial traction using Gardner-Wells tongs at the start of the procedure32 or through gentle, even traction applied by the anesthesiologist during graft impaction. If the patient is maintained in tongs during the procedure, it is crucial to remember to release this distraction after the grafting material has been inserted and before the fixation hardware is placed.
Discectomy With or Without Corpectomy
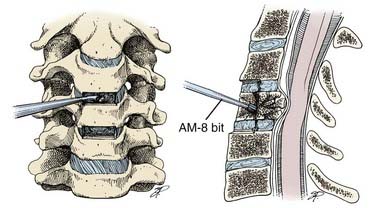
Once orientation at the level of pathology has been confirmed, annulotomies are performed and superficial diskectomies are initiated with straight and angle curets (Fig. 297-5A). If an interval corpectomy is necessary, a bone rongeur can be used to resect the anterior half of the vertebral body and the Midas Rex drill (Medtronic, Memphis, TN.) used to complete the deeper aspect of bone removal (Fig. 297-5B). If placement of an allograft strut (fibular) is planned, autologous bone from the vertebrectomy site is saved for packing the hollow center of the allograft shaft. The operative microscope is routinely used to assist with the removal of deeper bone and soft tissues to facilitate safe exposure of the dura. The epidural space is inspected, and posteriorly based osteophytes are removed from the vertebral bodies and foramen to ensure adequate decompression of the spinal cord and nerve roots. Where possible, generous diskectomies are substituted for a corpectomy if adequate neural decompression can be achieved through wide and deep undercutting of the offending posterior vertebral body surfaces. The benefits of avoiding a complete corpectomy include preserving additional sites for screw fixation along the plate and circumventing the higher risk of nonunion or hardware failure that accompanies fusion constructs involving multiple corpectomy segments.33,34 This latter point is particularly relevant for patients who require multilevel decompressions.
When completed, the typical lateral extent of tissue removed for diskectomies or corpectomies spans up to 18 to 20 mm. Reliable identification of the vertebral midline is crucial to ensure adequate decompression of neural tissue and to prevent vascular complications related to injury of the vertebral artery.35–37 Frequently, severe degenerative disease, traumatic disruption, or scarring from previous surgical procedures result in the loss of the otherwise apparent anatomic midline. Typically, however, several anatomic cues remain and can be used to provide orientation to the midline for both decompressive maneuvers and plate positioning (Table 297-1). Marking the midline of the vertebral bodies with monopolar cauterization before the longus colli muscles are elevated can also provide helpful reference as the procedure progresses. It is also worthwhile to confirm with the anesthesiologist that the patient’s head has not deviated from the midline position established at the beginning of the case.
TABLE 297-1 Anatomic Cues Available for Maintaining Midline Orientation
| Location of longus colli muscles |
| Location of uncovertebral joints |
| Curvature of vertebral body (lateral margin/waist) |
| Location of epidural veins and fat |
| Curvature of dural tube |
| Visualization of nerve roots |
| Palpation of pedicles |
| Location of sternomanubrial notch (angle of Louis) |
| Use of anteroposterior fluoroscopy (pedicle/spinous process location) |
From Baskin JJ, Vishteh AG, Dickman CA, et al. Techniques of anterior cervical plating. Oper Tech Neurosurg. 1998;1:90-102.
Bone Grafting and Plate Fixation
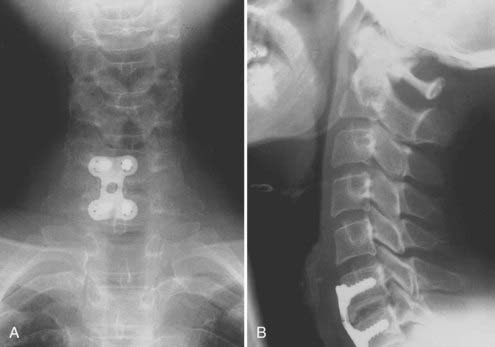
Screw-plate application provides immediate rigid fixation of the cervical spine and functions analogously to an internal halo brace. By ideally imparting some combination of load bearing to the vertebral column and load-sharing properties through the graft site, plating systems protect the neural elements from trauma while facilitating the development of a fusion response, respectively. Bone and instrumentation deform and reform as stress is applied.38 Over time, even the most rigid constructs permit some segmental motion across the site of fixation. In the absence of an osseous union, repetitive loading will fatigue an implant to the point of failure through loosening or breakage. Consequently, perhaps the most fundamental principle related to performing rigid internal fixation is that the presence of instrumentation does not substitute for a carefully conceived and meticulously prepared fusion site.39,40 In the absence of an associated arthrodesis, hardware failure is a time-dependent certainty (Fig. 297-6).
We typically use the Robinson-Smith technique for interbody fusion after a cervical diskectomy.41 Techniques to optimize the chances for successful arthrodesis (Table 297-2) at the operative site can be subdivided into those that (1) enhance the natural capacity for bone healing to occur, (2) minimize the extent of iatrogenically induced impediments to bone graft incorporation, and (3) maximize the biomechanical advantage of the hardware construct.
TABLE 297-2 Techniques to Optimize Fusion-Hardware Construct
| MANEUVER | BENEFIT |
|---|---|
| Insert graft under compression. | Improves graft incorporation |
| Maximize surface of implant-bone interface. | Improves graft incorporation |
| Remove soft tissue from fusion interface. | Avoids fibrous healing |
| Maintain integrity of cortical end plate. | Prevents telescoping of graft |
| Irrigate while drilling. | Prevents thermal injury with impaired bone healing/resorption |
| Avoid contouring plate. | Prevents fatiguing of implant |
| Avoid overtightening screws. | Prevents stripping screw hole and diminishing bone purchase |
| Insert angulated screws. | Improves pull-out strength |
| Use longest screws possible. | Improves pull-out strength |
From Baskin JJ, Vishteh AG, Dickman CA, et al. Techniques of anterior cervical plating. Oper Tech Neurosurg. 1998;1:90-102.
Enhancing the Natural Capacity for Bone Healing
Bone grafts are incorporated with the greatest success when the fusion construct is maintained under a compressive load (Wolff’s law).42 Consequently, the vertical dimension of the graft material being used is typically sized a few millimeters longer than the measured diskectomy or corpectomy defect to ensure mechanical compression of the graft within the recipient bed. At the time the graft is placed, the adjacent vertebral bodies can be distracted mildly through several techniques (disk space spreader, vertebral body distraction posts, axial traction, or gentle vertical distraction by the anesthesiologist) to ensure that the graft ultimately experiences a compressive load. After the posterior half of the graft has been tamped into place, the vertebral body distraction is released and the remainder of the graft advanced. These maneuvers promote seating and prevent excessive impaction of the graft. When relying on axial traction applied with cranial tongs to achieve vertebral distraction during the decompressive portion of the procedure, it is important not to overlook requesting its release before proceeding to internal fixation.
Iatrogenic Impediments to Fusion Biology
High-speed drills are convenient for denuding articular surfaces within the fusion bed and for shaping the fusion surfaces of the vertebral bodies and graft. During all drilling, consistent irrigation is needed to prevent thermal injury that can incite subsequent bone resorption and interfere with the fusion response. Similarly, the excessive use of monopolar cauterization to expose the vertebral column can impede healing as a result of direct thermal injury and bone devascularization. The recipient bed (vertebral surfaces) is the source of almost all of the osteogenic components critical to the fusion response. Even when using an autologous bone graft, few of the transplanted osteoblasts and osteocytes actually survive to contribute to healing.20 As such, the surface area of healthy vascularized bone in the fusion bed should be maximized. Using monopolar cauterization for deep tissue dissection also places adjacent soft tissues (e.g., esophagus, recurrent laryngeal nerve) at greater risk. Bone bleeding within the recipient site can be controlled with thrombin-soaked Gelfoam sponge (Upjohn, Kalamazoo, MI.), Avitene powder (MecChem, Woburn, MA.), Floseal (Baxter, Deerfield, IL.) or, if particularly intractable, bone wax. These substances hinder the fusion response and should be used sparingly at the graft-vertebral body interface.
Optimizing the Fusion and Hardware Construct
In contrast to cervical fusion procedures that do not include instrumentation, the graft material is not countersunk away from the ventral margin of the disk space. Instead, the anterior border of the bone plug or strut is left in line with the anterior margin of the adjacent vertebral bodies to maximize the contact surface between the plate and the entire fusion construct. A trough along the posterior aspect of one of the vertebral bodies protects against graft retropulsion and epidural compression. Autograft struts that span more than a one-level corpectomy are secured to the plate with a bicortically anchored screw to prevent graft retropulsion. Typically, fibular allograft is too brittle to accept a bone screw, and posterior troughs are created at the upper and lower vertebral levels to protect against its displacement (Fig. 297-7).
When the recipient site is prepared for graft placement, the cortical end plates are thinned sufficiently to expose bleeding bone but mostly left intact to minimize telescoping of the graft material through the adjacent vertebral bodies. This step is particularly important when allograft material is implanted because its rigidity makes this complication more likely than when autograft is used, especially in patients with osteopenic or otherwise soft bone. Loss of graft height, either because of settling or resorption, adds further mechanical stress to the screw-plate construct and increases the risk for implant failure and pseudarthrosis. Proper attention to graft harvesting (autograft) or preparation (allograft) optimizes the load-bearing capabilities of these materials. We prefer to harvest autologous iliac crest bone using an oscillating saw to prevent osteotome-related microfractures, which can reduce the compressive strength of the graft.43 Failure to reconstitute the freeze-dried allograft appropriately in saline (minimum of 30 minutes) before it is shaped or implanted compromises its structural integrity.20
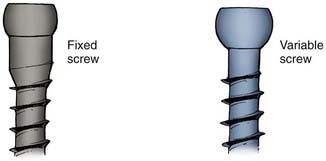
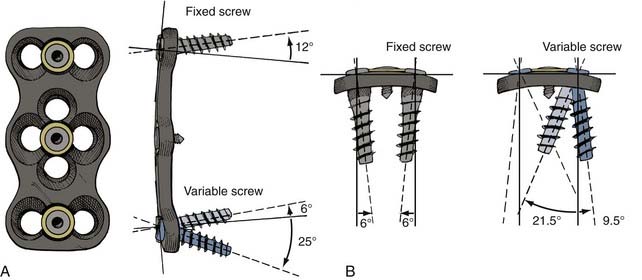
Selection of screw type and screw length depends on the pathology being addressed. The interaction of variable angle or fixed angle screws with the plate determines whether a plate acts as a constrained system or semiconstrained system or hybrid system. Use of variable angle screws allows some movement at the screw-plate interface and thus allows settling of the vertebral body end plate on the interbody graft. Such constructs are considered load-sharing or dynamic fixation. Fixed angle screws do not allow movement at the screw-plate interface and act against settling of the vertebral body end plate on the graft. These constructs are considered load-bearing or constrained or static fixation. Using a combination of fixed and variable angle screws is considered semiconstrained or a hybrid construct. Biomechanical studies on cadaveric specimen have shown that variable angle screws provides better load-sharing properties than fixed angle screws when graft subsidence considered.44 For degenerative pathology, we prefer a hybrid construct using fixed angle screws at the most caudal vertebral level and variable angle screws at the remaining levels. For traumatic pathology, we prefer a constrained system and thus use fixed angle screws at all levels and aim for bicortical purchase.
If possible, the screw trajectory should capture the denser bone tissue in the subchondral region of the vertebral body while respecting the end plate of the vertebral body. Crossing the distal vertebral end plate results in a suboptimal screw purchase that can further loosen over time because of motion across the violated disk space. Alternatively, this misplacement risks incorporating a normal motion segment within the fusion construct. If unicortical screw placement is pursued, the longest screws that can be accepted by an individual patient’s anatomy are used for plate fixation because they resist pulling out better than their shorter counterparts. When fixation involves multiple segments, the plate should be secured at as many points as possible. This step is particularly important at the caudal aspect of the plate given the greater failure stresses transmitted to that location.33,34 Because additional sites for fixation are preserved, partial corpectomies or generous diskectomies are desirable substitutes for a completed corpectomy. Obviously, minimizing bone removal presupposes satisfying the goal of adequate neural decompression. Midsagittal application of the plate fosters optimal load sharing among the fixation points and is facilitated by fluoroscopic guidance, as noted below.
Closure
Final inspection of the operative site includes assessing the alignment of the vertebral column after fixation, the position of the graft with respect to the epidural space, and the length of the plate and position of the screws with respect to the rostral and caudal disk spaces. Midline location and vertical orientation of the plate can be assessed fluoroscopically by observing the parallel overlap of plate holes and screw trajectories on true lateral cross-table views. An anteroposterior view can be obtained as the fluoroscope is removed from the operative field. Location of the plate midway between the vertebral pedicles and in line with the superimposed spinous processes confirms placement in the vertebral midline. The asymmetrical application of a plate most often is a consequence of the caudal aspect of the plate being shifted toward the side of surgical approach (see Fig. 297-6A).
Orthoses and Postoperative Follow-Up
The nature of the patient’s preoperative pathology, the extent of their underlying mechanical instability, and the length of their fusion construct dictate the type of postoperative cervical orthosis prescribed. In patients who have a three-column traumatic disruption of their spinal column or who suffer from an underlying metabolic impediment to healing (i.e., rheumatoid arthritis), a halo brace, or a posterior fusion should be considered for additional postoperative stabilization. Multilevel plate constructs are more prone to failure than their shorter counterparts.33,34 A patient whose procedure involves three or more corpectomies should be managed in a halo brace or augmented with a posterior fusion.33 When screw purchase is good in patients undergoing a single-level, two-level, or three-level fusion and plating procedure for spondylotic disease, they can likely be maintained without a collar after surgery.
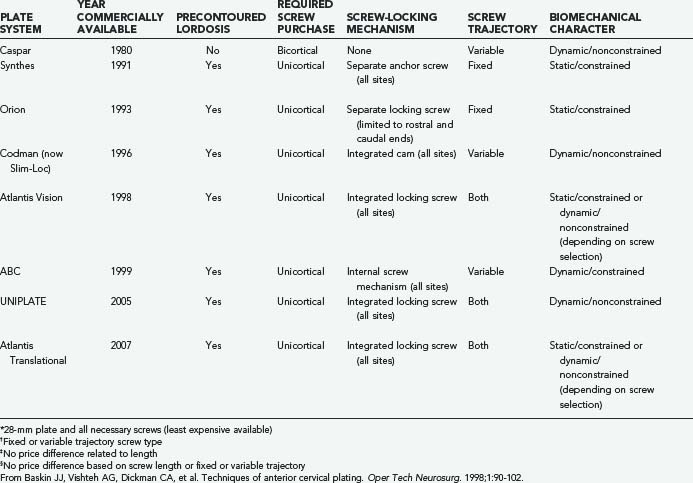
The Evolution of Screw-Plate Systems
The first reported use of screw-plate fixation in the anterior cervical spine occurred in 1964 and is attributed to Bohler and Gaudernak.45 They relied on the available hardware of the time, which was intended for long bone (extremity) fixation. In 1982, Caspar described a novel technique and instrumentation system (retractors, distractors, and screw-plates) that popularized the practice of anterior cervical plate application.46 From this beginning, several anterior cervical screw-plate systems have emerged. Some of the more frequently used systems are listed in Table 297-3. Each system has its own advocates and detractors, and the relative merits of one product compared with another largely remain subject to an individual surgeon’s preference rather than to an objectively demonstrated superiority of one system over another. Our institutional experience with anterior cervical plates has been derived from the use of different systems (Caspar, Aesculap; Synthes, Synthes Spine, Paoli, PA.; Orion, Medtronic Sofamor Danek, Memphis, TN.; Codman, Codman & Shurtleff Raynham, MA.; and Atlantis and Venture, Medtronic Sofamor Danek) whose specifications are detailed below. In addition, the ABC system (Aesculap), UNIPLATE system (DePuy Spine, Raynham, MA.), and Atlantis Translational System (Medtronic Sofamor Danek) are included in this comparison as new plates, although we have little clinical experience with them.
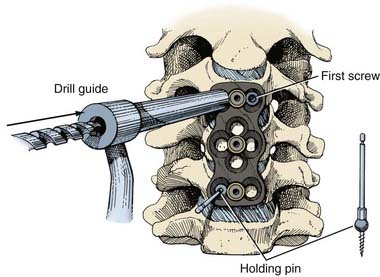
Most systems now offer an expanded selection of screw lengths and the option of standard or self-tapping screws. However, there is often a substantial disparity in cost between the standard screws and their self-tapping counterparts and between screw lengths considered to be “regular” or “expanded” (Table 297-3). A common inclusion within most of the recent generations of systems is a temporary “holding pin” that stabilizes the plate during screw-hole drilling and screw placement. These pins prove to be very useful during multilevel plate fixation and are placed either through designated holes along the plate midline or within one of the plate’s screw holes.
Some Individual Plating Systems
Caspar System
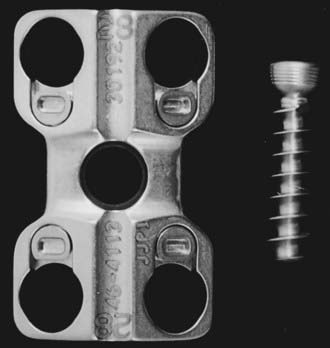
Introduced commercially in 1982, the Caspar osteosynthetic plate requires bicortical screw purchase (Fig. 297-8). The screw trajectory is variable, and no locking mechanism secures the screw head to the plate (nonconstrained/dynamic system). The requirement for bicortical screw purchase makes this the most technically challenging system to use because the depth of posterior cortical penetration must be determined precisely to avoid compromising the epidural space. The plates are machined without contour in the sagittal plane but can be curved as desired. The slotted configuration allows screws to be positioned and redirected as necessary. The recommended screw trajectory is directed 15 degrees medially and parallel to the adjacent vertebral end plate. The appropriate plate length should measure 2 mm from the rostral and caudal end plates of the rostral and caudal vertebral bodies, respectively, that are incorporated into the fusion construct.34,47 The posterior longitudinal ligament sufficiently shields the dura as long as the blunt-tipped bicortically placed screw does not extend further than the width of one screw thread beyond the posterior cortex.
Although bicortical screw placement poses a greater potential risk for dural violation and spinal cord injury than a unicortically positioned screw, the Caspar system has been in clinical use longer than any of the available screw-plate systems. It remains popular with a very low reported rate of complication.47 The newer generation Caspar titanium plate has been modified to include midline holes for holding pin placement and is marked to orient surgeons to its rostral and caudal ends. It is the least expensive of the available screw-plate systems (Table 297-3).
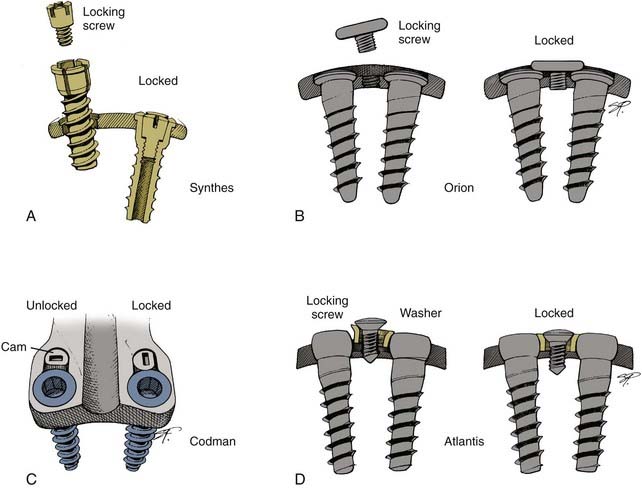
Synthes
Introduced in 1986, the Synthes unicortical system (Cervical Spine Locking Plate) employs fixation screws that accommodate a separate internal 1.8-mm expansion locking screw (Fig. 297-9). This combination rigidly secures the screw head to the plate (constrained/static system). The rostral and caudal fixation screws are directed in a fixed, medially convergent trajectory that increases the resistance to pulling out. The upper screws are angled 12 degrees cephalad to approximate the cervical lordosis, and the lower screws are directed perpendicular to the plate in the sagittal plane.24,48 Initially available only in a 4.0-mm diameter, 14-mm length, the fixation screws are now produced in 12-, 14-, and 16-mm lengths in both standard and self-tapping varieties. The working screw diameter for the set is 4.0 mm, and a 4.35-mm rescue screw is available in standard and self-tapping forms. As is the case with all of the plating systems, self-tapping screws are significantly more expensive than the standard variety (see Table 297-3).
Orion
This contoured system uses a fixed trajectory screw (constrained/static system) that is medially convergent (6 degrees) with 15 degrees of angulation at the rostral and caudal ends (divergent) (Fig. 297-10). As with the Synthes system, further plate bending alters the cephalad and caudal angulations of screw placement. In contrast to every other locking plate system, the Orion plate accommodates locking screws (separate components) only at its rostral and caudal ends. The head of each locking screw overlaps the tops of the paired 4.0-mm diameter fixation screws at the respective ends of the plate. Additional anchoring screws can be placed through a variable interval slot (4.35-mm diameter screws recommended) that is present within the longer plates. Screws in this location, however, cannot be secured to the plate with a locking screw and preferably are placed with a bicortical purchase. A 4.5-mm rescue screw is available within this system. The 4.0-, 4.35-, and 4.5-mm screws are currently produced only in a self-tapping form.
Insertion of the locking screw requires an orientation that is truly perpendicular to the plate surface. Failure to achieve this angle, which may be particularly difficult in the vicinity of the mandible or clavicle, can prevent successful placement of the locking screw. A self-limiting torque mechanism causes the driver for the locking screw to twist free from the screw head when it is secured appropriately. Plate sizing must allow for the fixed screw angulation of 15 degrees. Because of the vertical angle of the screws, the plate length should span just beyond the margins of the graft site to ensure that the screws do not violate the adjacent end plates.49
Slim-Lock Cervical Plate
The slimlock cerrical platie (DePuy Spine) is a contoured titanium plate (Fig. 297-11) that offers variable trajectories for screw insertion and has no specific rostral or caudal end. A locking cam mechanism integrated into the plate resists screw back out and allows unicortical screw fixation. However, the screw head is not rigidly fixed within its plate hole and can change its angulation relative to the plate (nonconstrained). This dynamic aspect of the system allows some load sharing and affords the system some tolerance for delayed vertebral settling that might occur because of graft resorption or telescoping.
The more commonly used 12- and 15-mm drill bits, taps, and screws are color-coded (blue and gold, respectively) to simplify use of the system. However, a wide range of screw lengths is available and can be inserted using the available variable depth drill guide and taps. All screws in this system are 4.5 mm in diameter, the size typically reserved for rescue screws in other systems. The recommended screw placement is 10 degrees medially and parallel to the orientation of the adjacent disk space in the sagittal plane. The recommended plate length is from the rostral subchondral region of the most rostral vertebral body to the caudal subchondral region of the most caudal vertebral body included in the fusion construct.50
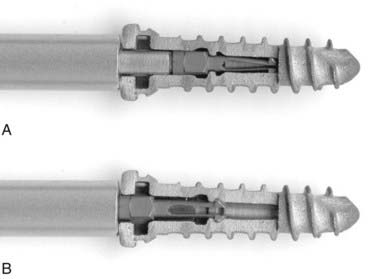
Atlantis Vision System
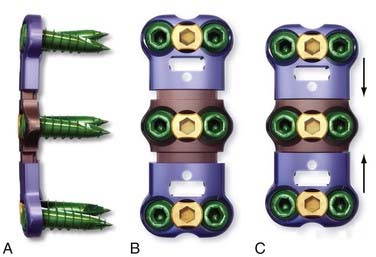
With the Atlantis Vision System, fixed or variable screw trajectories are available for any plate level or screw site (Figs. 297-12 and 297-13). The system includes specific drill guides that either lock in a fixed position in the plate screw hole (12 degrees divergent in sagittal plane, 6 degrees medially convergent) or allow variable angulation through an arc of approximately 31 degrees relative to the axis of the screw hole (Fig. 297-14). The diameter of the holding pin available for hands-off stabilization of the plate during drilling is small enough that an anchoring screw can ultimately be passed along its track (Fig. 297-15). The option of fixed or variable screw trajectories within any one plate-hole site enables the production of constrained, nonconstrained, or hybrid biomechanical constructs based on the underlying pathology of the vertebral column (Fig. 297-16).
The locking mechanism of the Atlantis plate consists of a locking screw and washer, which compress and cover the fixation screw heads in pairs (Fig. 297-17). Similar to the Codman system, extremes in screw angulation can result in an incomplete interface between the anchor screw and locking mechanism. At the time of screw insertion, it is important to make certain that the locking washer remains above the level of the fixation screw head. Due to its mobility while in an unlocked position, the locking washer can be caught under the head of the anchor screw as the latter is advanced into the vertebral body. The anchor screw would then be prevented from fully seating within its plate hole, and locking the pair of anchor screws to the plate would be precluded. The Atlantis plate is manufactured with all of the locking screws in the open, elevated position. Before the wound is closed, all locking screws should be recessed to minimize the profile of the fixation construct.
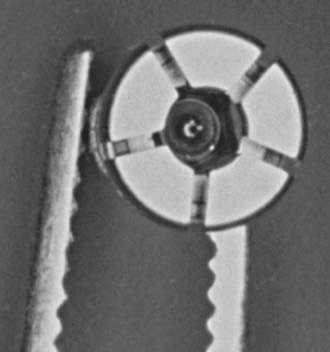
ABC System
Released for use in 1999, this system consists of precontoured, slotted, trapezoidal plates and a variable trajectory screw (Fig. 297-18). The screw head consists of five compressible petals that snap into the plate slot and prevent the screw from backing out (Fig. 297-19). The screws also have a self-contained locking mechanism: An internal pin, engaged by a locking tool, can be pulled up into the screw head and functions to block the petals in their respective positions and to secure the screw head rigidly to the plate (Fig. 297-20). Although the angle between the screw head and plate is fixed (constrained), the screws can migrate vertically within their slots. This capacity to maintain axial loading despite graft subsidence permits load sharing by minimizing the presence of stress shielding and promotes fusion.51
Atlantis Translational System
An example of translational plates is the new Atlantis Translational system, which became available in 2007. The plate features fixed and variable angle screws allowing constrained, nonconstrained, or hybrid biomechanical constructs. It also features an integrated locking mechanism (Fig. 297-21). The intention of this new plate is to maintain constant graft compression throughout the range of motion of the cervical spine by allowing unidirectional translation up to 2 mm per level in 1-mm increments. Unlike bidirectional translational plates that allow graft unloading during extension, unidirectional translational plates maintain constant graft loading even during extension. In addition, this plate allows in situ compression of the plate to maintain active compression of the interbody graft. This feature could be particularly helpful for the treatment of traumatic distraction injuries. After the graft is placed, the plate is locked in place with fixed angle screws. The plate can be compressed up to 2 mm per level using a plate compressor that fits in the locking mechanism (Fig. 297-22).
UNIPLATE System
The UNIPLATE system has been available since 2005. Compared with all the systems discussed previously, it features one column of screws instead of two columns with one screw hole per vertebral body level. It is available with two or three screw holes and thus can be applied after a one- or two-level anterior cervical discectomy and fusion (Fig. 297-23). Similar to the Slim-Lock plate, the UNIPLATE features a cam locking mechanism to lock the screw. There is a paucity of biomechanical data on the efficacy of the UNIPLATE design in stabilizing the cervical spine. As a result, the UNIPLATE can be regarded as an effective graft-holding device to prevent complications from interbody kick-out after an anterior cervical discectomy and fusion.
Complications
The risks related to screw-plate stabilization of the cervical spine include all risks intrinsic to a routine anterior cervical discectomy and fusion procedure52,53: injuries to vertebral and carotid arteries, injury to branches of the vagus nerve (recurrent or superior laryngeal nerves), dysphagia, radicular or myelopathic injury, cerebrospinal fluid leakage, infection, graft migration, postoperative hematoma, stroke and, if autologous graft is used, donor site morbidity. The development of pseudarthrosis (fibrous union) and instrumentation failure are intimately related. The primary occurrence of either can result directly in the other and necessitate revision of the entire fusion and fixation construct. Alternatively, successful arthrodesis can develop in the presence of failed instrumentation,54,55 thus illustrating the race between bony healing and implant fatigue. In this circumstance, the need to remove the hardware is not absolute and would have to be considered in the context of patients’ symptoms (if any) and their risk for tracheoesophageal or neurovascular injury.
Conclusion
A socioeconomic argument for using screw-plate systems after anterior cervical discectomy and fusion is that patients who receive these implants may require briefer hospitalizations, may have less or no need for an external cervical orthosis, and may return to work earlier than those who undergo cervical fusion procedures without plating. The cost of plates and screws varies greatly among systems. Individual hospital contracts with manufacturers can dramatically influence the cost of using one instrumentation construct compared with another. The figures listed in Table 297-3 reflect the manufacturers’ catalogue citations for 2008. Additional surgeons’ fees for performing internal fixation, the extra operating time needed, the expense and radiation exposure associated with the fluoroscopy necessary to perform this procedure safely, and postoperative radiography are other variables that should be considered when calculating the cost-to-benefit ratio of screw-plate insertion.
Aebi M, Zuber K, Marchesi D. Treatment of cervical spine injuries with anterior plating. Indications, techniques, and results. Spine. 1991;16:S38-S45.
Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate: a prospective comparative analysis. J Neurosurg. 1996;85:206-210.
Brodke DS, Klimo PJr, Bachus KN, et al. Anterior cervical fixation: analysis of load-sharing and stability with use of static and dynamic plates. J Bone Joint Surg Am. 2006;88:1566-1573.
Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989;25:491-502.
Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine. 1983;8:817-831.
Flynn TB. Neurological complications of anterior cervical interbody fusion. Spine. 1982;7:536-539.
Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: a meta-analysis of fusion rates. J Neurosurg Spine. 2007;6:298-303.
Hadley MN, Sonntag VKH. Cervical disc herniations. The anterior approach to symptomatic interspace pathology. Neurosurg Clin N Am. 1993;4:45-52.
Harkey HL. Bicortical anterior cervical plate fixation. Tech Neurosurg. 1995;1:108-116.
Kaufman HH, Jones E. The principles of bony spinal fusion. Neurosurgery. 1989;24:264-270.
Kilburg C, Sullivan HG, Mathiason MA. Effect of approach side during anterior cervical discectomy and fusion on the incidence of recurrent laryngeal nerve injury. J Neurosurg Spine. 2006;4:273-277.
Kurz LT, Garfin SR, Booth REJr. Harvesting autogenous iliac bone grafts. A review of complications and techniques. Spine. 1989;14:1324-1331.
Pait TG, Killefer JA, Arnautovic KI. Surgical anatomy of the anterior cervical spine: the disc space, vertebral artery, and associated bony structures. Neurosurgery. 1996;39:769-776.
Papadopoulos EC, Huang RC, Girardi FP, et al. Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine. 2006;31:897-902.
Paramore CG, Dickman CA, Sonntag VKH. Radiographic and clinical follow-up review of Caspar plates in 49 patients. J Neurosurg. 1996;84:957-961.
Tumialan LM, Pan J, Rodts GE, et al. The safety and efficacy of anterior cervical discectomy and fusion with polyetheretherketone spacer and recombinant human bone morphogenetic protein-2: a review of 200 patients. J Neurosurg Spine. 2008;8:529-535.
Wang JC, McDonough PW, Kanim LE, et al. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine. 2001;26:643-646.
White AA, Panjabi MM. Biomechanical considerations in the surgical management of the spine. In: White AA, Panjabi MM, editors. Clinical Biomechanics of the Spine. Philadelphia: Lippincott-Raven; 1990:511-634.
Wolff J, Maquet P, Furlong R. The Law of Bone Remodeling. Berlin: Springer-Verlag; 1986.
Xu R, Ebraheim NA. Essential bony anatomy of the cervical spine relative to instrumentation. Neurosurg Q. 1998;8:172-179.
1 Fraser JF, Hartl R. Anterior approaches to fusion of the cervical spine: a meta-analysis of fusion rates. J Neurosurg Spine. 2007;6:298-303.
2 Caspar W. Anterior stabilization with the trapezial osteosynthetic plate technique in cervical spine injuries. In: Kehr P, Weidner A, editors. Cervical Spine I. New York: Springer-Verlag; 1987:198-204.
3 Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery. 1989;25:491-502.
4 Suh PB, Kostuik JP, Esses SI. Anterior cervical plate fixation with the titanium hollow screw plate system. A preliminary report. Spine. 1990;15:1079-1081.
5 Tippets RH, Apfelbaum RI. Anterior cervical fusion with the Caspar instrumentation system. Neurosurgery. 1988;22:1008-1013.
6 Shapiro S. Banked fibula and the locking anterior cervical plate in anterior cervical fusions following cervical discectomy. J Neurosurg. 1996;84:161-165.
7 Aebi M, Zuber K, Marchesi D. Treatment of cervical spine injuries with anterior plating. Indications, techniques, and results. Spine. 1991;16:S38-S45.
8 Apfelbaum RI, Kriskovich MD. On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. spine. 2000.
9 Hadley MN, Sonntag VKH. Cervical disc herniations. The anterior approach to symptomatic interspace pathology. Neurosurg Clin N Am. 1993;4:45-52.
10 White AA, Panjabi MM. Biomechanical considerations in the surgical management of the spine. In: White AA, Panjabi MM, editors. Clinical Biomechanics of the Spine. Philadelphia: Lippincott-Raven; 1990:511-634.
11 Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine. 1983;8:817-831.
12 McAfee PC, Bohlman HH. One-stage anterior cervical decompression and posterior stabilization with circumferential arthrodesis. A study of twenty-four patients who had a traumatic or a neoplastic lesion. J Bone Joint Surg Am. 1989;71:78-88.
13 McNamara MJ, Devito DP, Spengler DM. Circumferential fusion for the management of acute cervical spine trauma. J Spinal Disord. 1991;4:467-471.
14 Stauffer ES, Kelly EG. Fracture-dislocations of the cervical spine. Instability and recurrent deformity following treatment by anterior interbody fusion. J Bone Joint Surg Am. 1977;59:45-48.
15 Van Peteghem PK, Schweigel JF. The fractured cervical spine rendered unstable by anterior cervical fusion. J Trauma. 1979;19:110-114.
16 Sonntag VKH. Point of view. Spine. 1997;22:2625.
17 Papadopoulos EC, Huang RC, Girardi FP, et al. Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine. 2006;31:897-902.
18 Wang JC, McDonough PW, Kanim LE, et al. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine. 2001;26:643-646.
19 Bishop RC, Moore KA, Hadley MN. Anterior cervical interbody fusion using autogeneic and allogeneic bone graft substrate: a prospective comparative analysis. J Neurosurg. 1996;85:206-210.
20 Dickman CA, Maric Z. The biology of bone healing and techniques of spinal fusion. BNI Q. 1994;10:2-12.
21 Bracken MB, Shepard MJ, Holford TR, et al. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury. Results of the third national acute spinal cord injury randomized controlled trial. JAMA. 1997;277:1597-1604.
22 Vishteh AG, Harrington T, Theodore N, et al. Cervical spine fusion: allograft versus autograft. Telluride, CO: Rocky Mountain Neurosurgical Society; 1996.
23 Sachs B, Brennan W. Comparison of freeze-dried allograft versus autograft in anterior cervical spine fusions. 20th Annual Meeting of Cervical Spine Research Society; Palm Desert, CA, December 3-5; 1992. 140-142 (abstract)
24 Shapiro S. Banked fibula, the locking anterior cervical plate, and allogeneic bone matrix in anterior cervical fusions following cervical discectomy. In: Rengachary SS, Wilkins RH, editors. Neurosurgical Operative Atlas. Park Ridge, IL: American Association of Neurological Surgeons; 1996:233-239.
25 Tumialan LM, Pan J, Rodts GE, et al. The safety and efficacy of anterior cervical discectomy and fusion with polyetheretherketone spacer and recombinant human bone morphogenetic protein-2: a review of 200 patients. J Neurosurg Spine. 2008;8:529-535.
26 Kurz LT, Garfin SR, Booth REJr. Harvesting autogenous iliac bone grafts. A review of complications and techniques. Spine. 1989;14:1324-1331.
27 Buck BE, Malinin TI, Brown MD. Bone transplantation and human immunodeficiency virus. An estimate of risk of acquired immunodeficiency syndrome (AIDS). Clin Orthop. 1989;240:129-136.
28 Ebraheim NA, Lu J, Skie M, et al. Vulnerability of the recurrent laryngeal nerve in the anterior approach to the lower cervical spine. Spine. 1997;22:2664-2667.
29 Hart AK, Greinwald JHJr, Shaffrey CI, et al. Thoracic duct injury during anterior cervical discectomy: a rare complication. Case report. J Neurosurg. 1998;88:151-154.
30 Kilburg C, Sullivan HG, Mathiason MA. Effect of approach side during anterior cervical discectomy and fusion on the incidence of recurrent laryngeal nerve injury. J Neurosurg Spine. 2006;4:273-277.
31 Beutler WJ, Sweeney CA, Connolly PJ. Recurrent laryngeal nerve injury with anterior cervical spine surgery risk with laterality of surgical approach. Spine. 2001;26:1337-1342.
32 McAllister P, Pait TG. Unicortical anterior cervical plate fixation. Tech Neurosurg. 1995;1:117-122.
33 Paramore CG, Dickman CA, Sonntag VKH. Radiographic and clinical follow-up review of Caspar plates in 49 patients. J Neurosurg. 1996;84:957-961.
34 Harkey HL, Caspar W, Tarassoli Y. Caspar plating of the cervical spine. In: Rengachary SS, Wilkins RH, editors. Neurosurgical Operative Atlas. Park Ridge, IL: American Association of Neurological Surgeons; 1992:261-271.
35 Xu R, Ebraheim NA. Essential bony anatomy of the cervical spine relative to instrumentation. Neurosurg Q. 1998;8:172-179.
36 Pait TG, Killefer JA, Arnautovic KI. Surgical anatomy of the anterior cervical spine: the disc space, vertebral artery, and associated bony structures. Neurosurgery. 1996;39:769-776.
37 Golfinos JG, Dickman CA, Zabramski JM, et al. Repair of vertebral artery injury during anterior cervical decompression. Spine. 1994;19:2552-2556.
38 Benzel EC. Qualitative attributes of spinal implants. In: Benzel EC, editor. Biomechanics of Spine Stabilization: Principles and Clinical Practice. New York: McGraw-Hill; 1995:135-150.
39 Prolo DJ. Biology of bone fusion. Clin Neurosurg. 1990;36:135-146.
40 Kaufman HH, Jones E. The principles of bony spinal fusion. Neurosurgery. 1989;24:264-270.
41 Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1955;96:223-224.
42 Wolff J, Maquet P, Furlong R. The Law of Bone Remodeling. Berlin: Springer-Verlag; 1986.
43 Dougherty PJ, Jones AAM, Sharkey N, et al. Iliac crest bone graft: osteotome versus saw. 20th Annual Meeting of Cervical Spine Research Society; Palm Desert, CA, December 3-5; 1992.
44 Brodke DS, Klimo PJr, Bachus KN, et al. Anterior cervical fixation: analysis of load-sharing and stability with use of static and dynamic plates. J Bone Joint Surg Am. 2006;88:1566-1573.
45 Bohler J, Gaudernak T. Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma. 1980;20:203-205.
46 Caspar W. Advances in cervical spine surgery. First experiences with trapezoidal osteosynthetic plate and a new surgical instrumentation for anterior interbody stabilization. Orthop News. 1982;4:7-8.
47 Harkey HL. Bicortical anterior cervical plate fixation. Tech Neurosurg. 1995;1:108-116.
48 Renachary SS. Anterior stabilization of the cervical spine using a locking plate system. In: Rengachary SS, Wilkins RH, editors. Neurosurgical Operative Atlas. Park Ridge, IL: American Association of Neurological Surgeons; 1993:423-434.
49 Lowery KL. Stabilization of the cervical spine with the Orion anterior cervical plate system. In: Rengachary SS, Wilkins RH, editors. Neurosurgical Operative Atlas. Park Ridge, IL: American Association of Neurological Surgeons; 1996:101-108.
50 Hurlbert RJ, Sonntag VKH. Anterior cervical spine stabilization with the Codman locking plate system. In: Rengachary SS, editor. Neurosurgical Operative Atlas. Park Ridge, IL: American Association of Neurological Surgeons; 1997:157-165.
51 Apfelbaum RI, Dailey AT, Barbera J. Clinical experience with a new load-sharing anterior cervical plate. Salt Lake City, UT: 27th Annual Meeting of the Cervical Spine Research Society; 1999.
52 Bulger RF, Rejowski JE, Beatty RA. Vocal cord paralysis associated with anterior cervical fusion: considerations for prevention and treatment. J Neurosurg. 1985;62:657-661.
53 Flynn TB. Neurological complications of anterior cervical interbody fusion. Spine. 1982;7:536-539.
54 Dickman CA, Fessler RG, MacMillan M, et al. Transpedicular screw-rod fixation of the lumbar spine: operative technique and outcome in 104 cases. J Neurosurg. 1992;77:860-870.
55 McAfee PC, Farey ID, Sutterlin CE, et al. 1989 Volvo Award in basic science. Device-related osteoporosis with spinal instrumentation. Spine. 1989;14:919-926.