Chapter 150 Ankylosing Spondylitis and Other Spondyloarthritides
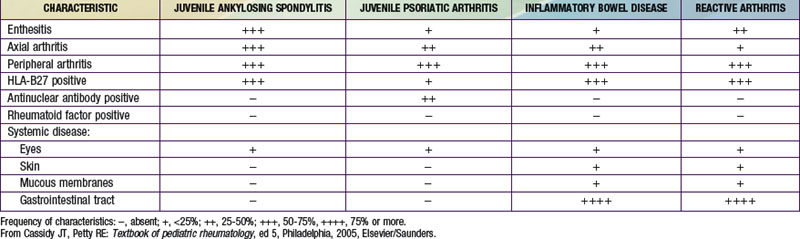
The diseases collectively referred to as spondyloarthritides include ankylosing spondylitis (AS), arthritis associated with inflammatory bowel disease (IBD) and psoriasis, and reactive arthritis following gastrointestinal or genitourinary infections (see Table 150-1 on the Nelson Textbook of Pediatrics website![]() at www.expertconsult.com). Pediatric rheumatologists have adopted the International League of Associations for Rheumatology (ILAR) classification scheme for juvenile idiopathic arthritis (JIA) and use the term enthesitis-related arthritis (ERA) to encompass most forms of spondyloarthritis in children, except those with co-existing psoriasis.
at www.expertconsult.com). Pediatric rheumatologists have adopted the International League of Associations for Rheumatology (ILAR) classification scheme for juvenile idiopathic arthritis (JIA) and use the term enthesitis-related arthritis (ERA) to encompass most forms of spondyloarthritis in children, except those with co-existing psoriasis.
Etiology and Pathogenesis
Spondyloarthritides are complex genetic diseases in which susceptibility is largely genetically determined. HLA-B27 is responsible for around 40% of AS susceptibility, with genes encoding the interleukin-23 (IL-23) receptor (IL23R), ERAP1 (endoplasmic reticulum aminopeptidase-1; also known as ARTS-1 [type 1 tumor necrosis factor receptor shedding aminopeptidase regulator]), IL-1α (IL1A), and others playing important roles. Enteric infection with certain gastrointestinal or genital pathogens can trigger reactive arthritis (Chapter 151); environmental triggers for other forms of spondyloarthritis have not been identified. Although molecular mimicry between HLA-B27 and antigens from bacteria has been postulated as an underlying mechanism of disease, evidence supporting this hypothesis is scarce. Other unusual properties of HLA-B27, such as its tendency to misfold and form unusual cell surface structures, may play a role.
Clinical Manifestations
Enthesitis-Related Arthritis
Children are classified as having ERA if they have either arthritis and enthesitis or arthritis or enthesitis, with two of the following additional characteristics: (1) sacroiliac joint tenderness or inflammatory lumbosacral pain (see Table 150-1), (2) the presence of HLA-B27, (3) age > 6 yr and male sex, (4) acute anterior uveitis, and (5) a family history of an HLA-B27–associated disease (ERA, sacroiliitis with IBD, reactive arthritis, or acute anterior uveitis) in a first-degree relative. Patients with psoriasis (or a family history of psoriasis in a first-degree relative), a positive rheumatoid factor (RF) test result, or systemic arthritis are excluded from this group. Many children with ERA go on to eventually have AS, but many do not, and it is not currently possible to determine whose ERA will progress.
Juvenile Ankylosing Spondylitis
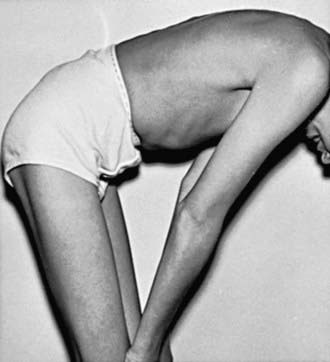
JAS frequently begins with oligoarthritis and enthesitis. The arthritis occurs predominantly in the lower extremities and often involves the hips, in contrast to oligoarticular JIA. Also unlike in adult-onset AS, in JAS axial involvement is usually absent until later in the disease course (Fig. 150-1). Enthesitis is particularly common, manifesting as localized and often severe tenderness at characteristic tendon (as well as ligament, fascia or capsule) insertions around the plantar surface of the foot, ankle (Achilles), and knee (patella). The disease course is variable and can include periods of low disease activity. Fever and weight loss are uncommon and, if present, raise the possibility of IBD.
Psoriatic Arthritis
Psoriatic arthritis is equally common in girls and boys, and arthritis can precede psoriasis. The most common presentation is asymmetric arthritis involving < 5 joints. Both large (knee, ankle) and small (finger, toe) joints can be involved, including distal interphalangeal joints. The presence of HLA-B27 is not a risk factor for psoriasis, and most patients with psoriatic arthritis do not have axial involvement. However, when HLA-B27 is present, axial arthritis is more common. In a child with oligoarthritis or even polyarthritis, the presence of nail pitting (Fig. 150-2), dactylitis, onycholysis, and/or a family history of psoriasis supports the diagnosis of psoriatic arthritis.
Laboratory Findings
Early radiographic changes in the sacroiliac joints include indistinct margins and erosions, with sclerosis typically starting on the iliac side of the joint (Fig. 150-3). Peripheral joints may exhibit periarticular osteoporosis, with loss of sharp cortical margins in areas of enthesitis, which may eventually show erosions or bony spurs. Squaring of the corners of the vertebral bodies and the classic “bamboo spine,” with syndesmophyte formation and calcification of ligaments characteristic of advanced AS, develop later. These findings are rare in early disease, particularly in childhood.
Diagnosis
Spondyloarthritis is suggested by the onset of oligoarthritis and/or enthesitis in an older boy. The arthritis predominantly affects hips, knees, ankles, and feet (often the intertarsal joints). When the axial skeleton is involved, patients may experience inflammatory back pain, which is characterized by nighttime pain and considerable morning stiffness that is improved by activity and worsened by rest (Table 150-2). With progressive disease there is a loss of the normal lumbar lordosis, inability to touch the toes with the legs straight, and sacroiliac pain on palpation or with pelvic compression. AS is diagnosed if there is sufficient radiographic evidence of sacroiliitis and the patient meets at least one clinical criterion involving inflammatory back pain, limitation of motion in the lumbar spine, or limitation of chest expansion. JAS is present if the patient is <16 yr. The term juvenile-onset AS is frequently used to describe AS when the symptoms begin before age 16 yr but full criteria for a diagnosis are not met. Because radiographic evidence of sacroiliitis can take 10 yr or longer to develop and clinical manifestations may be subtle, it can be difficult to differentiate spondyloarthritis from JIA early in the disease course. Efforts to establish criteria that are more sensitive for diagnosing axial spondyloarthritis with MRI and use of other clinical features and markers are underway.
In a child with chronic arthritis, the presence of erythema nodosum, pyoderma gangrenosum, fever, weight loss, or anorexia suggests IBD. The onset of arthritis following a recent history of diarrhea, and symptoms of urethritis or conjunctivitis may suggest reactive arthritis. Psoriasis, nail changes (see Fig. 150-2), or a family history of psoriasis suggests psoriatic arthritis. Early differentiation between the various forms of spondyloarthritis by laboratory or radiographic means is difficult. Sacroiliac joint involvement or enthesitis, including adjacent bone marrow edema, may be seen on MRI, and results of a technetium Tc 99m bone scan may be positive, but results of the latter examination are often difficult to interpret in children and adolescents.
Differential Diagnosis
Lower back pain can be caused by suppurative arthritis of the sacroiliac joint, osteomyelitis of the pelvis or spine, osteoid osteoma of the posterior elements of the spine, pelvic muscle pyomyositis, or malignancies. In addition, mechanical conditions such as spondylolysis, spondylolisthesis, and Scheuermann disease should be considered. Back pain secondary to fibromyalgia usually affects the soft tissues of the upper back in a symmetric pattern and is associated with well-localized tender points (Chapter 671.5).
Braun J, Sieper J. Ankylosing spondylitis. Lancet. 2007;369:1379-1390.
Gensler L, Ward MM, Reveille JD, et al. Clinical, radiographic and functional differences between juvenile-onset and adult-onset spondylitis: results from the PSOAS (Prospecitive Study of AS Outcomes) Cohort. Ann Rheum Dis. 2008;67:233-237.
Hofer M. Spondyloarthropathies in children—are they different from those in adults? Best Pract Res Clin Rheumatol. 2006;20:315-328.
Ravelli A, Martini A. Juvenile idiopathic arthritis. Lancet. 2007;369:767-778.
Sacks J, Helmick C, Yao-Hua L, et al. Prevalence of and annual ambulatory health care visits for pediatric arthritis and other rheumatologic conditions in the US in 2001–2004. Arth Rheum. 2007;57:1439-1445.
Smith JA, Marker-Hermann E, Colbert RA. Pathogenesis of ankylosing spondylitis: current concepts. Best Pract Res Clin Rheumatol. 2006;20:571-591.
Tse SML, Burgos-Vargas R, Laxer RM. Anti-tumor necrosis factor-α blockade in the treatment of juvenile spondyloarthropathy. Arth Rheum. 2005;52:2103-2108.