Chapter 4 ANEMIA
General Discussion
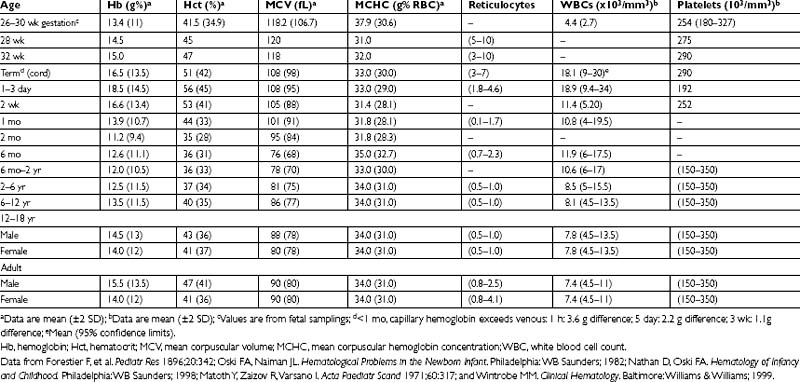
Anemia is a frequent laboratory abnormality in children, affecting as many as 20% of children in the United States and as many as 80% of children in developing countries. Anemia is defined as a decreased concentration of hemoglobin and red blood cell (RBC) mass compared with age-matched controls. Age-specific blood cell indices are outlined below in Table 4-1.
Medications Associated with Anemia
Acetylsalicylic acid (in patients with G6PD deficiency)
Antibacterials (in patients with G6PD deficiency)
Antimalarials (in patients with G6PD deficiency)
Human immunodeficiency virus (HIV) medications
Methylene blue (in patients with G6PD deficiency)
Phenacetin (in patients with G6PD deficiency)
Phenazopyridine (in patients with G6PD deficiency)
Probenacid (in patients with G6PD deficiency)
Key Physical Findings
 Measurement of weight, height, and head circumference to evaluate for growth delay
Measurement of weight, height, and head circumference to evaluate for growth delay
 General impression of well-being, noting irritability or pallor
General impression of well-being, noting irritability or pallor
 Assessment of developmental stage
Assessment of developmental stage
 Head and neck examination for scleral icterus or glossitis
Head and neck examination for scleral icterus or glossitis
 Cardiopulmonary examination for tachycardia, tachypnea, or murmurs. Acute anemia may present with signs of congestive heart failure or hypovolemia
Cardiopulmonary examination for tachycardia, tachypnea, or murmurs. Acute anemia may present with signs of congestive heart failure or hypovolemia
 Abdominal examination for fullness, hepatomegaly, or splenomegaly
Abdominal examination for fullness, hepatomegaly, or splenomegaly
Suggested Work-Up
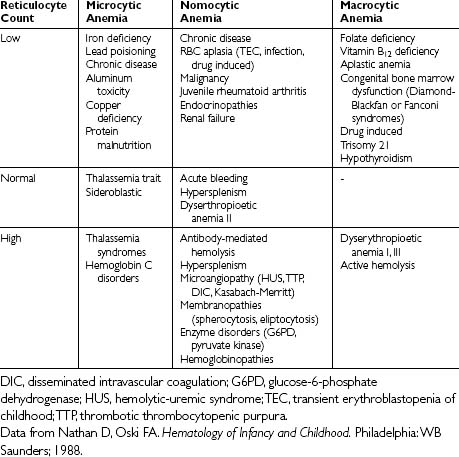
| Complete blood cell count (CBC) evaluation of the mean corpuscular volume (MCV) | When a low hemoglobin level is detected, evaluation of the MCV may be used to classify the anemia further as microcytic, normocytic, or macrocytic. The differential diagnosis of each is presented in Table 4-2 |
| Peripheral smear | Pathologic findings on the smear can indicate the cause of the anemia based on RBC morphology. For example, basophilic stippling is seen in thalassemia, whereas Howell-Jolly bodies are seen in asplenia, pernicious anemia, and severe iron deficiency anemia |
| Reticulocyte count | The reticulocyte count helps distinguish a hypoproductive anemia (decreased RBC production) versus a destructive process (increased RBC destruction). A low reticulocyte count may indicate bone marrow disorders or aplastic crisis, whereas a high count generally indicates a hemolytic process or active blood loss |
| There usually is a natural increase in RBC production in response to anemia. The corrected reticulocyte count is the reticulocyte count × (hematocrit [Hct]/normal Hct). This corrected reticulocyte count is generally >2%. A low count is suggestive of chronic anemia/hemolysis or a marrow problem |
Additional Work-Up
| Iron studies (ferritin, iron, total iron-binding capacity [TIBC]) | If iron deficiency is suspected, a trial of treatment with iron supplementation followed by a repeat CBC is also reasonable. An increase in hemoglobin levels of greater than 1.0 g/dL by 4 weeks is diagnostic of iron deficiency |
| Coombs’ test | To evaluate for autoimmune hemolytic anemia |
| G6PD assay | If G6PD deficiency is suspected |
| Hemoglobin electrophoresis | If a hemoglobinopathy is suspected |
| LDH, total bilirubin, indirect bilirubin, haptoglobin, and reticulocyte count. |
1. Irwin J.J., Kirchner J.T. Anemia in children. Am Fam Physician. 2001;64:1379–1386.
2. Robertson J., Shilkofski N. The Harriet Lane Handbook: A Manual for Pediatric House Officers, 17th ed. St. Louis: Mosby; 2005. 73-104
3. Segel G.B., Hirsh M.G., Feig S.A. Managing anemia in pediatric office practice: part 1. Pediatr Rev. 2002;23:75–84.
4. Segel G.B., Hirsh M.G., Feig S.A. Managing anemia in pediatric office practice: part 2. Pediatr Rev. 2002;23:111–122.