Local and Regional Control in Breast Cancer: Role of Sentinel Node Biopsy
Breast cancer is the most common malignancy and the second most common cause of cancer deaths in American women. The American Cancer Society estimates that 207,090 new cases of invasive breast cancer and 40,230 breast cancer deaths are expected in 2010 [1]. In patients with primary breast cancer, axillary lymph node status remains one of the most important prognostic indicators.
Nodal status has traditionally been determined by levels I and II axillary lymph node dissection (ALND). This procedure has been virtually replaced by the far-less morbid sentinel lymph node dissection (SLND). This technique was first described by Morton and colleagues [2] in 1992 for clinical stage I cutaneous melanoma. SLND is based on the hypothesis that the first node draining the primary tumor reflects the tumor status of the regional lymphatic nodal basin. This technique was adapted to breast cancer by Giuliano and colleagues [3].
Patient selection
The American Society of Clinical Oncology (ASCO) published guidelines for lymphatic mapping and SLND [4]. Routine SLND is acceptable for early-stage breast cancer in patients with clinically node-negative disease. The guidelines are summarized in Table 1. There is a debate on the timing of SLND in patients undergoing neoadjuvant chemotherapy (NAC). According to the ASCO guidelines, SLND is considered an option before, but not after, preoperative chemotherapy. However, practice patterns differ, with many clinicians performing SLND before or after NAC. Data can support either option. The National Cancer Institute Conference concluded that SLND can be performed before or after preoperative chemotherapy in patients with clinically node-negative cancer [5].
| Clinical circumstance | Recommendation for use of SNB | Level of evidencea |
|---|---|---|
| T1 or T2 tumors | Acceptable | Good |
| T3 or T4 tumors | Not recommended | Insufficient |
| Multicentric tumors | Acceptable | Limited |
| Inflammatory breast cancer | Not recommended | Insufficient |
| DCIS with mastectomy | Acceptable | Limited |
| DCIS without mastectomy | Not recommended except for large DCIS (>5 cm) on core biopsy or with suspected or proven microinvasion | Insufficient |
| Suspicious, palpable axillary nodes | Not recommended | Good |
| Older age | Acceptable | Limited |
| Obesity | Acceptable | Limited |
| Male breast cancer | Acceptable | Limited |
| Pregnancy | Not recommended | Insufficient |
| Evaluation of internal mammary lymph nodes | Acceptable | Limited |
| Prior diagnostic or excisional breast biopsy | Acceptable | Limited |
| Prior axillary surgery | Not recommended | Limited |
| Prior nononcologic breast surgery (reduction or augmentation mammoplasty, breast reconstruction, and so forth) | Not recommended | Insufficient |
| After preoperative systemic therapy | Not recommended | Insufficient |
| Before preoperative systemic therapy | Acceptable | Limited |
Abbreviations: DCIS, ductal carcinoma-in situ; SNB, sentinel lymph node biopsy.
From Lyman G, Giuliano AE, Somerfield M, et al. American Society of Clinical Oncology Guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol 2005;23:7703–20; with permission.
Technical aspects of SLND
Radioactive tracer requires a nuclear medicine team and preoperative injection and is the most commonly used technique. Technetium Tc 99m–labeled sulfur colloid [6] or albumin colloid [7,8] is injected in peritumoral, intradermal, or subareolar location 2 to 24 hours before surgery. The axillary drainage pattern is visualized on a lymphoscintigram or detected intraoperatively with a gamma counter. The skin incision is made, and in vivo radioactivity of the axillary nodal basin is reevaluated. A radioactive node is variably defined as the hottest node by absolute counts, a 10:1 ratio of sentinel node to background, a 4-fold reduction in count after sentinel node removal, or a 10-second count greater than 25 [6–10]. Any suspicious nodes that did not take up the dye or colloid should also be removed because cancer-filled nodes may not take up dye or colloid.
Grube and Giuliano [11] reviewed early published studies with 100 or more subjects reporting the identification and accuracy of SLND using vital dye, gamma probe–guided surgery or combined technique, followed by completion ALND for invasive breast cancer. The overall false-negative sentinel node identification rate ranged from 0% to 14.3%, and the accuracy ranged from 93% to 100%. Potential factors contributing to failure to identify sentinel node include variable lymphatic drainage pattern, patient or tumor characteristics, surgical technique, surgeon training, and pathologist experience.
The primary site of lymphatic drainage from the breast is the axilla. However, 1.3% to 9.9% isolated internal mammary drainage has been reported [8,12–15]. In a human cadaver study evaluating the lymphatic drainage of the breast [16], the lymphatics of the nipple-areola complex did not drain into the same nodes that receive the lymphatic drainage passing through the breast. At present, there is no consensus regarding the ideal sites for dye or radioactive colloid injection [17–19]. In practice, peritumoral [3,6], intradermal [7,20,21], or subareolar [22,23] injections seem equally effective to identify axillary nodes. However, peritumoral injections lead to better identification of the internal mammary nodes when compared with intradermal or subareolar injections [21,24–27]. Subareolar injection is regarded as a good choice for sentinel node identification for a multicentric disease [28].
Several studies have evaluated the proportion of successful SLND with blue dye, radiocolloid, or combination of dye with isotope with respect to sentinel node identification rate, accuracy, and/or false-negative rate. In the American College of Surgeons Oncology Group (ACOSOG) Z0010 trial, 5237 patients underwent SLND. Blue dye alone was used in 14.8%, radiocolloid alone in 5.7%, and the combination of dye with isotope in 79.4%. No statistically significant difference in sentinel node identification failure rate was seen (1.7%, 2.3%, and 1.2% for the blue dye, radiocolloid, and the combination of dye with isotope, respectively) [29]. Morrow and colleagues [30] performed a randomized trial comparing the use of blue dye alone with that of combined dye and isotope. The success rate of sentinel node biopsy was higher with combined mapping than with blue dye alone (100% vs 86%, P = .002). The accuracy and false-negative rates were similar. An accuracy of 100% for combined mapping versus 98% for blue dye and a false-negative rate of 0% for combined mapping versus 5% for blue dye were observed. In a study by Meyer-Rochow and colleagues [31], similar identification rates, accuracies, and sensitivities were reported with blue dye alone and triple modality, consisting of preoperative lymphoscintigraphy, intraoperative gamma probe, and intraoperative blue dye.
The accuracy of SLND depends greatly on the proficiency of the surgeon performing the procedure [32]. A learning curve exists, and surgeons master the procedure at different rates. According to the American Society of Breast Surgeons guidelines [33,34], 20 cases of SLND with back-up ALND with an identification rate of 85% and a false-negative rate less than 5% are recommended before abandoning ALND. However, the widespread use of this technique and its teaching in training programs have made these recommendations obsolete.
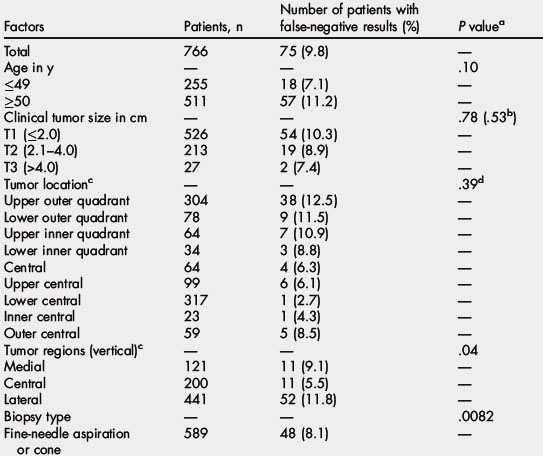
Studies have shown that increasing the number of sentinel nodes removed may increase accuracy and decrease false-negative rates [35–37]. In the National Surgical Adjuvant Breast and Bowel Project (NSABP) B-32 trial, the false-negative rate was 17% for removal of 1 sentinel node, 10% for 2 removal of nodes, 6.9% for removal of 3 nodes, 5.5% for removal of 4 nodes, and 1% for removal of 5 or more nodes [35]. Zakaria and colleagues [36] evaluated how many sentinel nodes are enough in SLND for breast cancer and found that 98% of patients with lymph node metastasis were identified by the third node and 100% by the fourth node. They concluded that terminating the procedure at the fourth node may reduce the morbidity of the procedure. Chagpar and colleagues [37] evaluated whether removing 3 sentinel nodes is sufficient. When SLND was limited to the first 3 nodes, the false-negative rate was 10.3% in this University of Louisville Breast Cancer Sentinel Lymph Node Study. The investigators concluded that removal of only 3 nodes cannot be recommended. Controversy exists regarding how many nodes are sufficient for accurate staging of the axilla. In general, all blue nodes or nodes at the end of blue lymphatic channel, hot nodes or nodes with radioactive counts greater than 10% of the hottest node, and any palpably suspicious nodes should be removed. Increasing the number of nodes removed increases the probability of removing the sentinel node, but experienced surgeons may need to remove only 1 node for a successful sentinel node identification.
Impact of patient and tumor characteristics on SLND success
Several studies evaluated the patient and tumor characteristics associated with SLND success and failure. Age 70 years or older and increased body mass index (BMI), defined as the weight in kilograms divided by the height in meters squared, were associated with SLND failure in the ACOSOG Z0010 trial [29]. The differences in tumor location, the type of biopsy, and the number of SLNs removed significantly affected the false-negative rate in the NSABP B-32 trial [35]. The study result is summarized in Table 2. In the Axillary Mapping Against Nodal Axillary Clearance (ALMANAC) study, SLND success decreased with increasing BMI, tumor location other than the upper outer quadrant, and nonvisualization of hot nodes on the preoperative lymphoscintigraphy [38].
The role of SLND in axillary staging
The purpose of the NSABP B-32 trial is to establish whether SLND can achieve the same therapeutic goals as conventional ALND but with less morbidity [35]. A total of 5611 women with clinically node-negative operable breast cancer were randomized to SLND followed by ALND or to observation if the sentinel node was tumor free. The overall survival, disease-free survival, and regional control were statistically equivalent between the groups. When the sentinel node is histologically tumor free, SLND alone with no further ALND is an appropriate, safe, and effective therapy for patients with clinically node-negative breast cancer [39]. The morbidity results comparing SLND and ALND were recently reported [40]. The shoulder abduction deficit greater than 10% peaked at 1 week for the ALND (75%) and SLND (41%) groups. Arm volume difference of greater than 10% was seen at 36 months for the ALND (14%) and SLND (8%) groups. The rate of numbness peaked at 6 months for the ALND (49%) and SLND (15%) groups. These results indicate the superiority of SLND with respect to surgical morbidity outcomes over a 3-year follow-up period. The secondary end points were accuracy and technical success. A 97.2% sentinel node identification rate and 9.8% false-negative rate were reported. Only 1.4% of the sentinel nodes were found outside of the axillary levels I and II.
The ALMANAC trial quantified the detection and false-negative rates of SLND and evaluated the factors influencing them [38]. A total of 842 patients with clinically node-negative breast cancer underwent SLND using the combined technique of dye and isotope. SLND was followed by immediate ALND. The study reported a 96.1% sentinel node identification rate, 97.6% accuracy, and 6.7% false-negative rate. The factors influencing false-negative rate were tumor grade (9.3% for grade 3 tumor vs 4.7% for grade 2 tumor) and the number of sentinel nodes harvested (10.1% for 1 node vs 1.1% for 3 or more nodes).
The Royal Australian College of Surgeons’ multicenter trial of the Sentinel Node versus Axillary Clearance (SNAC) was a randomized one designed to determine if sentinel node biopsy produces less morbidity and equivalent cancer-related outcomes when compared with immediate axillary clearance in women with early-stage breast cancer [41]. Stage 1 tested the performance measures for SLND and found 5% false-negative rate, 95% sensitivity, and 98% negative predictive value. Stage 2 was a randomized controlled trial of SLND alone versus axillary clearance in women with clinically node-negative breast cancer less than 3 cm. The SNAC trial had insufficient power on its own to detect differences in recurrence and survival. Given the low false-negative rate, the differences will likely be small. SLND resulted in accurate axillary staging with less morbidity [42].
The Italian Sentinella/Gruppo Interdisciplinare Veneto Oncologia Mammaria (GIVOM) study was a multicenter randomized trial that assessed the efficacy and safety of SLND compared with ALND [43]. A total of 749 patients with breast cancer less than 3 cm were randomly assigned to SLND associated with ALND or SLND followed by ALND only if sentinel node was metastatic. Data were available for review in 697 patients. A 95% sentinel node identification rate and a 16.7% false-negative rate were reported. There were more locoregional recurrences (LRR) in the SLND arm (16 of 345 patients) when compared with the ALND arm (3 of 352 patients). Postoperative side effects were significantly less in the SLND group. The 5-year disease-free survival was 89.9% in the ALND arm and 87.6% in the SLND arm. The number of enrolled patients was not sufficient to draw definitive conclusions in this study.
Histopathologic analysis of the sentinel node
The College of American Pathologists published guidelines for processing sentinel nodes [44]. The SLNs should be sectioned as close to 2 mm as possible, embedded in paraffin, and stained with hematoxylin-eosin (H&E). Although commonly performed, routine cytokeratin staining of histologically negative SLNs should not be considered the standard until clinical trials demonstrate its clinical significance. For the intraoperative assessment of SLNs, careful gross examination with cytologic evaluation (imprint cytology) is preferable to frozen section examination, which may consume significant amount of nodal tissue.
When metastases are detected in the sentinel node, the size of the metastasis and the method of detection are reported according to the new American Joint Committee on Cancer guidelines [45]. ITCs are defined as small clusters of cells 0.2 mm or less, single tumor cells, or a cluster of less than 200 cells in a single histologic cross-section. ITCs may be detected by routine histology or by immunohistochemical (IHC) methods. Positive molecular findings refer to tumor cells identified by reverse-transcriptase polymerase chain reaction but not detected by histology or IHC. Micrometastases are greater than 0.2 mm and/or more than 200 cells, but none are greater than 2 mm.
SLND and axillary recurrence in patients with sentinel node-negative cancer
At present, there are little long-term follow-up data from large multicenter randomized trials that compare axillary failure rates for SLND and ALND. However, there are several single institution studies and a few multicenter trials with short-term follow-up data that show lower-than-expected axillary recurrence in the SLND-alone arm. These studies suggest that SLND may play a role in providing regional nodal control for sentinel node-negative cancer [29,46–51].
Giuliano and colleagues [46] were the first to report a prospective study to evaluate the safety and feasibility of SLND as a replacement for ALND in women with histopathologically node-negative cancer. A total of 133 women with breast cancers 4 cm or less and clinically negative nodes were entered into a trial of SLND with vital blue dye. Sentinel nodes were examined by standard microscopy or IHC. In 67 patients with histopathologically tumor-free sentinel nodes, SLND was the only axillary procedure. Adjuvant systemic therapy was administered to 33 patients (49%). No axillary irradiation was given. At a 39-month follow-up, no local or axillary recurrence was noted. If nonsentinel nodes harbored metastatic disease, a higher rate of axillary recurrence should have been observed. In the NSABP-04 study, the axillary recurrence rate after total mastectomy without radiation therapy was 18%, with more than three-quarters developing axillary recurrence within the first 24 months [52]. Among the 57 patients with positive sentinel nodes in the ALND group, 26 patients (46%) had macrometastases (>2 mm) and 31 patients (54%) had micrometastases (≤2 mm). This was the first study to evaluate SLND as the only axillary procedure in patients with histopathologically node-negative cancer and provided evidence that suggests that ALND is not required in these patients. SLND provided accurate staging without sacrificing axillary control.
Following this initial report, Hansen and colleagues [53] reported outcome data for 238 patients who underwent breast conserving therapy and SLND without completion of ALND. These patients were sentinel node negative by both H&E and IHC stains. About 85% had T1 tumor and 15% had T2 tumor. Around 66.4% of the patients received adjuvant systemic therapy. At a median follow-up of 38.9 months, no axillary recurrence was observed. About 98.3% of patients were alive without evidence of disease. SLND provided excellent regional control in patients with early node-negative breast cancer.
Veronesi and colleagues [50] published a single-institution phase 3 study with a 10-year follow-up. A set of 516 patients with tumor up to 2 cm were randomized to SLND followed by ALND or SLND only if sentinel node is negative. Only 2 cases of axillary recurrence were reported. Both cases occurred in the SLND group (0.77%). Among the 174 patients in the ALND arm, 8 patients (5%) were found to have false-negative results sentinel nodes. A similar number of patients (8 patients) with axillary involvement was expected in SLND group because the 2 arms (ALND and SLND) were well balanced for number of sentinel nodes found, proportion of positive sentinel nodes, and all other tumor and patient characteristics. There were a total of 49 breast cancer–related events, 23 in the SLND group and 26 in the ALND group (P = .52). There was no difference between the 2 groups with respect to disease-free survival (89.9% in the SLND group vs 88.8% in the ALND group). The overall survival was slightly greater in the SLND arm, 93.5%, compared with the ALND arm, 89.7%, but this was not statistically significant (P = .15).
Zavagno and colleagues [47] reported 479 patients from 5 institutions with early-stage breast cancer and negative sentinel node who had SLND alone. No clinical axillary recurrence was found at a median follow-up of 35.8 months. A mean of 1.4 sentinel nodes were removed. About 90.6% of the patients received systemic therapy.
In a Swedish Multicenter Cohort Study by Bergkvist and colleagues [48], 3534 patients with breast cancer less than 3 cm were prospectively studied. It was reported that 2246 patients had tumor-free sentinel node and underwent SLND alone. A total of 26 hospitals and 131 surgeons contributed to the patient accrual. At a median follow-up of 37 months, 27 patients (1.2%) had axillary recurrence. Of these 27 patients, 13 had isolated axillary recurrence, 7 had axillary and local recurrence in the breast, and 7 had axillary and distant metastases. An overall survival of 92.1% and a disease- free survival of 91.6% were reported.
Researchers at the Memorial Sloan-Kettering Cancer Center (MSKCC) reported their experience with 4008 consecutive SLNDs [49]. There were 326 patients with tumor-free sentinel nodes who had ALND and 2340 patients with tumor-free sentinel nodes who had SLND only. At a median follow-up of 31 months, 0.12% axillary recurrence was reported in the SLND group.
A systematic review and meta-analysis of 48 studies with 14,959 patients who were sentinel node negative and did not undergo ALND was reported by Van der Ploeg and colleagues [51]. At a median follow-up of 34 months, a 0.3% axillary failure rate was reported.
The ACOSOG Z0010 trial is one of the largest trials of SLND involving 5237 patients with clinically node-negative breast cancer [29]. This is a prospective multicenter observational study to determine the clinical significance of sentinel node and bone marrow metastases. Patients underwent lumpectomy and sentinel node biopsy with bilateral iliac crest bone marrow aspiration. Bone marrow and histologically negative sentinel nodes were evaluated with IHC in a central laboratory. The overall survival, disease-free survival, and LRR were determined. At a median follow-up of 31 months, axillary recurrence occurred in only 0.2% of the patients with sentinel node-negative cancer.
SLND and axillary recurrence in patients with sentinel node-positive cancer
Several studies have reported short-term outcomes in patients with sentinel node-positive cancer who did not undergo completion ALND [49,54,55]. Park and colleagues [54] evaluated 287 patients with SLN-positive cancer who did not undergo ALND (SLN+/no ALND) at MSKCC. This was an observational nonrandomized study. Patients in SLN+/no ALND group were older (59 years vs 52 years, P<.001), had more favorable tumors, were more likely to have breast conservation (68% vs 55%, P<.001), and had a marginally higher rate of axillary LRR (2% vs 0.4%, P = .004) at 23 to 30 months’ follow-up when compared with the SLN+/ALND group [54]. In both groups, half of all axillary recurrences occurred as the only site of disease recurrence, whereas the remainder of axillary recurrences were coincident with ipsilateral breast recurrence or with distant relapse. In SLN+/no ALND group, SLND alone had a 9% predicted likelihood of residual axillary disease by MSKCC nomogram but an observed axillary local recurrence of only 2%, suggesting that the nomogram does not predict axillary recurrence rate accurately.
Naik and colleagues [49] reported 1.4% axillary recurrence rate at a median follow-up of 31 months in 210 patients with SLN-positive cancer who declined ALND. In these patients, the axillary recurrence was infrequent in both those who had completion ALND and those who did not, 0.35% and 1.4%, respectively.
There are several reports of the subset of patients with SLN-positive cancer who were older, had smaller tumors, less-frequent lymphovascular invasion, and lower volume SLN metastases who did not undergo completion ALND and had a 0% axillary recurrence [55–57]. Fant and colleagues [55] performed a retrospective review of 31 patients with SLN-positive cancer who declined ALND. Most primary tumors were T1. A total of 27 patients had microscopic (<2 mm) metastases and 4 patients had macroscopic metastases found in the sentinel nodes. No axillary recurrences were detected at a 30-months follow-up. Guenther and colleagues [56] studied 46 women with SLN metastases who did not undergo ALND. The mean age was 61.6 years, mean tumor size was 1.65 cm, and 87% of the patients had estrogen receptor–positive tumor. Seven patients (15%) had macrometastases (>2 mm), 16 (35%) had micrometastases (≤2 mm), and 23 (50%) had cellular metastases. Only 16 positive SLNs (35%) were seen on H&E staining, whereas 30 SLNs (65%) had positive IHC staining. No axillary recurrence was observed. One patient (2%) developed distant metastases during a 32-month follow-up. Winchester and colleagues [57] studied 73 patients with SLN metastases who omitted completion ALND. No axillary recurrence was reported at a 27.6-month follow-up. The mean age was 59 years, mean tumor size was 1.9 cm, median size of nodal metastasis was 1 mm, and 79% of the patients had estrogen receptor–positive tumors. Standard breast irradiation was given in 92% of the patients. These studies suggested that there is a low-risk subset of patients with metastatic SLNs who do not need completion ALND.
The NSABP B-04 trial randomized women with clinically node-negative cancer to radical mastectomy, total mastectomy with axillary irradiation, or total mastectomy [58]. Adjuvant systemic therapy was not routinely given. About 38% of women who underwent axillary dissection (radical mastectomy group) were found to have axillary nodal metastases. Because this was a randomized study, it was assumed that the other 2 groups had similar rates of axillary nodal metastases. The 10-year axillary recurrence rate after total mastectomy was 18%, with more than three-quarters of recurrence observed in less than 2 years. This study suggested that not all axillary metastases progress to become clinically evident. Patients with axillary recurrence underwent ALND. No statistically significant effect of locoregional control on survival was found when 3 groups were compared [52].
Martelli and colleagues [59] performed a randomized trial comparing axillary dissection with no axillary dissection in women 65 years or older with T1 tumors and clinically negative nodes. A total of 219 women were randomized to breast-conserving surgery with or without axillary dissection. Tamoxifen was prescribed to all patients for 5 years, although 12% of them had estrogen receptor–negative cancer. At a 60-month follow-up, 2 patients (1.8%) in the no ALND arm developed axillary recurrence and 23% of the patients in the ALND arm had nodal metastases. This result suggests that not all axillary nodal metastases progress. There was no statistically significant difference in breast cancer mortality, overall survival, or crude cumulative incidence of breast events between the groups.
The International Breast Cancer Study Group (IBCSG) 10-93 randomized 473 patients 60 years or older with clinically node-negative cancer into primary surgery and ALND (ALND) or surgery without ALND (no ALND). Tamoxifen was given for 5 years in both groups. The median age was 74 years; 80% had estrogen receptor–positive disease. The primary end point was quality of life (QL) reported by the patient and by physician assessment. At a median follow-up of 6.6 years, ALND and no ALND groups yielded similar disease-free survival, 67% versus 66%, and similar overall survival, 75% versus 73%. About 28% of patients in the ALND group had involved nodes. Axillary recurrence was observed in 1% of ALND and 3% of no ALND groups. This randomized study examined the option of avoiding axillary surgery altogether and demonstrated that in older women with clinically node-negative breast cancer who receive adjuvant Tamoxifen, QL can be improved without compromising disease-free survival or overall survival [60].
The After Mapping of the Axilla Radiotherapy or Surgery (AMAROS) study is an international multicenter trial comparing axillary radiotherapy with axillary surgery in patients with sentinel node–positive early-stage breast cancer [61]. Sentinel node positivity was categorized as macrometastatic (>2 mm), micrometastatic (0.2–2 mm) or ITCs (<0.2 mm). The objective of this study is to prove equivalence of the 2 treatment modalities for locoregional control. The result has not been reported.
The results of the ACOSOG Z0011 study have recently been reported. This is a prospective phase 3 study of patients with sentinel node–positive cancer with clinical T1 or T2 breast cancer randomized to ALND or observation of the axilla after SLND [62]. Sentinel node metastases were detected by frozen section, touch preparation, or H&E staining on permanent section. All patients received breast-conserving surgery and whole breast irradiation. No third field was given to the axillary lymph nodes. A total of 446 patients were randomized into the SLND group and 445 patients into the ALND group. The 2 groups were similar with respect to age, Bloom-Richardson score, estrogen receptor status, use of adjuvant systemic therapy, tumor type, T stage, and tumor size. At 6.3 years follow-up, there was no significant difference between SLND and ALND groups observed with respect to local recurrence (1.6% vs 3.1%) and regional recurrence (0.9% vs 0.5%). The overall survival was 92.5% (SLND) versus 91.8% (ALND) (P = .25), and the disease free survival was 83.9% (SLND) versus 82.2% (ALND) (P = .14). In this study, SLND alone provided excellent locoregional control comparable to SLND with completion ALND in patients with T1 or T2 breast cancers with sentinel node metastases. Adjuvant systemic therapy was given in 96% of patients in the ALND group and 97% of SLND group. In the early breast cancer trialists’ collaborative group overview, greater than 10% difference in the LRR at 5 years resulted in survival difference at 15 years [63]. In the Z0011 study, the total LRR at 5 years was 2.5% in the SLND group and 3.6% in the ALND group. Differences in survival between the 2 groups seem unlikely to emerge. Of note, the Z0011 trial did not include patients undergoing mastectomy without radiation treatment, accelerated partial breast irradiation, or whole breast radiation in the prone position, which would exclude low axillary treatment. Also, patients receiving neoadjuvant therapy were excluded from the study. Further randomized studies are needed to confirm and expand the findings of the Z0011 trial.
References
[33] The American Society of Breast Surgeons. Consensus statement on guidelines for performance of sentinel lymphadenectomy for breast cancer. 2000. Available at: http://www.breastsurgeons.org/statements/PDF_Statements/SLN_Dissection.pdf.
[34] The American Society of Breast Surgeons. Consensus statement on guidelines for performance of sentinel lymphadenectomy for breast cancer. 2005. Available at: http://www.breastsurgeons.org/statements/PDF_Statements/SLN_Dissection.pdf.