W3 Biomechanics and Biology of Plate Fixation of Distal Radius Fractures
Anatomical or near-anatomical restoration, fracture stabilization, “atraumatic” surgery, pain control, and early progressive joint mobilization constitute the basic principles of the operative management of fractures that cannot be satisfactorily reduced or maintained within acceptable parameters by nonoperative methods.1,2 Although perfect anatomical restoration is the ideal, good to excellent functional results may be achieved with near-anatomical reduction, owing to some tolerance of mild deformity.
Loss of length may be linear along the axis of the radius, or may be caused or accentuated by loss of dorsal articular tilt or displacement of the fracture. The distal radius may accommodate 2 to 3 mm of shortening and a loss of 15 to 20 degrees of articular angulation in the frontal and sagittal planes with little functional loss.3–10 Dorsal translation of the lunate in the distal radial fossa with secondary midcarpal collapse owing to loss of dorsal angulation may be an indication for fracture restitution.11 Up to 1 to 2 mm of distal radial articular surface incongruity may not appreciably increase the risk of later post-traumatic arthritis.12,13 Patients with fractures not meeting these criteria may be candidates for open reduction and plate stabilization.
Open reduction and internal plate fixation may be used to achieve fracture restoration and stability throughout the entire healing process without protruding wires or pins and to allow early intensive rehabilitation. These advantages may offset the disadvantages, which include additional operative trauma, fragment devascularization, and some additional risk of wrist stiffness; occasional tendon rupture; and, at times, plate removal. Plates must be matched to the fracture configuration and selected according to the surgeon’s judgment and skills. Bone grafting of defects enhances distal radius fracture stability and healing capacity. We discuss the operative approaches and plate designs that have evolved in an effort to achieve and maintain sufficient biomechanical fracture support, while improving plate biocompatibility with fracture healing.
Approaches
Sharp low-energy incisions are designed to approach the fracture directly in a single plane and to minimize bone fragment devascularization and scar tissue formation. Nevertheless, open reduction, periosteal stripping, and internal fixation convert a closed fracture into a complex open fracture. The opportunity for good fracture reduction and adequate stability to allow otherwise unimpaired fracture healing and early wrist motion may warrant this method of treatment.
Traditionally, dorsally displaced distal radial plates have been approached dorsally, and palmarly displaced fractures have been approached from the palmar side, allowing reliable “buttressing” of the metaphyseal fragments. A plate applied adjacent to the comminuted side and opposite to a side with cortical contact is substantially stronger than the opposite configuration.14 Conversely, the high frequency of postoperative symptoms and complications resulting after dorsal plating has led to the development of smaller “low-profile” plates, “fragment-specific” plates and operative approaches, and plates that may be inserted on the palmar side of the fracture for all fracture configurations.
Dorsal Approach
Dorsal plate application may result in overlying wrist extensor tendon adhesions, irritation, attrition, and occasional extensor tendon rupture; skin irritation from the plate; and wrist stiffness. Nevertheless, some distal radius fracture configurations may be more reliably stabilized and bone graft or substitute applied under direct vision using the dorsal approach. Dorsally applied plates may more reliably prevent redisplacement in some instances of dorsally displaced metaphyseal fragments than palmar plating.
Plate spurs caused by trimming some of the holes of the plate stem or bar may be a substantive source of extensor tendon irritation, attrition, or rupture. Subcutaneous transposition of the extensor pollicis longus to the radial side of the wrist and repair of the third dorsal compartment retinaculum over the plate may limit these complications. Although extensor pollicis longus transposition may restrict the extremes of thumb extension, this is rarely a significant problem. Newer plates have beveled edges, tapered ends, and smooth nonadherent surfaces to prevent soft tissue irritation and adhesions. Despite these precautions and a variety of lower profile design changes, plate removal may be necessary more frequently for dorsally applied plates than for plates positioned on the palmar side.
Palmar Approach
Tendon problems may be more inherent to the dorsal approach than attributable to specific plate characteristics.15,16 There is less space available between bone and tendons on the dorsal side of the radius than on the palmar side. The palmar side of the radius, owing to the increased space available between the bone and the flexor tendons, also may accommodate a thicker and stronger plate to accommodate the increased plate loads generated using this configuration.
Plates inserted on the palmar side of the distal radius may be partially covered by the pronator quadratus, providing additional protection to the extrinsic flexor tendons. Extrinsic flexor tendon attrition or rupture is rare with palmar plating. Proper rotational fracture fragment realignment may be facilitated more easily on the palmar side of the radius, owing to the flat palmar surface of the radius compared with its rounded dorsal side.
Conversely, a palmar incision requires elevation of the pronator quadratus to approach the fracture and placement of a portion of the plate between the pronator quadratus and the bone, diminishing the palmar blood supply of distal radial fragments and impairing their revascularization from this source.17 Occasionally, the distal muscular portion of the flexor pollicis longus must be raised to fit the plate stem on the bone. Although early discomfort on the palmar radial side of the distal forearm and thumb stiffness may result, symptoms are usually transient. Although the “extended flexor carpi radialis approach” preserves the important ulnar circulation to the distal radius, it substantially extends the dissection and compromises the blood supply of a second side of the fracture, the lateral radius.18 Bone grafting dorsal defects from the palmar side of the radius may be more problematic even with the extended approach, owing to difficulty in visualizing the defect.
Biomechanics of Fracture Reduction
Traction, ligamentotaxis, “periosteotaxis,” and manipulation are the mainstays of fracture reduction. The brachioradialis is the only muscle attached to the distal radial fracture fragment. Sarmiento and colleagues19 recognized the resistance and deforming force of the brachioradialis on the distal radial metaphyseal or styloid fragment during the wrist flexion and forearm pronation maneuvers of classically applied closed reduction techniques. The brachioradialis also may remain a deforming force after closed fracture reduction. Sarmiento and colleagues19 reported and advocated fracture reduction, positioning, and cast bracing with the forearm in a supinated position to relax brachioradialis tension during and after fracture reduction.
Orbay and coworkers18 popularized brachioradialis tendon insertion release or lengthening to achieve the same effect, facilitating the biomechanics of open reduction of extra-articular distal radius metaphyseal or intra-articular styloid fragments. The brachioradialis tendon is approached by incising the radial septum, the fascia separating the flexor and extensor compartments of the forearm proximally and containing the insertion of the brachioradialis tendon and the tendons of the first extensor compartment distally over the radial styloid. Brachioradialis release is especially helpful in established fractures and nascent malunions.
The “rule of the majority,” also known as the “vassal rule,” may be helpful in assembling the fracture fragments. This rule states that the major fragments should be realigned, and that the smaller or “vassal” fragments follow the major fragments into position. Replacement of each of the articular fragment components before definitive plate fixation may avoid some of the difficulties that may be encountered in reducing ulnar “die-punch” fragments after radial styloid fixation. Fluoroscopy or arthroscopy or both may be useful in achieving fracture and articular alignment. Kirschner wires may be used for provisional fixation before plate insertion.
Plate Biomechanics
Plate strength is proportionate to the cube of its thickness and inversely proportionate to the cube of its length.20 Screws enhance plate strength and holding power at the plate-bone interface. Wider spacing of screws in the stem increases the bending strength of plate-screw-bone fixation. The torsional strength of plate stem fixation is independent of screw spacing and is proportionate to the number of screws holding the stem.21
Evolution of Distal Radius Plates
Basic Distal Radius T-Plate
In 1973, Mathys designed metallic T-shaped small fragment plates (Synthes, Paoli, PA) that were proportionate to the size of the distal radius (Fig. W3-1).1,2 These plates were among the first generation of modern plates manufactured specifically for distal radius fracture fixation. Distal radius plates support or buttress distal radius fractures. Their stem is affixed to the diaphyseal fragment, and a bar supports and incorporates the metaphyseal fragment or fragments. These plates may be bent and contoured to coapt to the bone.
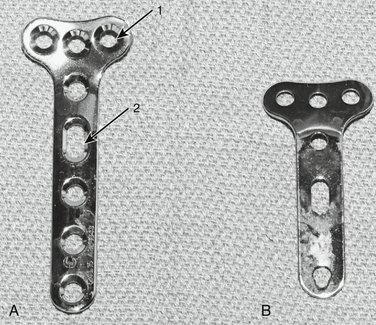
FIGURE W3-1 A, AO/ASIF small fragment distal radius T-plate (long stem). Arrow 1 points to conventional 3.5-mm round plate hole. Arrow 2 points to elliptical 3.5-mm conventional plate stem hole; this hole allows minor plate position adjustments after initial screw insertion. B, Undersurface of conventional distal radius T-plate (short stem).
(Courtesy of Synthes, Paoli, PA.)
Low-Profile, Low-Contact Plates
Plate design has continually evolved toward smaller, “lower profile” implants in an effort to maintain biomechanical fracture stability and improve biocompatibility.22–26 “Relieved” areas of the plate stem, bar, and undersurfaces decrease the amount of plate surface in contact with the bone and facilitate revascularization of the bone segment under the plate.27 The “pi” plate and its T-plate analogue (Synthes, Paoli, PA) were among the early plates of lower profile design (Figs. W3-2 and W3-3). The use of the “pi plate” in distal radial fractures has not shown any appreciable decrease, however, of extensor tendon irritation, attrition, and rupture compared with its predecessors.22
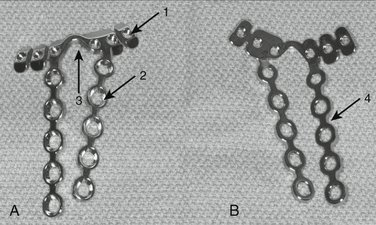
FIGURE W3-2 A, Lower profile dorsal distal radius “pi” plate. Arrow 1 points to round 2.4-mm threaded plate hole for conventional screw or locking peg. Arrow 2 points to round 2.7-mm conventional plate-stem hole. Arrow 3 points to notch to accommodate Lister’s tubercle. B, Undersurface of “pi” plate. Arrow 4 points to lateral area of plate-stem relief.
(Courtesy of Synthes, Paoli, PA.)
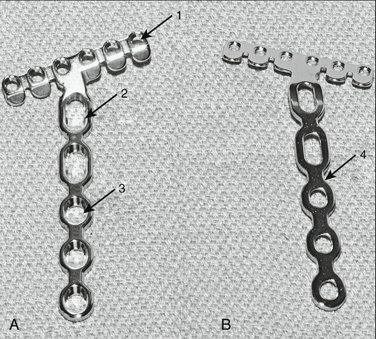
FIGURE W3-3 A, Low-profile T-plate. Arrow 1 points to round 2.4-mm threaded plate hole for conventional screw or locking peg. Arrow 2 points to elliptical 2.7-mm conventional plate-stem hole; this hole allows minor plate position adjustments after initial screw insertion. Arrow 3 points to conventional 2.7-mm round plate-stem hole. B, Undersurface of low-profile distal radius T-plate. Arrow 4 points to lateral area of plate-stem relief.
(Courtesy of Synthes, Paoli, PA.)
Fragment-Specific Fixation
Geissler and Fernandez12 first reported “fragment-specific fixation” in 1991 using a mini-fragment T-plate for palmar “die punch” intra-articular fragments (Fig. W3-4). Leslie and Medoff25 and Barrie and Wolfe26 expanded the concept of “fragment-specific fixation,” introducing “pin plates” (TriMed, Valencia, CA) designed to fit the lateral contour of radial styloid fragments and for volar and dorsal “die-punch” and marginal lip fragments (Fig. W3-5). These smaller plates may sometimes be inserted through smaller incisions, but when more than one plate is used, one or two additional incisions may be required.
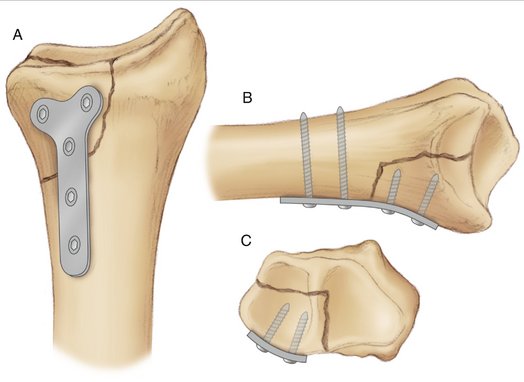
FIGURE W3-4 Fragment-specific fixation of palmar ulnar “die-punch” fragment with 2.7-mm mini-T-plate. A, Palmar view. B, Lateral view. C, Cross-sectional view.
(Courtesy of Synthes, Paoli, PA.)
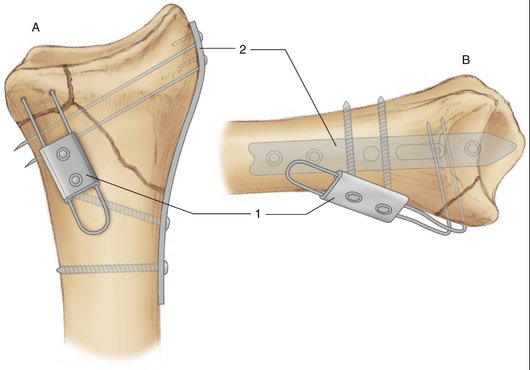
FIGURE W3-5 A and B, Pin plates. 1, Pin plate for marginal lip or “die punch” fragments. 2, Styloid fragment pin plate.
(Courtesy of TriMed, Valencia, CA.)
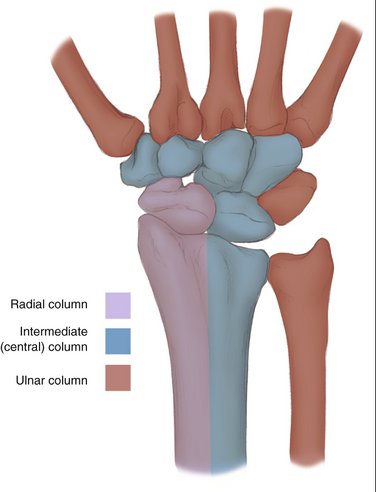
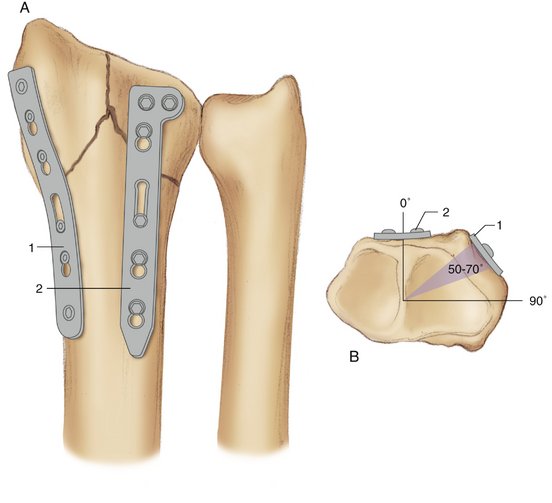
Rikli and Regazzoni and others28–31 have conceptually divided the distal radius into longitudinal, radial, and intermediate columns corresponding to similar carpal columns (Fig. W3-6). The radial and intermediate columns support the areas of high impact and force on the distal radial articular surface generated by the scaphoid and lunate. There also is an ulnar column. Various “fragment-specific,” low-profile plates that individually support the articular fragments of each column are now available in several distal radius plate sets (Fig. W3-7). Two “flexible” low-profile plates, one supporting each column of the fractured distal radius and applied in an orthogonal configuration with the plane of the radial column (radial styloid) plate 50 to 70 degrees in relation to the plane of the intermediate column (dorsal or palmar die-punch fragment) plate, are stronger than a single conventional T-plate or “pi plate,” and individually contain the fragments of both columns (Fig. W3-8).32,33 Orthogonal bicolumnar plating may allow earlier and more intensive rehabilitation, and may have a favorable effect on outcome, but probably does not diminish the operative dissection necessary for plate application.
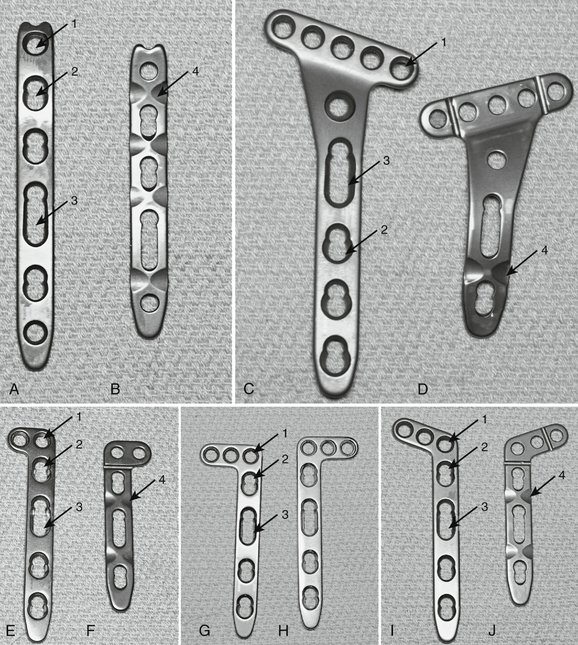
FIGURE W3-7 A to J, Distal radius low-profile locking plates for fragment-specific fixation of the radial styloid (A and B), palmar metaphyseal fragments (C and D), and intra-articular metaphyseal fragments (E-J). Arrow 1 points to threaded round bar-holes for 2.4-mm conventional screws or locking screws or pegs. Arrow 2 points to 2.7-mm “combiholes.” Arrow 3 points to elliptical “combiholes” that allow minor plate position adjustments after initial screw insertion. Arrow 4 points to notched “low-contact” plate undersurfaces.
(Courtesy of Synthes, Paoli, PA.)
“Fixed-Angle Principle”
The “working portion” of a buttress plate is the bar—the distal segment of the plate supporting the metaphyseal fracture fragment or fragments. Support of the metaphyseal fragment and overall plate-bone construct strength may be improved by blades affixed to the plates or screws or pegs locked into the screw or peg holes of the bar by matching threads. Each fixed-angle blade or locking screw or peg provides an additional point of fixation within the plate and increases plate stability.34–37 Fixed-angle blades or locking screws or pegs in the bar of the plate provide additional support for the articular surface of the distal radius against axial loads compared with conventional screws. The “subchondral support” (SCS) plate (Avanta, San Diego, CA) has fixed-angle blades (Fig. W3-9).34 Several plates have a fixed-angle screw or peg option for the bar of the plate (Fig. W3-10). The increased stability of fixed-angle blades or locking screws or pegs may be especially advantageous in osteopenic bone.38,39
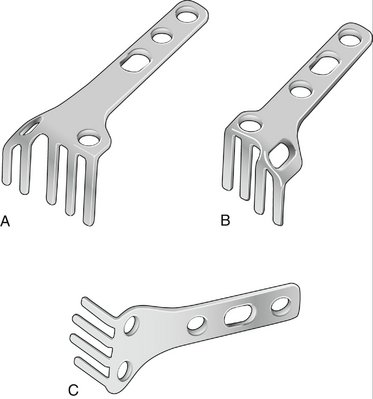
FIGURE W3-9 Subchondral support fixed angle blade plate. A, Large dorsal plate. B, Small dorsal plate. C, Palmar plate.
(Courtesy of Avanta, San Diego, CA.)
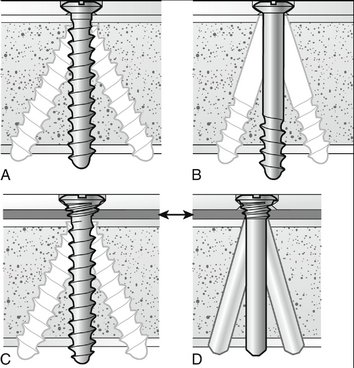
FIGURE W3-10 A, Threaded standard screw. B, Partially threaded standard screw. C, Threaded locking screw. D, Locking peg. Arrows pointing to C and D indicate a space between the locking plate and the bone. Standard holes and flexible bushings in locking holes allow 15 degrees of screw angulation from the perpendicular position.
(Universal Distal Radius System; courtesy of Striker Leibinger Micro Implants, Portage, MI.)
The distal volar plate (DVP) (Hand Innovations, Miami, FL) and similarly designed plates combine fixed-angle locking screws or pegs in the stem of the plate with robust design so that they may be applied to the palmar side of the distal radius for almost all fracture configurations regardless of the direction of instability (Fig. W3-11).15,16,38,40–42 The goal of this plate design is consistently to avoid dorsal plate application and its consequences. Fixed-angle pegs follow the articular contour, are directed to support the articular surface, and help to ensure fixation of commonly found articular fragments. The radialmost pegs are directed into the styloid, and the ulnarmost pegs are directed into the dorsal ulnar edge of the radius to incorporate styloid and dorsal “die-punch” fragments. Failure to incorporate the dorsal “die-punch” fragment may lead to loss of reduction and arthrosis.43 The distal palmar edge of the plate supports palmar die-punch fractures, which also may be incorporated with pegs.
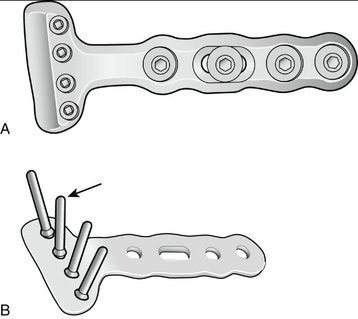
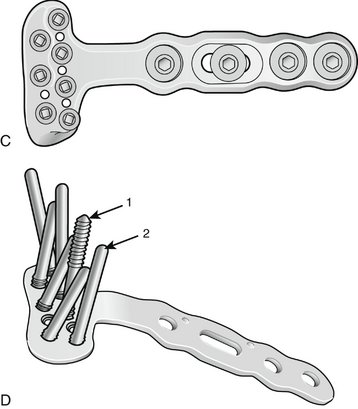
FIGURE W3-11 A, First-generation DVR plate. B, Undersurface first-generation DVR plate with a row of locking pegs (arrow in B) designed to parallel and support the subchondral portion of the articular surface of the distal radius. C, Second-generation DVR plate. D, A proximal row of screws (arrow 1) or pegs (arrow 2) may be inserted to incorporate or support the dorsal lip or fragments of the distal radius.
(Courtesy of Hand Innovations, Miami, FL.)
Locking Plate Stems and Combination Plate Holes (“Combiholes”)
The “fixed-angle principle” also may be applied to the plate stem. Elliptical plate holes (“combiholes”) have been added to the stems of the AO/ASIF distal radius locking plate set (Fig. W3-12) (Synthes, Paoli, PA).35–37 “Combiholes” allow the option of inserting either a fixed-angle locking screw or a conventional screw. Standard screws compress the plate onto the bone and stabilize the fracture owing to friction between the plate and the bone. Locking screws inserted into the stem of the plate provide an additional point of fracture fixation, prevent screw toggle, and increase plate resistance to axial loads compared with conventional screws, owing to locking screw head thread engagement in corresponding threads within the locking plate hole. Distal radius locking plates are precontoured and do not have to be shaped to or rest flush on all parts of the bone and, in essence, may act as an “internal fixator” (i.e., an implanted external fixator) (Fig. W3-13). This feature makes locking plates more biocompatible with the bone. A locking plate might be envisioned as the “ultimate external fixator” with the plate (connecting bar) placed extremely close to the mechanical axis of the bone, maximizing its stability.35–37 Locking plate stems may be especially advantageous in osteopenic bone.
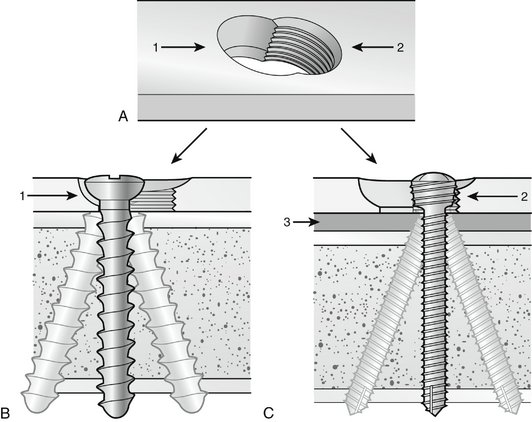
FIGURE W3-12 A to C, “Combihole” (A) allows engagement of a conventional screw (B) or a locking screw (C). Arrow 1, The smooth portion of the “combihole” accommodates a standard screw head. Arrow 2, The threaded portion of the “combihole” accommodates a locking screw head. Arrow 3, Space between the fixed-angle locking plate and the bone surface. Standard screw holes or bushings incorporated in locking plate holes may allow a few degrees of angulation from the vertical position.
(Courtesy of Synthes, Paoli, PA.)
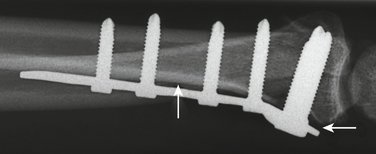
FIGURE W3-13 Small fragment locking T-plate used as an “internal fixator” with a small space between parts of the plate and the bone (arrows).
(Courtesy of Synthes, Paoli, PA.)
The pullout strength of a unicortical screw from bone is about 60% compared with a bicortical screw.37 The surgeon must decide whether to engage one or both cortices. Unicortical drilling may minimize damage to the endosteal circulation of the distal radius and eliminates the need to measure screw length.
Physiology of Fracture Healing
The distal radius receives its diaphyseal intramedullary blood supply on its ulnar surface from the anterior and posterior interosseous arteries through one or more nutrient arteries.18,44 The palmar and dorsal wrist arterial arches supply the periosteum of the cortical surfaces of the distal radial metaphysis directly and through the adjacent joint capsule and ligaments.45 Muscles adjacent to fractures provide blood supply that may enhance fracture healing.17 Muscular blood supply of the distal radius is confined to that from the pronator quadratus.
Enchondral peripheral calcification of fractures escalates at 10 to 21 days after injury and progresses in a centripetal fashion as fracture stability increases.46,47 Plates substitute for external (periosteal) callus, but their application requires devascularization of some of the bone surface resulting in some initial temporary bone necrosis and consequent potential delay in fracture healing, especially in areas where the plate contacts the bone.48,49 This disadvantage is compensated by the immediate stability, pain control, and early and more intensive active exercises provided and allowed by plate fixation. Smaller, newer generation low-contact plates allow more rapid recovery of the bone circulation under the plate than larger or full contact plates.
Fracture callus is typically apparent on x-ray at 4 to 6 weeks after injury or surgery. The fracture is “locked” by the callus at this point, and rehabilitation may be pursued in earnest, including the initiation of progressive strengthening and conditioning exercises. Local clinical signs, including pain, swelling, discoloration, heat, and tenderness, diminish as fracture healing progresses. The plate transforms from “load bearing” at the time of application to “load sharing” as healing progresses, until the completely healed bone bears almost the entire load of stresses.14
Complications
Plates have an internal “memory” for fatigue stresses and may fail (bend or break) as a result of repetitive bending stresses at the fracture site before bone healing. Repetitive bending forces accumulate within the plate over time and may lead to plate breakage if bone healing is delayed.14 Plates should be contoured by bending in only one direction. Bending a plate back eliminates a significant portion of the plate’s fatigue strength. Screw breakage or pullout also may occur from axial or bending forces between the plate and bone surfaces. There is, in essence, a race between bone healing and plate or screw failure. Fractures with defects, comminution, or osteopenia increase the risk of implant failure. As forces between the plate and bone interface increase in strength, intensity, and frequency, conventional screws applied through round and elliptical plate holes are at risk for loosening, toggling, or dislodgment. Bone grafting or bone graft substitutes inserted into major fracture defects and locking screws may relieve plate stresses and enhance fracture healing. Implants are customarily removed only if symptomatic after fracture healing.
There are disadvantages of locking screws.37 The surgeon has no tactile feedback of the quality of screw purchase into the bone. Locking screws stop advancing when their heads are seated into the plate, regardless of bone density. The surgeon is unable to alter the angle of the screw. Polyaxial locking screws with an expandable bushing inside the plate hole (Versalock; Dupuy, Warsaw, IN, and Striker Leibinger Micro Implants, Portage, MI) have been developed and allow some freedom of screw angulation, but testing currently is limited.37 The locking plate cannot be bent or contoured without risk of distorting the plate hole and preventing screw head engagement. The fracture components must be adequately reduced before locking plate and screw or peg insertion. Any malaligned fragment would be held rigidly, which could result in nonunion, malunion, or implant failure. Locking screws may become cold-welded to the plate, rendering removal more difficult. Torque-limiting screwdrivers may minimize this concern.
Discussion
Plate application compounds the closed distal radial fracture and is selected because the surgeon believes that it provides a favorable benefit-to-risk ratio in relation to other choices for the designated fracture. The plate needs to secure the fracture independently only until bone healing occurs, as signaled by the appearance of fracture callus on x-ray and the resolution of local signs and symptoms on clinical examination. Plate strength is only one consideration in plate selection. Fractures with extra-articular comminution or bone loss may require stronger plates and plates with longer stems. Operative trauma should be minimized. Although palmarly applied plates may be less abrasive to surrounding soft tissues than dorsally applied plates, structural stability and ease of application may dictate a dorsal approach. Fixed-angle blades or locking screw or pin options offer additional stability. Locking screws, pins, and plates may be especially advantageous in osteopenic bone.
A plethora of plating systems are available, and a fury of effort has been made to market them with claims and counterclaims that may be largely unsubstantiated by adequate follow-up and reliable statistics.50–54 Conflicts of interest exist and must be taken into consideration.55 Clinicians should look for unconflicted collaborative confirmation from sources independent of the manufacturers and innovators. Evidence-based medicine is important and, in the absence of clearly defined valid choices, there may be no substitute for common sense.56 Previous expectations have not always been fulfilled, even when based on sound theory.22
Implants may come and go, but fracture management principles remain constant.1,2 Plates should be selected to correspond with fracture configuration as closely as possible. Numerous plates and plating systems satisfy these criteria. In our view, there is no single plate that matches up with all myriad fracture patterns. There may be more than one “right” surgical approach or combination of approaches and more than one “right” plate or aggregate of plates to treat each fracture. The judgment of the surgeon remains paramount in plate and surgical approach selection.
There are some practical considerations. Most of us are restricted in how many plate systems our hospitals will buy for us. Plate cost is a consideration in plate and plating system selection, especially in comparable situations. It may be helpful to have as many plate designs available as possible. Use by consignment for each patient may be accommodating.
ACKNOWLEDGMENTS
The authors acknowledge the advice and assistance of David Little, I.V. Hall, Michael Schenk, Bill Buhner, Kyle Cunningham, Clint Clardy, Bill Dixon, Patrick Harmon, and Alvra Jenkins in the preparation of this manuscript.
1. Muller M, Allgower M, Schneider R, et al. Manual of Internal Fixation. New York, 3rd ed; 1991; Springer: Verlag.
2. Heim U, Pfeiffer KM. Internal Fixation of Small Fractures. New York, 3rd ed; 1988; Springer: Verlag.
3. Lidstrom A. Fractures of the distal end of the radius: a clinical and statistical study of end results. Acta Orthop Scand. 1959;41(Suppl):1-25.
4. Villar RN, Marsh D, Rushton N, et al. Three years after Colles’ fracture: a prospective review. J Bone Joint Surg Br. 1987;69:635-638.
5. Short WH, Palmer AK, Werner FW, et al. A biomechanical study of distal radius fractures. J Hand Surg. 1987;12:529-534.
6. McQueen M, Caspers J. Colles’ fracture: does the anatomical result affect the final function? J Bone Joint Surg Br. 1988;70:649-651.
7. Bradway JK, Amadio PC, Cooney WPIII. Open reduction and internal fixation of displaced, comminuted intraarticular fractures of the distal end of the radius. J Bone Joint Surg Am. 1989;71:839-847.
8. Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20:208-210.
9. Aro HT, Koivunen T. Minor axial shortening of the radius affects outcome of Colles’ fracture treatment. J Hand Surg [Am]. 1991;16:392-398.
10. Fitoussi F, Ip WY, Chow SP. Treatment of displaced intraarticular fractures of the distal end of the radius with plates. J Bone Joint Surg Am. 1997;79:1303-1312.
11. Taleisnik J, Watson HK. Midcarpal instability caused by malunited fractures of the distal radius. J Hand Surg [Am]. 1984;9:350-357.
12. Geissler WB, Fernandez DL. Percutaneous and limited open reduction of the articular surface of the distal radius. J Orthop Trauma. 1991;5:255-264.
13. Knirk JL, Jupiter JB. Intraarticular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647-659.
14. Disegi JA, Wyss H. Implant materials for fracture fixation: a clinical perspective. Orthopedics. 1989;12:75-79.
15. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg [Am]. 2002;27:205-215.
16. Orbay JL, Fernandez DL. Volar fixed angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg [Am]. 2004;29:96-102.
17. Stein H, Perren SM, Cordey J, et al. The muscle bed—a crucial factor for fracture healing: a physiological concept. Orthopedics. 2002;25:1379-1383.
18. Orbay JL, Infante A, Khouri RK, et al. The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Upper Extrem Surg. 2001;5:204-211.
19. Sarmiento A, Pratt GW, Berry NC, et al. Colles’ fractures: functional bracing in supination. J Bone Joint Surg Am. 1975;57:311-317.
20. Cochran GVB. A Primer of Orthopedic Biomechanics. New York: Churchill Livingstone; 1982.
21. Tornkvist H, Hearn TC, Schatzker J. The strength of plate fixation in relation to the number and spacing of bone screws. J Orthop Trauma. 1996;10:204-208.
22. Ring D, Jupiter J, Brennwald J, et al. Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg [Am]. 1997;22:777-784.
23. Simic PM, Weiland AJ. Fractures of the distal radius: changes in treatment over the past two decades. J Bone Joint Surg Am. 2003;85:552-564.
24. Carter PR, Frederick HA, Laseter GF. Open reduction and internal fixation of unstable distal radial fractures with a low profile plate: a multicenter study of 73 fractures. J Hand Surg [Am]. 1998;23:300-307.
25. Leslie BM, Medoff RJ. Fragment specific fixation of distal radius fractures. Tech Orthop. 2000;15:336-352.
26. Barrie KA, Wolfe SW. Internal fixation for intraarticular distal radial fractures. Tech Hand Upper Extrem Surg. 2002;6:10-20.
27. Perren SM, Klaue K, Pohler O, et al. The limited contact dynamic compression plate (LC-DCP). Arch Orthop Trauma Surg. 1990;109:304-310.
28. Rikli D, Regazzoni P. Fractures of the distal end of the radius treated by internal fixation and early function: a preliminary report of 20 cases. J Bone Joint Surg Br. 1996;78:588-592.
29. Rikli D, Regazzoni P. The double plating technique for distal radius fractures. Tech Hand Upper Extrem Surg. 2000;4:107-114.
30. Taleisnik J. Post-traumatic carpal instability. Clin Orthop. 1980;149:73-82.
31. Taleisnik J. Wrist anatomy, function, and injury. Instr Course Lect. 1978;27:61-87.
32. Jakob M, Rikli DA, Regazzoni P. Fractures of the distal radius treated by internal fixation and early function: a prospective study of 73 consecutive patients. J Bone Joint Surg Br. 2000;82:340-344.
33. Peine R, Rikli DA, Hoffmann R, et al. Comparison of three different plating techniques for the dorsum of the distal radius: a biomechanical study. J Hand Surg [Am]. 2000;25:29-33.
34. Gesensway D, Putnam MD, Mente PL, et al. Design and biomechanics of a plate for the distal radius. J Hand Surg [Am]. 1995;20:1021-1027.
35. Perren SM. Evolution of the internal fixation of long bone fractures: the scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093-1110.
36. Frigg R. Development of the locking compression plate. Injury. 2003;34(Suppl 2):B6-B10.
37. Haidukewych GJ. Innovations in locking plate technology. J Am Acad Orthop Surg. 2004;12:205-221.
38. Orbay JL, Fernandez DL. Volar fixed angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg. 2004;29:96-102.
39. Kiyoshige Y. Condylar stabilizing technique with AO/ASIF distal radius plate for Colles fracture associated with osteoporosis. Tech Hand Upper Extrem Surg. 2002;6:205-208.
40. Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000;5:103-112.
41. Osada D, Viegas SF, Shah MA, et al. Comparison of distal radial dorsal and volar fracture fixation plates: a biomechanical study. J Hand Surg [Am]. 2003;28:94-104.
42. Osada D, Fujita S, Tamai K, et al. Biomechanics in uniaxial compression of three distal radius volar plates. J Hand Surg [Am]. 2004;29:446-451.
43. Harness N, Ring D, Volar Jupiter JB:. Barton’s fractures with concomitant dorsal fracture in older patients. J Hand Surg [Am]. 2004;29:439-445.
44. Nagel A. The clinical significance of the nutrient artery. Orthop Rev. 1993;22:557-661.
45. Sheetz KK, Bishop AT, Berger RA. The arterial blood supply of the distal radius and ulna and its potential use in vascularized pedicled bone grafts. J Hand Surg [Am]. 1995;20:902-914.
46. Einhorn TA, Hirschman A, Kaplan C, et al. Neutral protein-degrading enzymes in experimental fracture callus: a preliminary study. J Orthop Res. 1989;7:792-805.
47. Buckwalter JA, Einhorn TA, Bolander ME, et al. Healing of musculoskeletal tissues. In: Rockwood CAJr, Green DP, Bucholz RW, editors. Fractures in Adults. Philadelphia: Lippincott-Raven, 1996.
48. Perren SM, Cordey J, Rahn BA, et al. Early temporary porosis of bone induced by internal fixation implants: a reaction to necrosis, not to stress protection? Clin Orthop. 1988;232:139-151.
49. Cordey J, Perren SM, Steinemann SG. Stress protection due to plates: myth or reality? A parametric analysis made using the composite beam theory. Injury. 2000;31(Suppl 3):C1-C13.
50. Freedman KB, Back S, Bernstein J. Sample size and statistical power of randomized, controlled trials in orthopaedics. J Bone Joint Surg Br. 2001;83:397-402.
51. Lochner HV, Bhandari M, Tornetta PIII. Type-II error rates (beta errors) of randomized trials in orthopaedic trauma. J Bone Joint Surg Am. 2001;83:1650-1659.
52. Bhandari M, Morrow F, Kulkarni AV, et al. Meta-analyses in orthopaedic surgery: a systematic review of their methodologies. J Bone Joint Surg Am. 2001;83:15-24.
53. Bhattacharyya T, Tornetta PIII, Healy WL, et al. The validity of claims made in orthopaedic print advertisements. J Bone Joint Surg Am. 2001;85:1224-1228.
54. Gummesson C, Atroshi I, Ekdahl C. The quality of reporting and outcome measures in randomized clinical trials related to upper extremity disorders. J Hand Surg [Am]. 2004;29:727-734.
55. Zuckerman JD, Prasarn M, Kubiak EN, et al. Conflict of interest in orthopaedic research. J Bone Joint Surg Am. 2004;86:423-437.
56. Bernstein J. Evidence-based medicine. J Am Acad Orthop Surg. 2004;12:80-88.