Applied anatomy of the temporomandibular joint
The temporomandibular joint (TMJ) is sited at the base of the skull and formed by parts of the mandible and the temporal bone, separated by an intra-articular meniscus. It is a synovial joint capable of both hinge (rotation) and sliding (translatory) movements. Like other synovial joints, it may be affected by internal derangement, inflammatory arthritis, arthrosis, and muscular disorders.
Bones
The mandible has a horizontal part (the body) and a vertical part (the ramus). They meet at the mandibular angle. The cranial end of the ramus has two processes: anteriorly the coronoid process and posteriorly the condylar process, which has a head on top and a distinct neck below. The squamous portion of the temporal bone contains the articular surface with a concave articular fossa posteriorly and a convex articular tubercle anteriorly. The articular surface is about three times as large as that of the mandibular head and is covered with fibrocartilage which continues anteriorly into the articular tubercle, the posterior aspect of which is the most important part of the joint. From the temporal bone develops a zygomatic process which, together with the temporal process of the zygomatic bone, forms the zygomatic arch (Fig. 1).
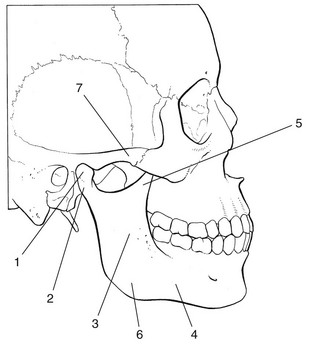
Fig 1 Osseous structures of the temporomandibular joint: 1, mandibular head (condylar process); 2, neck of mandible; 3, ramus; 4, body; 5, coronoid process; 6, mandibular angle; 7, zygomatic arch.
The midline fusion of the left and right mandibular bodies provides a connection between the two temporomandibular joints, so that movement in one joint always influences the opposite one.
Joint capsule and ligaments
The joint capsule is wide and loose on the upper aspect around the mandibular fossa. Distally, it diminishes in a funnel shaped manner to become attached to the mandibular neck (Fig. 2). Its laxity prevents rupture even after dislocation.
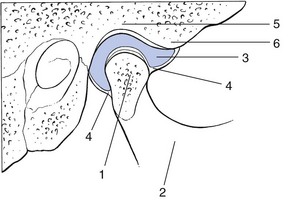
Fig 2 The joint capsule and the intra-articular meniscus: 1, condylar process; 2, mandible; 3 meniscus; 4, joint capsule; 5, articular fossa; 6, articular tubercle.
Laterally and medially, a local reinforcement of the joint capsule is found. The lateral collateral ligament courses from the zygomatic arch obliquely downwards and backwards towards the posterior rim of the mandibular neck, lateral to the outer aspect of the capsule. At its posterior aspect, it is in close relation to the joint capsule and prevents the joint from opening widely. Medially, the joint capsule is locally reinforced by the medial collateral ligament. There are also two extracapsular ligaments: the sphenomandibular (between the spine of the sphenoid bone and the lingula of the mandible) and the stylomandibular (from the styloid process of the temporal bone to the mandibular angle).
Intra-articular meniscus
The intra-articular meniscus, or disc (see Fig. 2), is attached along its entire circumference to the capsule. It compensates for the discongruent articular bony surfaces and contributes to the stability of the joint. The meniscus divides the joint into an upper and a lower compartment, each fully separated from the other (see Hodges, 1990, in bibliography). The upper compartment is a sliding joint, the lower a hinge. Because the meniscus is malleable, it fills the whole joint space in any position of the condyle. Its anterior aspect is connected to the lateral pterygoid muscle. Posteriorly, the condyle is attached to the meniscus by loose connective tissue – the bilaminar zone – which is also fused to the posterior capsule. The superior surface of the meniscus relates to the middle third of the articular tubercle, the inferior surface to the anterior portion of the condyle. The meniscus always follows the movement of the condyle: when the mandibular head glides anteriorly on opening the mouth, the meniscus moves anteriorly; when it moves back on closing, so does the meniscus.
Nociceptive innervation
The articular cartilage, the synovial tissues and the central portion of the disc do not contain any pain receptors and therefore cannot give rise to pain. All other capsular and intra-articular structures do possess nociceptors; the meniscus has them mainly at the posterior edge, less on its anterior portion. They are chiefly activated by high mechanical stresses and by acute or chronic inflammation.
Muscles and tendons
The most important contractile structures are the masseter, temporal and pterygoid muscles (Fig. 3).
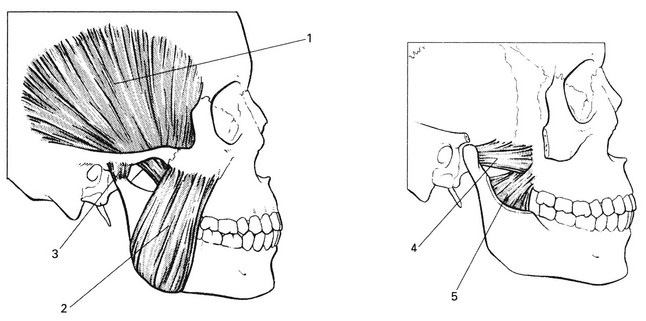
Fig 3 Muscles of the temporomandibular joint: 1, temporalis; 2, masseter; 3, joint capsule; 4, lateral pterygoid; 5, medial pterygoid.
The masseter muscle originates at the lower edge (superficial part) and deep aspect of the zygomatic arch and at the temporal fascia (deep part). Both parts course superficially from the mandibular ramus towards the angle, where they have broad insertions into the tuberosity. Contraction of the masseter closes the mouth.
The origin of the temporalis muscle is in the temporal fossa and at the temporal fascia. It stays deep to the zygomatic arch and inserts into the coronoid process of the mandible. It also closes the mouth.
The medial pterygoid originates in the pterygoid fossa at the base of skull and inserts into the deep aspect of the mandibular angle at the pterygoid tuberosity. It acts synergistically with the masseter and temporalis muscles.
The lateral pterygoid muscle lies on the deep aspect of the mandibular neck. It has two heads: one originating at the major wing of the sphenoid bone, the other at the lateral aspect of the pterygoid process. The two heads course laterally and posteriorly, join each other and insert into the pterygoid fovea of the mandibular condyle, the joint capsule and the meniscus. Because the muscle courses in an anteromedial to posterolateral direction, bilateral simultaneous action of both lateral pterygoids pulls the mandibular condyles anteriorly; which opens the mouth. Unilateral contraction provokes a contralateral deviation of the chin. The medial and lateral pterygoid muscles are too deep to be palpated.
The suprahyoid muscles – digastric and stylohyoid – and the muscles of the floor of the mouth – mylohyoid and geniohyoid – only take part in opening of the mouth when the effect of gravity is excluded, for example lying down. They are of little clinical importance.
Biomechanical aspects
The mandible allows three types of movement.
Forward movement of the mandible
The lateral pterygoid muscle pulls the mandible forwards (anterior translatory movement). During this process the mandible moves slightly downwards because the condyle is pressed down on the articular tubercle. The mandible is pulled backwards on closing by the posterior fibres of the temporalis muscle.
Opening and closing the mouth
Because the TMJ contains a meniscus, two independent movements are possible: a rotation or hinge movement and a translatory glide. From the onset of opening to the midpoint, the mandibular head rotates on the undersurface of the intra-articular meniscus because of the effect of gravity and the action of the muscles of the floor of the mouth. At the same time, the collateral ligaments are taut. On further movement, condyle and meniscus glide together anteriorly and slightly caudally on the articular tubercle because of contraction of the lateral pterygoid. No further rotation occurs once the anterior translatory movement has begun. If for some reason the anterior movement of the mandibular head on opening is not possible on one side, the chin deviates to the ipsilateral side.
The mouth is closed by contraction of the temporalis, masseter and medial pterygoid muscles.
Grinding movements
The mandible rotates around a vertical axis through the contralateral mandibular head by a unilateral contraction of the lateral pterygoid muscle. This is followed by a contraction of the posterior fibres of the temporal muscle, which repositions the head of the condyle. When this occurs on alternate sides a typical grinding movement results. If at the same time the other masticatory muscles contract, food can be crushed.
Nerves and blood vessels
Between the tragus and the mandibular condyle lie the superficial temporal artery and veins. The superficial temporal artery is the continuation of the external carotid artery and the veins course towards the internal jugular vein. Deep to the neck of the mandible passes the maxillary artery, a branch of the external carotid.
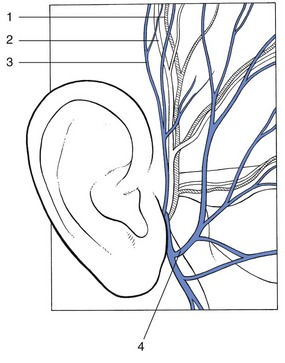
The auriculotemporal nerve, a branch of the mandibular nerve, which again originates from the trigeminal nerve (V), is just posterior to the blood vessels, which it follows cranially. The upper branch of the facial nerve (VII) passes superficially to the blood vessels at the level of the mandibular neck and runs horizontally forwards before breaking up into several terminal branches (Fig. 4).
Fautrez, J. Leiddraad bij de Studie van de Stelselmatige Ontleedkunde van de mens; vol I. Uitgevers Desoer, Luik, 1967.
Gerritsen, B, Heerkens, Y. Anatomie in vivo van het Bewegingsapparaat. Utrecht: Bunge; 1986.
Hodges, JM, Managing temporomandibular joint syndrome. Laryngoscope 1990; 100:60–66. ![]()
McMinn, R, Hutchings, R. Atlas of Human Anatomy, 2nd ed. London: Wolfe; 1993.
Sobotta, J, Becher, H. Atlas der Anatomie des Menschen; vols 1 and 3. Urban & Schwarzenberg, Munich, 1967.