Applied anatomy of the knee
Articular surfaces
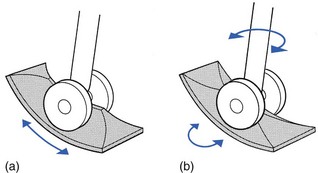
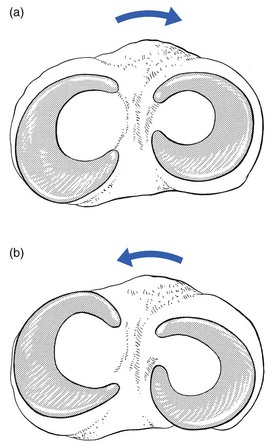
The distal femur can be compared with a double wheel, in which the medial and lateral condyles are the components and the intercondylar notch the junction between them (Fig. 1). The condyles are convex in both planes. The medial condyle extends a little more distally than the lateral. The greater prominence of the lateral femoral condyle prevents the patella from sliding laterally.
The anteroposterior elevation between the tibial condyles corresponds to the femoral intercondylar notch. If the surfaces of the tibial condyles are projected anteriorly, they coincide with the articular surface of the patella which corresponds to, and is almost congruent with, the anterior surfaces of the femoral condyles. If the intercondylar eminence of the tibia is projected anteriorly, its plane is continuous with the vertical ridge on the patella just as the intercondylar notch of the femur continues in the central groove of the patellar surface of the femur. This arrangement resembles a twin-wheel rolling on a central rail (Fig. 1a). During flexion and extension, tibia and patella act as one structure in relation to the femur.1
The rounded surfaces of the femoral condyles in relation to the flatter tibial ones might suggest that the former roll during flexion–extension. In fact this is not so. As long ago as 1836 the Weber brothers demonstrated that the femoral condyles roll and slide almost simultaneously, and that these movements are in opposite directions. During flexion, the femoral condyles roll backwards and slide forwards on the tibia, whereas during extension they roll forwards and slide backwards (see Standring, Fig. 82.20). The ratio of rolling to sliding differs with the degree of flexion or extension, which means that during the first 30° of flexion the movement is almost entirely rolling, whereas at nearly full flexion the condyles slip over the tibial plateau without rolling.2
The knee joint is thus primarily a hinge, with the wheel-shaped surfaces of the femoral condyles gliding and rolling in a twin set of concave curved gutters: the tibial and patellar surfaces. However, while this is a satisfactory concept in terms of flexion and extension, in reality the situation is more complex because the knee allows not only gliding and rotation around a horizontal axis but also rotation through a vertical axis, i.e. internal and external rotation of the tibia in relation to the femur. Were the knee to be only as so far described – a hinge joint with a long tibial intercondylar eminence gliding between the two femoral condyles – rotation would be precluded. However, if the anterior and posterior ends are flattened, rotation becomes possible (Fig. 1b). The remaining middle part of the eminence, forming the ‘intercondylar spines’, is then the central pivot about which the movements of axial rotation occur.
The patella
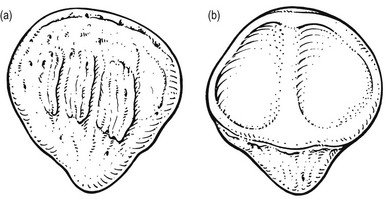
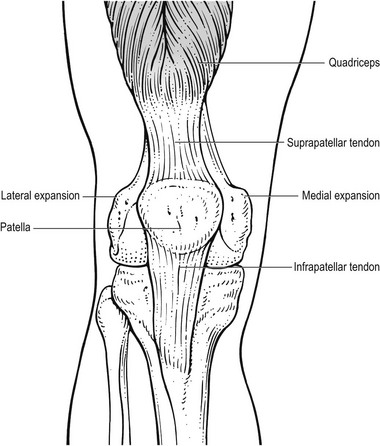
The patella is a flat, triangular bone, situated on the front of the knee joint (Fig. 2). It is usually regarded as a sesamoid bone, developed in the quadriceps femoris tendon. Its convex anterior surface is covered by an expansion from the tendon of the quadriceps femoris which is continuous below with the superficial fibres of the ligamentum patellae. It is separated from the skin by a bursa (prepatellar bursa).
The apex is pointed and gives attachment to the ligamentum patellae.
The menisci
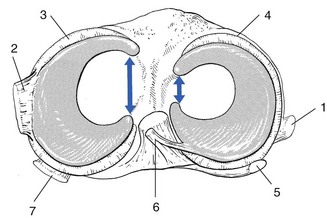
There are two menisci in the space between the femoral and tibial condyles. They are crescent-shaped lamellae, each with an anterior and a posterior horn, and are triangular in cross section. The superior and inferior surfaces are in contact with the femoral and tibial condyles, respectively, and the peripheral surfaces are adherent to the synovial membrane of the capsule. The anterior and posterior horns are anchored to the tibial condyle in the anterior and posterior intercondylar fossae, respectively. The horns of the medial meniscus are further apart than those of the lateral, which makes the former nearly semilunar and the latter almost circular. The menisci correct the lack of congruence between the articular surfaces of tibia and femur, increase the area of contact and improve weight distribution and shock absorption.3–6 They also help to guide and coordinate knee motion, making them very important stabilizers of the knee.
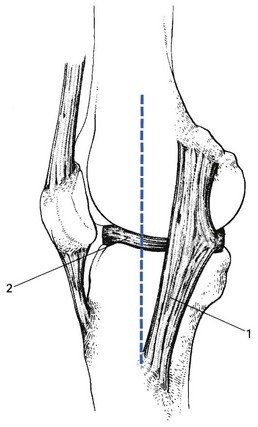
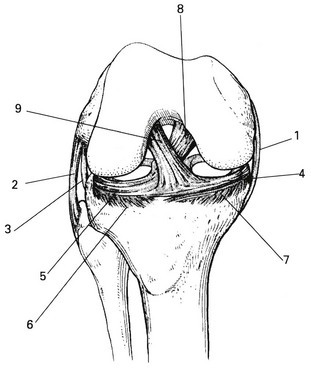
Movement between the tibial surface and the menisci is limited by the coronary ligaments connecting the outer meniscal borders with the tibial edge (Fig. 3, see Standring, Fig. 82.9). The coronary ligaments of the medial meniscus are shorter (4–55 mm) and stronger than those of the lateral meniscus (13–20 mm).7 The medial collateral ligament of the knee is attached by its deep fibres to the outer border of the medial meniscus. In contrast, there is no connection between the lateral meniscus and the corresponding collateral ligament (Fig. 4). These anatomical differences between the medial and the lateral meniscus may explain the lesser mobility and the greater vulnerability of the former (see Fig. 3).8
Menisci do not contain pain-sensitive structures and are consequently insensitive to trauma. Their outer third has some blood supply and therefore a slight ability to heal. The inner non-vascularized part receives nutrition through diffusion of synovial fluid.9,10
Movements of the menisci
During flexion of the knee, the body of the meniscus moves posteriorly and during extension it moves anteriorly. In lateral (axial) rotation, the menisci will follow exactly the displacement of the femoral condyles, which means that the lateral meniscus will be pushed forwards on the tibia and the medial meniscus will be pulled backwards (Fig. 5a). On the medial aspect the anterior part of the medial coronary ligament then comes under tension. The same effect occurs in the medial rotation: the medial meniscus is pressed forwards and the lateral meniscus drawn backwards (Fig. 5b), which causes tension in the anterior part of the lateral coronary ligament.
Joint capsule and ligaments
Capsule
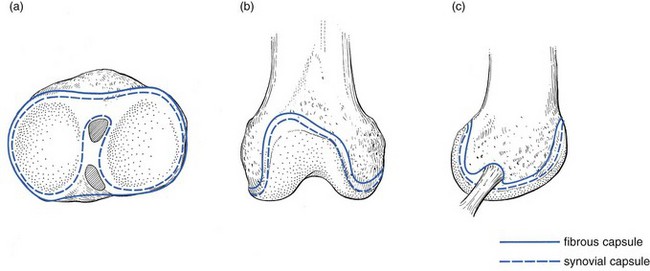
The tibial attachment of the capsule (Fig. 6a) is attached to the borders of the articular surfaces of the tibia and therefore follows its anterior, medial and lateral edges. At the posterior border the synovial membrane follows the edges of the medial and lateral condyles, to form a loop around the insertion of the anterior cruciate ligament. At the anterior border the synovial membrane is projected backwards by a sizeable pad of adipose tissue – the infrapatellar pad.
• Anteriorly the capsule is attached proximal to the edge of the articular surface, thus forming the suprapatellar pouch (Fig. 6b).
• On the lateral condyle the attachment of the fibrous capsule lies above the insertion of the popliteus tendon, which makes the latter lie intra-articularly, covered only by the synovial membrane (Fig. 6c).
• Posteriorly and following the articular surfaces of the femoral condyles, the attachment of the synovial membrane dives into the intercondylar notch to form a loop around the femoral insertions of the cruciate ligaments. The cruciate ligaments are thus kept outside the capsule by an invagination of the synovial membrane, which forms a partition in the sagittal plane of the joint space.
At the patella, the capsule follows the margins of the bone.
Ligaments
The medial ligamentous complex
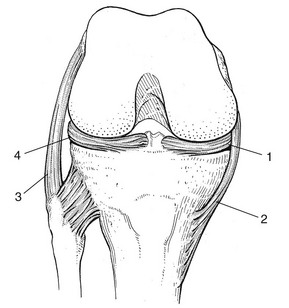
The medial ligamentous complex has two layers: the deeply situated capsular reinforcements with an anterior, medial and posterior part, and the strong and more superficially localized medial collateral ligament (MCL). The MCL is the primary stabilizer of the medial side of the knee. It is a broad, flat and almost triangular band with a large femoral attachment on the posterosuperior aspect of the epicondyle. Its fibres run obliquely anteriorly and inferiorly to insert at the medial aspect of the tibia, just behind and slightly under the insertions of the semitendinosus muscle (see Gosling et al, Fig. 6.79). The anterior fibres of the ligament are separated from those of the deep capsular reinforcements and therefore the anterior border of the ligament can be palpated easily. The posterior fibres, however, blend intimately with the capsule and with the medial border of the medial meniscus (Fig. 7).11
The strong MCL stabilizes the knee against excessive valgus forces and external rotation. Although it slackens during flexion, the posterior fibres attached to the meniscus remain taut, an observation that is important in the consideration of chronic ligamentous adhesions of the MCL (see p. 700).
The lateral collateral ligament
The lateral collateral ligament (LCL) is part of the so-called lateral quadruple complex (biceps tendon, iliotibial tract, popliteus and LCL), responsible for the lateral stability of the knee. It is round in cross-section and runs from the lateral epicondyle of the femur to the head of the fibula, deep to the insertion of the biceps. The ligament lies completely free, separated from the capsule and the lateral meniscus by the popliteus tendon (see Figs 3, 10, see Gosling et al, Fig. 6.78). It stabilizes the knee against excessive varus movement. A small bursa lies between the popliteus tendon and the LCL.
The cruciate ligaments
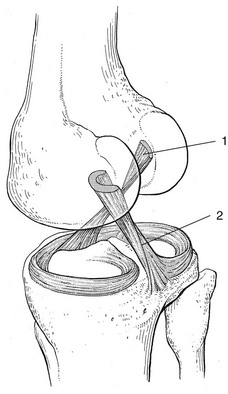
Although the cruciate ligaments lie in the centre of the joint (Fig. 8), they remain extrasynovial because of the posterior invagination of the synovial membrane. They ensure the anteroposterior stability of the knee and, together with the collateral ligaments, prevent rotational movements during extension.
The posterior cruciate ligament
The tibial attachment of the posterior cruciate ligament is at the posterior intercondylar area, but fans out at the posterior border of the tibial plateau. The ligament runs in a medial and anterior direction and crosses the anterior cruciate ligament from medial and from behind to insert at the lateral surface of the medial condyle, deeply in the intercondylar fossa. Like the anterior cruciate, the posterior cruciate ligament has a complex architecture but is twice as strong. It is a basic knee stabilizer, tightest in mid-position. During extension, the posterior cruciate ligament pulls on the femur, causing backwards sliding during its anterior rolling. The posterior cruciate ligament also prevents anterior gliding of the femur during squatting, resists hyperextension and has an important role in the medial stability of the knee.12
Muscles and tendons
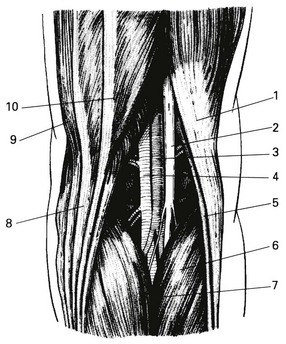
The extensor mechanism (Fig. 10)
The biarticular nature of the rectus femoris and the fact that it runs anterior to the flexion–extension axis of the hip gives it the specific function of a hip flexor (see online chapter Applied anatomy of the hip and buttock).
Flexors of the knee
• The gastrocnemii, although strong plantiflexors and invertors of the heel, are only weak flexors of the knee (see Standring, Fig. 82.3). They also help in active stabilization of the joint. The medial head is a weak internal and the lateral head a weak external rotator.
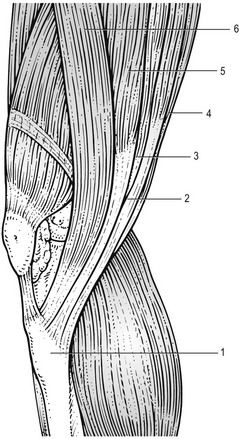
• The semitendinosus, gracilis and sartorius insert under and in front of the medial condyle of the tibia in the so-called ‘pes anserinus’, just medial to the tibial tuberosity and anterior to the tibial insertion of the MCL. They are flexors and internal rotators of the knee (Fig. 11).
• The semimembranosus inserts at the medial condyle of the tibia but has some fascicles attaching to the oblique popliteal ligament and a few fibres attaching to the posterior edge of the medial meniscus. It is a flexor and an internal rotator.
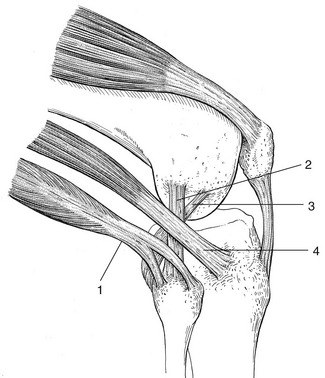
• The popliteus muscle originates within the joint at the lateral epicondyle of the femur (Fig. 12, see Standring, Fig. 83.11, see Gosling et al, Fig. 6.77). Other origins are situated at the dorsal aspect of the capsule and the lateral meniscus. The muscle belly lies deeply in the popliteal fossa under the lateral gastrocnemius and the plantaris. The broad insertion is at the upper and posterior aspect of the tibia. The popliteus is a flexor and an internal rotator of the knee. It also spans the posterior capsule of the knee and pulls the lateral meniscus in a posterior direction during flexion. Another important function of the muscle is to prevent the femur from slipping forwards on the tibia during squatting. This active function of the popliteus is very similar to the static role of the posterior cruciate ligament.
• The biceps femoris or lateral hamstring inserts at the top and posterior aspect of the fibular head in front of and behind the insertion of the lateral collateral ligament (see Fig. 12). Some fibres also attach to the posterolateral aspect of the tibia and the lateral part of the joint capsule. It is a strong flexor and external rotator of the knee.
Innervation of the muscles
Table 1
| Peripheral nerve | Spinal innervation | |
| Extension | ||
| Quadriceps | Femoral | L2, L3, L4 |
| Flexion | ||
| Semitendinosus | Tibial | L5, S1, S2 |
| Semimembranosus | Tibial | L5, S1, S2 |
| Gracilis | Obturator | L2, L3, L4 |
| Sartorius | Femoral | L2. L3 |
| Popliteus | Tibial | L4, L5, S1 |
| Biceps femoris | Sciatic | L5, S1 |
| Tensor fasciae latae | Superior gluteal | L4, L5 |
| Gastrocnemius | Tibial | S1, S2 |
Nerve structures and blood vessels: the popliteal fossa
The lozenge-shaped popliteal fossa is an anatomical space of particular importance because it contains the vessels and nerves of the lower limb (Fig. 13, see Standring, Fig. 82.2). Its lower borders are formed by the heads of the gastrocnemius. The upper lateral border is the biceps femoris and the upper medial border the semitendinosus and semimembranosus muscles. Its floor is the posterior capsule and the popliteus muscle. The popliteal fossa is bounded posteriorly by the deep popliteal fascia.
References
1. Kapandji, IA. The Physiology of the Joints, vol 2: Lower Limb, 5th ed. Churchill Edinburgh: Livingstone; 1987.
2. Pope, MH, Crowninshield, R, Miller, R, Johnson, R, The static and dynamic behavior of the human knee in vivo. J Biomech 1976; 9:449–452. ![]()
3. Seedhom, BB, Dowson, D, Wright, V, Functions of the menisci – a preliminary study. J Bone Joint Surg 1974; 56B:381. ![]()
4. Seedholm, BB, Hargraves, DJ. Transmission of load in the knee joint with special reference to the role of the menisci. Part II: experimental results, discussion and conclusions. Eng Med. 1979; 8:220.
5. Shrive, NG, O’Connor, JJ, Goodfellow, JW, Load bearing in the knee joint. Clin Orthop 1978; 131:129. ![]()
6. Walker, PS, Erkman, MJ, The role of the menisci in force transmission across the knee. Clin Orthop 1975; 109:184. ![]()
7. Seedhom, BB, Dowson, D, Wright, V. The load-bearing function of the menisci: a preliminary study. In: Ingwersen OS, Van Linge B, Van Rens TJG, Rosingh GE, Veraart B, Le Vau D, eds. The Knee Joint. Excerpta Medica and American Elsevier; 1974:37–42.
8. McDermott, LJ. Development of the human knee joint. Arch Surg. 1943; 46:705–719.
9. Arnoczky, SP, Warren, RF, The micro-vasculature of the meniscus and its response to injury. Am J Sports Med 1983; 11:131. ![]()
10. Danzig, L, Resnick, D, Gonsalves, M, Akeson, WH, Blood supply to the normal and abnormal menisci of the human knee. Clin Orthop 1983; 172:271. ![]()
11. McMinn, RMH, Hutchings, RT. A Colour Atlas of Human Anatomy. London: Wolfe; 1977.
12. Girgis, FG, Marshall, JL, Monajem, ARS, The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop 1975; 106:216–231. ![]()
13. Gollehon, DL, Torzill, PA, Warren, RF, The role of the posterolateral and cruciate ligaments in the stability of the human knee. A biomechanical study. J Bone Joint Surg 1987; 69A:233–242. ![]()
14. Williams, P, Warwick, R. Gray’s Anatomy. London: Churchill Livingstone; 1980.
15. Sobotta, J, Becher, H. Atlas of Human Anatomy. Munich: Urban & Schwarzenberg; 1975.