CHAPTER 27 Anatomy and Biomechanics of Forearm Rotation
Evolution
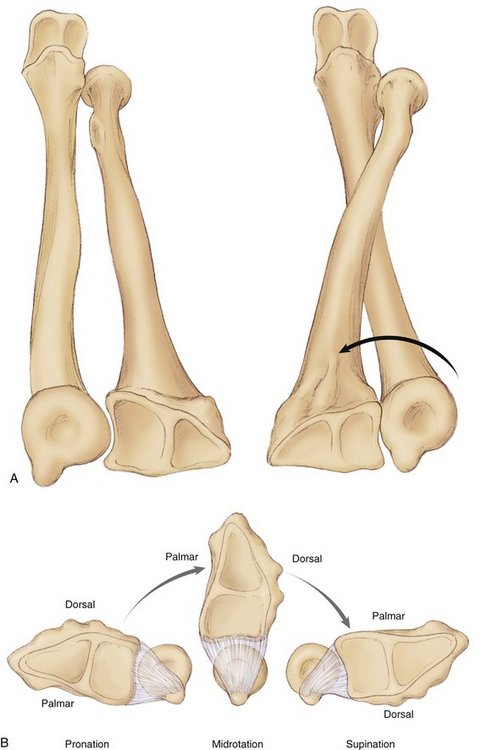
Pronation and supination are rotational motions that exist exclusively in the forearm. The mechanical bases for these movements are the existence of two forearm bones and the presence of two coupled trochoid joints—the proximal and distal radioulnar joints (PRUJ and DRUJ).1 Two bones at the forearm are an inheritance from a remote ancestor, the icthyostega, a crossopterygian tetrapod that sprang up from the sea 300 million years ago, transforming its fins into members.2 This unique ability to transfer rotational force to the grasping hand must have played a decisive role in the human evolution.3 Two bones in comparison to one bone with one joint bring advantages—no tendon, nerve, and vessel twisting at the wrist with decreased function. Furthermore, only two bones at the forearm provide a wide range of motion but stable and light construction.4
The DRUJ and PRUJ together work as a single “forearm joint,” resulting in pronation/supination. Hagert5 compared the montages of the forearm with a ventral view of the leg. The proximal ulnar and distal radial segments create a unit similar to the tibia. The olecranon resembles the patella fused with the tuberosity of the tibia; the radial styloid resembles the medial malleolus at the ankle. The proximal radial and distal ulnar segments create a unit reminiscent of the fibula with the ulnar styloid resembling the lateral malleolus.
Anatomy
Distal Radioulnar Joint
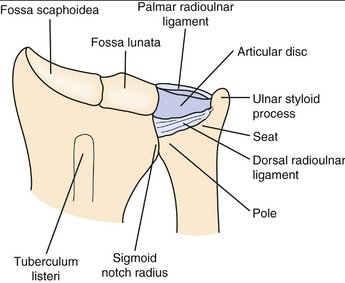
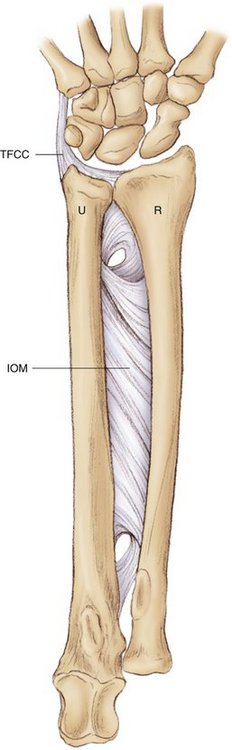
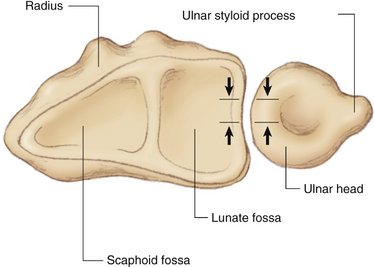
The DRUJ consists of two parts: the radioulnar articulation and the ulnoligamentous articulation. The border between these two components is defined as the ulnar extension of a line along the subchondral bone of the distal radius. The articular surface of the distal radius toward the ulnar head is the sigmoid notch, and the corresponding surface of the ulnar head constitutes the seat of the joint.6 The sigmoid notch is a shallow concave articular surface for the ulnar head; it is convex proximally and concave distally, where it meets the lunate facet on its medial surface.7 The radius and ulna are constrained from proximal to distal by the annular ligament, interosseous membrane (IOM), and triangular fibrocartilage (TFC) (Fig. 27-1).7 There is a variation in the relative lengths of the forearm bones, as measured at the wrist. By convention, an ulnar-neutral variance is one in which the distal cortical surface of the ulnar pole is level with the cortical surface of the most proximal aspect of the lunate fossa. This is measured perpendicular to the longitudinal axis of the forearm when the radiograph is taken with the forearm and wrist in neutral extension and neutral deviation and with the x-ray tube perpendicular to the plane of the radiocarpal joint.7 An ulnar-negative variance indicates an ulna that is shorter than the lunate fossa of the radius and an ulnar-positive variance indicates an ulna that is longer. Although most forearms are within 2 mm of a positive variance and 4 mm of a negative variance, pathological conditions are more prevalent at the extremes.8 The shape of the ulnar head depends on the lengths of the ulna and radius. If the ulna is shorter than the radius (ulnar negative), the ulnar head is cone shaped. If the ulna and radius are similar in length, the ulnar head is cylindrical (ulnar neutral). If the ulna is longer than the radius (ulnar positive), the ulnar head is spherical (Fig. 27-2).9,10
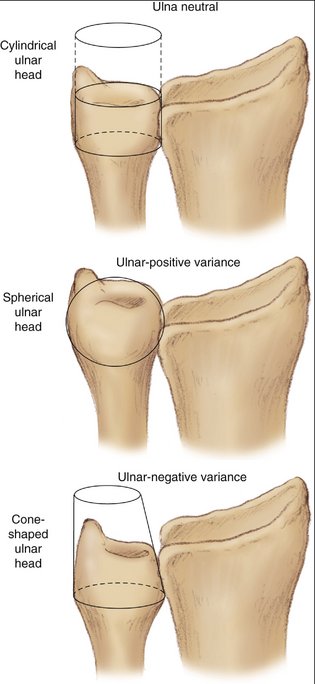
FIGURE 27-2 Shaping of the ulnar head depends on the length of the bone and its different anatomical configurations.
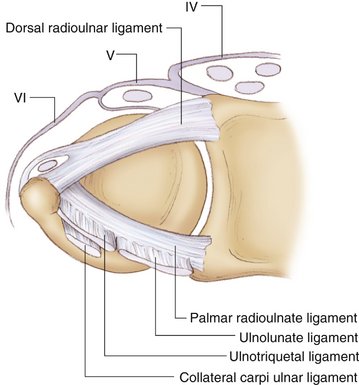
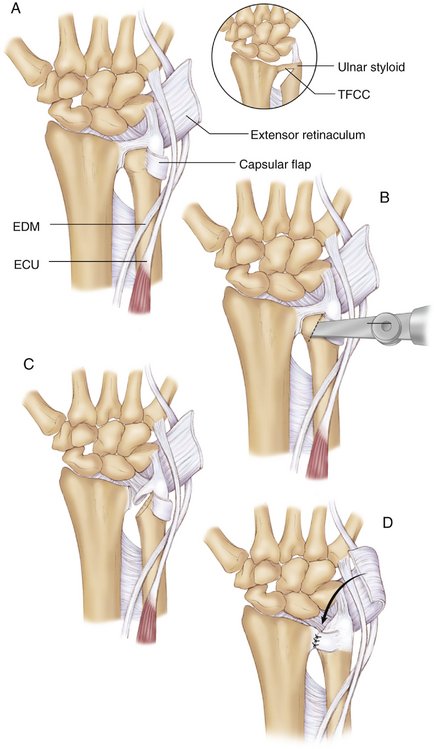
Aside from the seat, the ulnar head articulates with the TFC.7 The triangular fibrocartilage complex (TFCC) consists of the dorsal and palmar radioulnar ligaments, the meniscus homologue, and the articular disc. The dorsal radioulnar ligament attaches to the dorsal rim of the distal radius at the level of the sigmoid notch and courses obliquely ulnarly and anteriorly to insert with the palmar radioulnar ligament into the fovea of the ulnar head and the styloid process. The palmar radioulnar ligament attaches radially to the palmar rim of the distal radius at the level of the sigmoid notch and courses obliquely ulnarly and dorsally to attach with the dorsoulnar ligament to the fovea of the ulnar head and the ulnar styloid process (Fig. 27-3).11
Interosseous Membrane
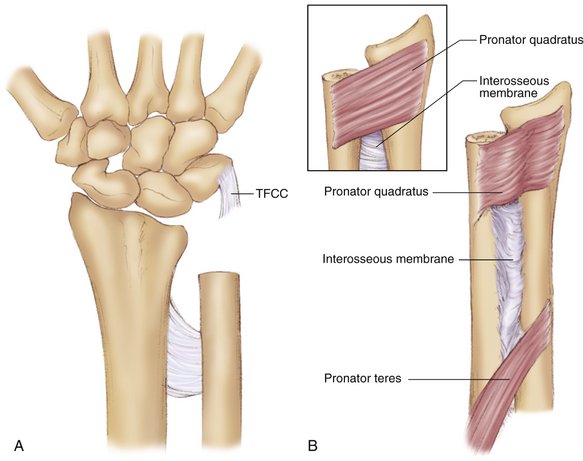
The IOM is a quadrangular sheath that extends from the radius to the ulna, filling the interosseous space. It links both bones of the forearm and also separates the anterior and the posterior compartments of the forearm. Proximally and distally the membrane is not continuous and is perforated by posterior and anterior interosseous vessels (Fig. 27-4).1
Fibers in the anterior plane run distally and obliquely from the medial border of the radius to the lateral border of the ulna. Three bundles are distinguished: the proximal descending fibers are almost horizontal, the intermediate descending fibers follow a short oblique direction, and the distal descending fibers have a long, oblique trajectory.1 In the posterior plane, fibers run proximally and obliquely from the radius to the ulna. The proximal ascending bundle is short, oblique, and quite strong. It arises from the interosseous tubercle of the radius and ends at the proximal ulna. The distal ascending bundle is inconstant. Its direction is long oblique. It arises from the distal radius and reaches the proximal ulna.1 Hotchkiss and coworkers studied the role of the IOM in preventing proximal migration of the radius. In their cadaver study, they found a discrete central band or thickening.12 The central band was responsible for 71% of the longitudinal stiffness of the forearm, whereas the TFCC was responsible for only 8%.
From the IOM of the forearm a tract extends to the dorsal capsule of the DRUJ. It originates from the radius 22 mm proximal to the distal dorsal corner of the sigmoid notch and inserts distally at the capsule of the DRUJ between the tendon sheaths of the extensor digiti minimi and extensor carpi ulnaris. The tract of the IOM is taut in pronation and loose in supination. It strengthens the dorsal capsule of the DRUJ, forming a sling that protects the ulnar head during pronation.13
Proximal Radioulnar Joint
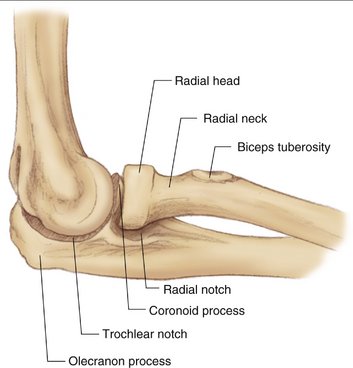
The PRUJ is not a “hinge” but rather a ball-and-socket type of articulation.5 The radial head has a 360-degree convex articulating surface. The head is ovoid rather than circular and is offset approximately 15 degrees from the longitudinal axis of the radius. Cartilage covers 240 degrees of the radial head, which articulates with the ulna at the PRUJ.
The stability of the PRUJ is excellent because the radial head is enclosed in a very strong osteoligamentous cavity that is made of the radial notch of the ulna and the annular ligament, which is a very resistant ligament (Fig. 27-5). There are rarely problems with the joint, except in fractures of the radial head.4
Biomechanics
Kinetics
The ulnar head moves in a rolling and sliding motion from the dorsal to the palmar rim of the sigmoid notch as the joint moves from pronation to supination.7 From pronation to supination, the TFC is taut first dorsally and then palmarly in the same sequence.7 The radius rotates around the ulnar head about a longitudinal axis that passes roughly through the center of the radial head at the PRUJ at the elbow to the fovea of the ulnar head at the level of the wrist (Fig. 27-6).7 The axes of the two radioulnar joints must be aligned coaxially; if not, forearm rotation is blocked. Kapandji compared this situation with a door where two hinges of the door are not aligned; thus, the door cannot be opened.4
The ulnar variance depends on the length of both forearm bones (see earlier), as well as gripping and forearm rotation. The radius migrates proximally with forearm pronation, which increases ulnar variance.14 Maximal ulnar variance is found when gripping with the forearm in pronation; minimal ulnar variance occurs when the hand is relaxed and the forearm is in supination.15 In the pronated position the radius becomes shorter than the ulna and the inferior aspect of the ulna head moves palmarward with regard to the lower rim of the radial sigmoid notch. When there is loss of radial height after a distal radius fracture, resulting in an ulnar-positive variance, pronation increases the impaction to the carpus, particularly the lunate and triquetrum.4
Rotation of the forearm allows the palm of the hand to be directed facing upward, medially, and downward while the elbow is flexed and anteriorly, medially, and posteriorly with an extended elbow. The total arc of rotation is close to 180 degrees. Rotation of the forearm associated with rotation of the shoulder allows for 270 degrees of rotation of the upper limb.1 Because the seat of the ulna fills the sigmoid notch of the radius only in a sector of 90 to 135 degrees, increasing pronation and supination gradually diminishes the contact area. In maximal pronation or supination, the joint surfaces of the seat and sigmoid notch have a marginal contact of 2 to 3 mm.6 Joint surface contact is optimal only in a neutral forearm position (Fig. 27-7).
The ulna and radius transmit loading forces to the elbow and wrist, respectively. Eighteen percent of the load that is transmitted through the wrist passes through the ulna and 82% passes through the radius.16 With the elbow extended, 60% of the load is transmitted through the radius and 40% through the ulna.1 The force transmission through the wrist was investigated by Schuind and associates, who found that the force transmission ratio at the radioulnocarpal joint was 55% through the radioscaphoid and 35% through the radiolunate joints. The remaining 10% of the load passed through the TFC.17
Stability is provided by the contour of the joints, the surrounding ligaments, and the crossing muscles.18 However, the dominant structures stabilizing the DRUJ are the ligamentous components of the TFCC proper. The major constraint to dorsal translation of the distal ulna relative to the radius is the palmar radioulnar ligament. Palmar translation of the distal ulna relative to the radius is constrained primarily by the dorsal radioulnar ligament, with secondary constraint provided by the palmar radioulnar ligament and IOM. In each position the IOM becomes the main stabilizing structure that prevents dislocation of the DRUJ.5 Hotchkiss and colleagues reported that the IOM was most stiff in forearm supination and least stiff in pronation.12 The trajectories of the collagen fibers that make up these two ligaments run in a somewhat helical course from origin to insertion. They do not resist axial radial translation well. Schuind and associates examined the role of the TFCC in stabilizing the DRUJ in pronation and supination and in the transverse plane. They found that the palmar radioulnar ligament of the TFCC is taut in supination and the dorsal radioulnar ligament is taut in pronation. In full pronation, the palmar radioulnar ligament decreased to an average of 71% of its length in tension. In full supination, the dorsal radioulnar ligament decreased to an average of 90% of its length. Furthermore, they observed that in the transverse plane the TFCC was less stiff in neutral forearm rotation than in pronation and supination.18 The ulnocarpal ligaments and extensor carpi ulnaris subsheath did not contribute significantly to DRUJ stability; however, approximately 20% of DRUJ constraint is provided by the articular contact of the radius and ulna.19 Additionally, the extensor retinaculum does not play a part in stabilization of the DRUJ, but the tension of the extensor carpi ulnaris in its intact fibro-osseus tunnel does.20
Motor Muscles of Pronation and Supination
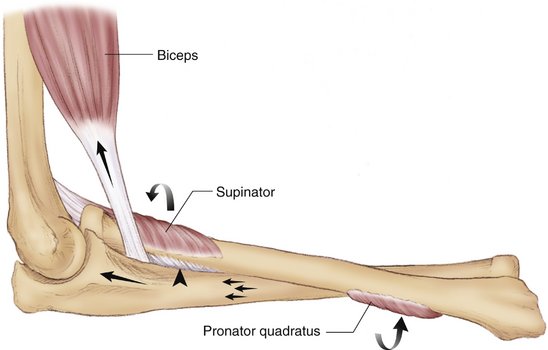
Four important major muscles provide active motion of the DRUJ: the pronator quadratus muscle and the pronator teres, innervated by the median nerve, pronate the forearm; and the biceps brachii, which is innervated by the musculocutaneus nerve, and the supinator muscle, innervated by the radial nerve, provide supination (Fig. 27-8).5 The supinator muscle originates from the lateral epicondyle of the humerus, supinator crest of the ulna, and radial collateral ligament and inserts at the lateral proximal radial shaft. The muscle acts by a mechanism of unrolling. It has been established that slow unresisted supination is brought about by the independent action of the supinator, whereas fast resisted and unresisted supination is assisted by the action of the biceps muscle.21 The pronator quadratus muscle is shown to be the prime pronator for the forearm in all positions of elbow flexion and extension.21 There are two distinct heads of the pronator quadratus: superficial and deep.22 The superficial head takes origin from a short tendon on the dorsoulnar border of the ulna and inserts into a broad flat facet on the palmar surface of the radius. The deep head takes origin in a similar manner to the superficial head, but with a slightly less distinct tendon and from a slightly more palmar position of the ulna.23 The pronator teres has two heads. The humeral head, which is larger and more superficial, arises immediately above the medial epicondyle of the humerus. The ulnar head is a thin fasciculus that arises from the medial side of the coronoid process of the ulna. The muscle passes obliquely across the forearm and ends in a flat tendon, which is inserted into a rough impression at the middle of the lateral surface of the radius, just below the insertion of the supinator. The pronator teres muscle is stronger in the flexed elbow than in the extended elbow. The flexor and extensor carpi ulnaris muscles may be responsible for initiating pronation from maximal supinated position.24 Supination is accomplished through the action of the supinator muscle and the biceps at the proximal quarter of the forearm, whereas pronation is achieved through the actions of the pronator teres and pronator quadratus, which act distal to the midpoint of the forearm.7 Supinatory torque is approximately 15% greater than pronatory torque.25 The brachioradialis muscle is not usually a supinator, except when the forearm is in complete pronation (see Fig. 27-8). The S-shaped configuration of the radius around the axis of pronation/supination determines, anatomically, the sizes of the lever arms of the pronating/supinating muscles5 (see Fig. 27-6).
Clinical Consequences
Dislocation/Subluxation
Clinically, the majority of dislocations involving the DRUJ are dorsal, where the distal ulna is dorsal to the radius. It has been believed that the combination of forearm pronation and wrist hyperextension predisposes to this injury pattern.26–28 Instability of the distal ulna at the DRUJ can result from dislocations, radius and ulna fractures, malunions, and ligament injuries. Avulsion of the radioulnar ligaments from either the radial or ulnar origins results in increased mobility of the ulnar head on the radius, which may be detected by ballottement tests such as the “piano key sign” (Fig. 27-9). The unstable distal ulna most commonly presents with dorsal displacement of the ulnar head and a carpal supination deformity (see Fig. 27-9).29

FIGURE 27-9 A, “Piano key” sign. B, Dorsal subluxation of the DRUJ. C, CT scan (axial view) of dorsal subluxation.
(Courtesy of Dr. Richard A. Berger, Mayo Clinic, Rochester, Minnesota)
Adams recently described true anatomical reconstruction of the distal radioulnar ligament for post-traumatic DRUJ instability (Fig. 27-10).30,31 The DRUJ is stabilized by a tendon graft (e.g., palmaris longus tendon) for reconstruction of the palmar and dorsal radioulnar ligament.
Fractures
Traumatic subluxations and dislocations of the DRUJ can be isolated phenomena,28,32 but they can also occur in association with fractures of the radius, ulna, or both. Distal radius fractures with concomitant DRUJ instability are more common than previously thought.33 Recent studies have shown that the associated pathology in the DRUJ is a major contributor to long-term loss of motion and poor clinical outcomes after distal radius fractures.34,35 Recent data, however, seem to indicate that it is not merely the presence of a styloid fracture that matters but the location of that fracture relative to the base and its amount of displacement that relates to the outcome.36 Fracture at the base of the ulnar styloid and significant displacement of an ulnar styloid fracture were found to increase the risk of DRUJ instability. Significant displacement of an ulnar styloid is an indication for internal fixation (Fig. 27-11).
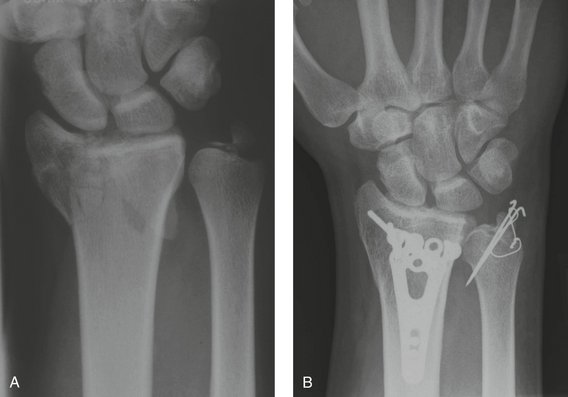
FIGURE 27-11 A, Radiograph of distal radius fracture with fracture at the base of the ulnar styloid. B, Fixation of the fracture.
(Courtesy of Hermann Krimmer, MD, Center for Hand Surgery, Ravensburg, Germany.)
In the case of Galeazzi fracture-dislocation, there is a complex traumatic disruption of the DRUJ that is associated with an unstable radius fracture, commonly at the junction of the middle and distal thirds of the radial shaft. This injury represents nearly 7% of all fractures of the forearm.37 The mechanism of injury is often a high-velocity direct impact with forceful forearm pronation.38 This injury is often treated with open reduction and internal fixation of the radius fracture and open or pin fixation of the DRUJ and repair of the ligaments.
The Monteggia fracture consists of a fracture to the proximal third of the ulna with a concomitant dislocation of the radial head. The Galeazzi lesion is three times more common than the Monteggia pattern of injury. The most common mechanism for a Monteggia fracture-dislocation is a fall on an outstretched and hyperpronated hand, resulting in an ulnar shaft fracture and anterior radial head dislocation.39 Monteggia fracture-dislocations are usually considered a more severe injury in adults, who most often require open reduction and internal fixation.40
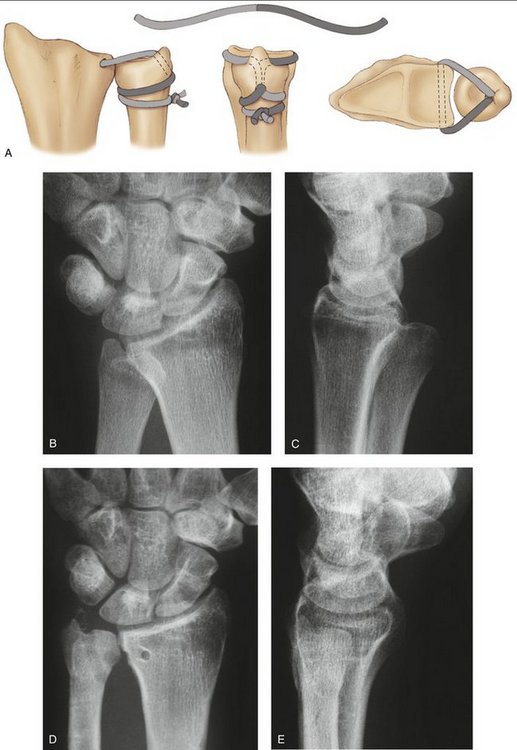
The longitudinal stability of the forearm can be altered in some high-energy radial head fractures, such as the Essex-Lopresti lesion.41 In this lesion there is a comminuted radial head fracture. This injury is associated with a proximal migration of the radius in case of a dislocation of the DRUJ and the IOM is ruptured completely.1 This type of accident is one of the worst case scenarios in forearm injuries. Radiographs of the elbow should be routinely performed when there is suspicion of PRUJ injury (Fig. 27-12).

FIGURE 27-12 Essex-Lopresti injury. A, Radiograph shows dislocation of the DRUJ. B, Radial head fracture.
(Courtesy of Hermann Krimmer, MD, Center for Hand Surgery, Ravensburg, Germany.)
To allow for longitudinal migration of the radius, the whole membrane must be disrupted, because one ascending and one descending group of fibers suffice to prevent these displacements.1 If the IOM is intact, even with excision of the PRUJ and DRUJ, the radius maintains its longitudinal stability.1 As mentioned earlier, the central band of the IOM is responsible for 71% of the longitudinal stiffness of the forearm, whereas the TFCC is responsible for 8%.12 The stability of the DRUJ is minimally supported by bony architecture.42
The potential importance of dynamic stabilization of the DRUJ by the extensor carpi ulnaris and the pronator quadratus, especially the deep head, has been proposed and even recognized in some innovative surgical reconstruction procedures. The majority of dislocations involving the DRUJ are dorsal, where the distal ulna is dorsal to the distal radius. The radius of the curvature of the sigmoid notch is 4 to 7 mm larger than that of the ulnar head; and, consequently, pronation and supination are a combined rotation and sliding movement in the DRUJ.6 In the DRUJ, stability supported by joint surface architecture is minimal and the ligament is therefore of particular importance for stability.6
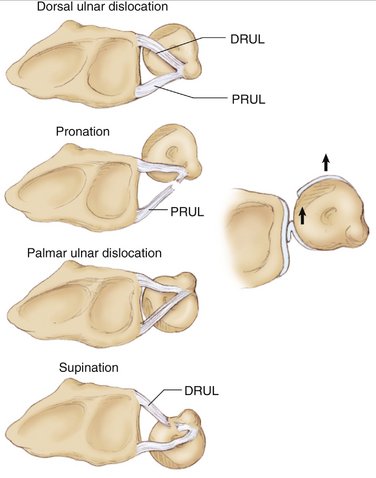
With the forearm in neutral position the palmar and dorsal ligaments are relaxed.6 If the palmar ligament is injured, the radius dislocates palmarly in pronation. In supination, the opposite occurs: the dorsal radioulnar ligament is taut (Fig. 27-13).6
Arthrosis
Arthrosis of the DRUJ is a common problem, often leading to substantial disability from pain, weakness, and instability. Such degenerative changes can result from mismatches in the length of the radius and ulna distally, traumatic disruptions of the soft tissues that stabilize the DRUJ, fractures involving the mutual articulating surfaces of the radius and ulna, or any combination thereof. Therefore, resection of one or both articular surfaces of the DRUJ is the treatment of choice. This can take several forms, such as resection of the entire ulnar head (Darrach procedure) (Fig. 27-14),43 partial resection of the joint surfaces with or without interposition of connective soft tissue (Fig. 27-15),44,45 or fusion of the distal radius and ulna with creation of a proximal pseudarthosis.46 The results of a biomechanical investigation showed less instability of the hemi-resection arthroplasty in comparison with the Darrach procedure.47
In a recently performed biomechanical study, the implantation of an ulnar head endoprosthesis effectively restored the stability of the DRUJ by simulating the geometry of the ulnar head (Fig. 27-16).48 There were significantly better results after the implantation of the prosthesis compared with the Darrach procedure. The interposition of the pronator quadratus muscle or tenodesis with the extensor and flexor carpi ulnaris tendons49 did not reduce the radioulnar convergence created by resection of the distal ulna50 and showed significantly worse results in comparison with the prosthesis implantation.48 Neither of the two soft tissue stabilizations could prevent radioulnar impingement.48 Implant arthroplasty of the distal ulna combined with an adequate soft tissue repair is recommended to improve pain, function, and strength of the wrist and forearm to treat painful disorders of the DRUJ secondary to instability and arthrosis.51
1. Poitevin LA. Anatomy and biomechanics of the interosseous membrane: its importance in the longitudinal stability of the forearm. Hand Clin.. 2001;1:97-110.
2. Kapandji AI. Why are there two bones in the forearm? Ann Chir.. 1975;29:463-470.
3. Lewis OJ. Evolutionary change in primate wrist and inferior radio-ulnar joints. Anat Rec.. 1965;151:275-285.
4. Kapandji A. Biomechanics of pronation and supination of the forearm. Hand Clin.. 2001;17:111-122.
5. Hagert CG. The distal radioulnar joint in relation to the whole forearm. Clin Orthop Relat Res.. 1992;275:56-64.
6. Ekenstam F. Anatomy of the distal radioulnar joint. Clin Orthop Relat Res.. 1992;275:14-18.
7. Linscheid R. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res.. 1992;275:46-55.
8. Czitrom AA, Dobyns JH, Linscheid RL. Ulnar variance in carpal instability. J Hand Surg [Am]. 1987;2:205-208.
9. Forstner H. The distal radio-ulnar joint: morphologic aspects and surgical orthopedic consequences. Unfallchirurg.. 1987;11:512-517.
10. De Smet L. Ulnar variance: facts and fiction. Review article. Acta Orthop Belg.. 1994;1:1-9.
11. Berger RA. The anatomy of the ligaments of the wrist and distal radioulnar joints. Clin Orthop Relat Res.. 2001;383:32-40.
12. Hotchkiss RN, An KN, Sowa DT, et al. An anatomic and mechanical study of the interosseous membrane of the forearm: pathomechanics of proximal migration of the radius. J Hand Surg [Am].. 1989;14:256-261.
13. Gabl M, Zimmermann R, Angermann P, et al. The interosseous membrane and its influence on the distal radioulnar joint: an anatomical investigation of the distal tract. J Hand Surg [Br].. 1998;23:179-182.
14. Goodfellow JW, Bullough PG. The pattern of ageing of the articular cartilage of the elbow joint. J Bone Joint Surg Br.. 1967;49:175-181.
15. Jung JM, Baek GH, Kim JH, et al. Changes in ulnar variance in relation to forearm rotation and grip. J Bone Joint Surg Br. 2001;83:1029-1033.
16. Palmer AK, Werner FW, Glisson RR, Murphy DJ. Partial excision of the triangular fibrocartilage complex. J Hand Surg [Am].. 1988;3:391-394.
17. Schuind F, Cooney WP, Linscheid RL, et al. Force and pressure transmission through the normal wrist: a theoretical two-dimensional study in the posteroanterior plane. J Biomech.. 1995;28:587-601.
18. Schuind F, An KN, Berglund L, et al. The distal radioulnar ligaments: a biomechanical study. J Hand Surg [Am].. 1991;6:1106-1114.
19. Stuart PR, Berger RA, Linscheid RL, An KN. The dorsopalmar stability of the distal radioulnar joint. J Hand Surg [Am].. 2000;4:689-699.
20. Spinner M, Kaplan EB. Extensor carpi ulnaris: its relationship to the stability of the distal radio-ulnar joint. Clin Orthop Relat Res.. 1970;68:124-129.
21. Basmajian J, Deluca CJ. Butler J, editor ed. Muscles Alive. Their Functions Revealed by Electromyography; 1985; Williams & Williams: Baltimore; 280-289.
22. Johnson RK, Shrewsbury MM. The pronator quadratus in motions and in stabilization of the radius and ulna at the distal radioulnar joint. J Hand Surg [Am].. 1976;3:205-209.
23. Stuart PR. Pronator quadratus revisited. J Hand Surg [Br].. 1996;21:714-722.
24. Haugstvedt JR, Berger RA, Berglund LJ. A mechanical study of the moment-forces of the supinators and pronators of the forearm. Acta Orthop Scand.. 2001;72:629-634.
25. Askew LJ, An KN, Morrey BF, Chao EYS. Isometric elbow strength in normal individuals. Clin Orthop Relat Res.. 1987;222:261-266.
26. Hui FC, Linscheid RL. Ulnotriquetral augmentation tenodesis: a reconstructive procedure for dorsal subluxation of the distal radioulnar joint. J Hand Surg [Am]. 1982;3:230-236.
27. Buterbaugh GA, Palmer AK. Fractures and dislocations of the distal radioulnar joint. Hand Clin.. 1988;3:361-375.
28. Heiple KG, Freehafer AA. Isolated traumatic dislocation of the distal end of the ulna or distal radio-ulnar joint. J Bone Joint Surg Am.. 1962;44:1387-1394.
29. Bowers WH. Problems of the distal radioulnar joint. Adv Orthop Surg. 1984;7:289-303.
30. Adams BD. Anatomic reconstruction of the distal radioulnar ligaments for DRUJ instability. Tech Hand Up Extrem Surg. 2000;4:154-160.
31. Adams BD, Berger RA. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg [Am].. 2002;2:243-251.
32. Rainey RK, Pfautsch ML. Traumatic volar dislocation of the distal radioulnar joint. Orthopedics.. 1985;7:896-900.
33. Frykman GK. Fractures of the distal radius including sequelae of shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function: a clinical and experimental study. Acta Orthop Scand. 1967;108(Suppl.):7-153.
34. Cooney WP3rd, Dobyns JH, Linscheid RL:. Complications of Colles’ fractures. J Bone Joint Surg Am.. 1980;62:613-619.
35. Stoffelen D, De Smet L, Broos P. The importance of the distal radioulnar joint in distal radial fractures. J Hand Surg [Br].. 1998;23:507-511.
36. May MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg [Am].. 2002;27:965-971.
37. Dameron TB. Traumatic dislocation of the distal radioulnar joint. Clin Orthop Relat Res.. 1972;83:55-63.
38. Mikic ZD. Galeazzi fracture-dislocations. J Bone Joint Surg Am.. 1975;57:1071-1080.
39. Boyd HB, Boals JC. The Monteggia lesion: a review of 159 cases. Clin Orthop Relat Res.. 1969;66:94-100.
40. Ring D, Jupiter JB. Current concepts review: fracture-dislocation of the elbow. J Bone Joint Surg.. 1998;80:566-580.
41. Essex-Lopresti P. Fractures of the radial head with distal radioulnar dislocation: report of two cases. J Bone Joint Surg Br.. 1951;33:244-247.
42. Ekenstam F, Hagert CG. Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg.. 1985;1:17-25.
43. Darrach W. Partial excision of lower shaft of ulna deformity following Colles fracture. Ann Surg.. 1913;57:764-765.
44. Bowers WH. Distal radioulnar joint arthroplasty: the hemiresection–interposition technique. J Hand Surg [Am].. 1985;10:169-178.
45. Watson HK, Ryu JJ, Burgess RC. Matched distal ulnar resection. J Hand Surg [Am].. 1986;11:812-817.
46. Kapandji IA. Opération de Kapandji-Sauvé: techniques et indications dans les affections non rhumatismales. Ann Chir Main.. 1986;5:181-193.
47. Sauerbier M, Fujita M, Hahn ME, et al. The dynamic radioulnar convergence of the Darrach procedure and the ulnar head hemiresection interposition arthroplasty: a biomechanical study. J Hand Surg [Br].. 2002;4:307-316.
48. Sauerbier M, Hahn ME, Fujita M, et al. Dynamic radioulnar convergence after Darrach operation, soft tissue stabilizing operations of the distal ulna, and ulnar head prosthesis implantation—an experimental biomechanical study. Unfallchirurg.. 2002;8:688-698.
49. Breen TF, Jupiter JB. Extensor carpi ulnaris and flexor carpi ulnaris tenodesis of the unstable distal ulna. J Hand Surg [Am].. 1989;4:612-617.
50. Sauerbier M, Berger RA, Fujita M, Hahn ME. Radioulnar convergence after distal ulnar resection: mechanical performance of two commonly used soft tissue stabilizing procedures. Acta Orthop Scand.. 2003;4:420-428.
51. Willis AA, Berger RA, Cooney WP3rd:. Arthroplasty of the distal radioulnar joint using a new ulnar head endoprosthesis: preliminary report. J Hand Surg [Am].. 2007;32:177-189.