Chapter 40 Anatomical Retroscrew Anterior Cruciate Ligament Fixation
Single- and Double-Bundle Anterior Cruciate Ligament Reconstruction with Retroscrew Biointerference in a Single Femoral Socket
The concept of anatomic graft positioning for anterior cruciate ligament reconstruction (ACL) has been previously described by many authors.1–6 In the past, anatomical graft tunnels were believed to obtain an optimal ACL reconstruction; the position of the graft within bone tunnels had to avoid the intercondylar roof and wall impingement. Studies have documented the landmarks for the placement of endoscopic tunnels in anatomical reconstructions through a full knee range of motion that will avoid impingement.7,8
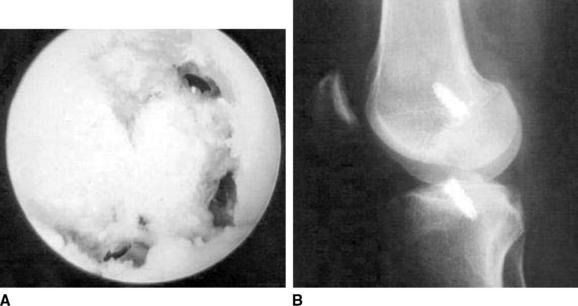
Recently, issues regarding graft fixation position have become important. Experimental and clinical trials have shown that anatomical graft fixation and position at or near the origin and insertion of the native ACL in contrast to nonanatomical fixation position will (1) minimize graft tension, (2) minimize graft length change, (3) produce a more stable reconstruction through full knee range of motion, and (4) avoid anteroposterior, sagittal, windshield wiper–type graft motion.1,2,4,7–10 Five-year follow-up studies comparing anatomical and nonanatomical fixation for ACL reconstruction have shown absence of tunnel expansion up to 5 years with an anatomically fixed graft at the intraarticular tibial tunnel orifice (Fig. 40-1)5,6,8,11,12
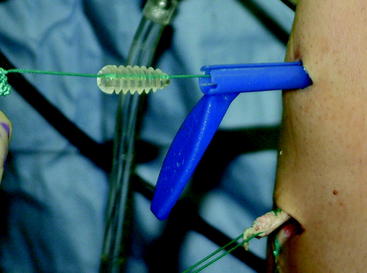
The Retroscrew (Arthrex, Naples, FL) (Fig. 40-2) is inserted into the tibial tunnel in an inside-out position so that the head of the screw achieves aperture fixation at the intraarticular tunnel orifice. Standard interference screw fixation is used on the femoral side. The Retroscrew is beneficial during tensioning because unlike an antegrade screw, the Retroscrew will pull the graft tighter into the tunnel, especially during tensioning.
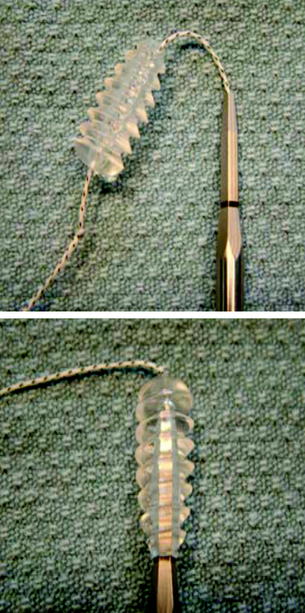
Fig. 40-2 The femoral and tibia Retroscrews are shown. The screws are tethered by a #2 Fiberwire suture.
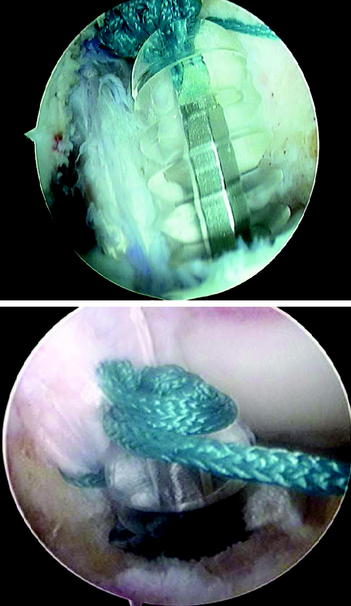
Morgan et al4 first described an “all-inside” technique for ACL reconstruction that addressed the issues of anatomical fixation. However, the procedure was not popular because of its technically demanding nature3,5,6,13 (Fig. 40-3).
Operative Technique: Single Femoral Socket, Single-Bundle Graft
Once the appropriate anatomical bone tunnels have been placed, the graft is passed in a routine fashion. Femoral fixation may be achieved using an interference screw equal to the diameter of the tunnel placed through the anteromedial portal with the knee in hyperflexion. Alternatively, femoral fixation may be accomplished with a specially designed, cannulated Retroscrew driver (Arthrex) passed through the tibial tunnel to achieve parallel interference screw fixation. This is performed using a preloaded Fiberstick Suture (Arthrex) withdrawn from the tip of the screw driver and out the anteromedial portal (see Fig. 40-3).
The #2 suture is then passed through the cannulation of the Retroscrew, and a 3-mm Mulberry knot is tied to prevent the screw from disengaging the driver. Intraarticular passage of the femoral Retroscrew from the anteromedial portal is facilitated with the aid of a flexible slotted cannula (shoehorn cannula, Arthrex) at the same time as the suture exiting the handle portion of the screwdriver is pulled (Fig. 40-4). The shoehorn cannula avoids hang-up of the screw in the fat pad. This is used to secure and lead a femoral Retroscrew (7 to 10 mm × 20 mm) onto the driver tip. Once the screw has been securely placed onto the end of the driver, the suture may be removed. With the leg in approximately 90 degrees of flexion, the screw is advanced into the femoral socket to secure the femoral side of the graft.
Tibial fixation can next be performed by placing a tibial Retroscrew equal to the tunnel diameter. As previously described, the tibial Retroscrew (8 to 10 mm × 20 mm) is placed onto the driver tip over a #2 Fiberwire suture from the medial portal. It is important that the screwdriver tip be anterior to the graft and free of all soft tissue. Obscuring the tip will prevent seating of the screw on the driver. Once inside the joint, the screw is “flipped” onto the driver by pulling the suture exiting the driver handle at the same time as the driver tip is lowered into the aperture (Fig. 40-5). The screw is then secured to the driver by wrapping the exiting suture around the grommets on the driver handle.
Operative Technique: Single Femoral Socket, Double-Bundle Graft
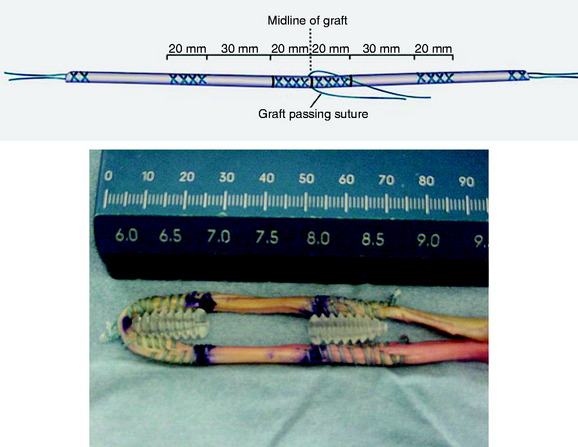
The simplicity of this technique is what makes it appealing. Only minor modifications are made to the previously described single-bundle procedure. Our preferred graft source for the double-bundle technique is a two-limbed tibialis tendon allograft. During preparation, it is recommended that it be prepared in the manner described by Charlick and Caborn.14 Specifically, this may be carried out by suturing (#2 Fiberwire) 20 mm to either side of the midline of the folded soft tissue graft (Fig. 40-6). If a hamstring graft is chosen, the semitendinosus and gracilis tendons should first be sutured together under tension to create a two-limbed, folded graft. Further suturing is performed distally after accommodating 30 to 35 mm for the intraarticular portion of the graft. This additional whipstitch aids in controlling the anteromedial bundle (AMB) and posterolateral bundle (PLB) as they are oriented into the femoral and tibial tunnels. Caborn stitching has been shown to increase pullout to failure by approximately 30% when using interference screw fixation for soft tissue grafts.14
After standard femoral and tibial socket preparation, to create the double-bundle socket on the femur, a notching device is used to create two slots on the femoral socket intraarticular orifice, for the AMB and PLB of the ACL graft, respectively. The slots can be further delineated using a motorized bur or shaver or a curved curette (Fig. 40-7). With the knee flexed 90 degrees, the AMB slot is made at the 10- or 2-o’clock position and the PLB slot is made at the 4- or 8-o’clock position within the circumference of the tunnel orifice. Each slot is typically 6 to 7 mm in width.
The graft is then passed in routine fashion using a Beath pin. While the graft is held into the tunnel by an assistant, the limbs of the graft are rotated into their respective notches. The AMB is retraced by a probe from the anteromedial portal. Femoral fixation is then carried out with a concentrically placed femoral Retroscrew placed central between the bundles and secured into position by the driver, which is passed through the tibial tunnel as described previously (Fig. 40-8). As the screw is advanced in the tunnel, the graft strands will seek the two-bundle origin of the ACL in their respective slots (Fig. 40-9).
1 Barber FA. Flipped patellar tendon autograft anterior cruciate ligament reconstruction. Arthroscopy. 2000;16:483-490.
2 Ishibashi Y, Rudy T, Livesay G, et al. The effect of anterior cruciate ligament graft fixation site at the tibia on knee stability: evaluation using a robotic testing system. Arthroscopy. 1997;13:177-182.
3 Leitman EH, Morgan CD, Grawl DM. Quadriceps tendon anterior cruciate ligament reconstruction using the all-inside technique. Operative Tech Sports Med. 1999;7:179-188.
4 Morgan CD, Kalman VH, Grawl D. Isometry testing for anterior cruciate ligament reconstruction revisited. Arthroscopy. 1995;11:647-659.
5 Palmeri M, Morgan CD. The all-inside anterior cruciate ligament reconstruction: a double socket approach. Operative Tech Orthop. 1996;6:161-176.
6 Stahelin A, Weiler A. All-inside anterior cruciate ligament reconstruction using semitendinosus tendon and soft threaded biodegradable interference screw fixation. Arthroscopy. 1997;13:773-779.
7 Howell SM, Clark JA. Tibial tunnel placement in ACL reconstructions and graft impingement. Clin Orthop. 1992;283:187-195.
8 Morgan CD, Kalman VH, Grawl DM. Definitive landmarks for reproducible tibial tunnel placement in anterior cruciate ligament reconstruction. Arthroscopy. 1995;11:275-288.
9 Howell SM, Clark JA, Farley TE. A rationale for predicting anterior graft impingement by the intercondylar roof. A magnetic resonance imaging study. Am J Sports Med. 1991;19:276-281.
10 L’Insalata JC, Klatt B, Fu FH, et al. Tunnel expansion following anterior cruciate ligament reconstruction: a comparison of hamstring and patellar tendon autografts. Knee Surg Sports Traumatol Arthrosc. 1997;5:234-238.
11 Weiler A, Hoffman RFG, Bail HJ, et al. Tendon healing in a bone tunnel. Part II: histologic analysis after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy. 2002;18:124-135.
12 Weiler A, Peine R, Pashmineh-Azar A, et al. Tendon healing in a bone tunnel. Part I: biomechanical results after biodegradable interference fit fixation in a model of anterior cruciate ligament reconstruction in sheep. Arthroscopy. 2002;18:113-123.
13 Morgan CD. Quadriceps tendon autograft for ACL reconstruction. In Jackson D, editor: Master techniques in orthopaedic surgery, ed 2, New York: Lippincott, 2002, Lippincott.
14 Charlick DA, Caborn DN. Alternative soft-tissue graft preparation technique for cruciate ligament reconstruction. Arthroscopy. 2000;16:E20.
Brand JCJr, Pienkowski D, Steenlage E, et al. Interference screw fixation: strength of a quadrupled hamstring tendon graft is directly related to bone mineral density and insertion torque. Am J Sports Med. 2000;28:705-710.
Morgan CD, Caborn D. Anatomic graft fixation using a retrograde biointerference screw for endoscopic anterior cruciate ligament reconstruction: single-bundle and 2-bundle techniques. Tech Orthop. 2005;20:297-302.