Chapter 24 Anatomical Double-Bundle Anterior Cruciate Ligament Reconstruction with a Semitendinosus Hamstring Tendon Graft
Introduction
Conventional techniques of reconstructing the torn ACL employ the use of either a bone–patellar tendon or hamstring graft. The majority of these reconstruction techniques, however, basically reconstructs the anteromedial (AM) bundle of the cruciates as the femoral tunnel is placed between the 10- and 11-o’clock position for the right knee (or 1- and 2-o’clock position for the left knee). Although good results have been generally demonstrated concurrent with its ability to restore the knee’s anteroposterior (AP) stability, questions remain regarding its efficiency in restoring rotational stability.1 Recently, the performance of an anatomical double-bundle reconstruction technique has generated renewed interests as several in vitro analyses demonstrated better results in terms of restoring knee rotational stability.2–8
Performing an anatomical double-bundle reconstruction usually entails the use of both the semitendinosus (ST) and gracilis (Gr) autografts, requiring the use of independent femoral and tibial fixations.5,9,10 With this technique, therefore, the surgery becomes more costly with the additional fixation required. Moreover, with the use of both the ST/Gr, hamstring strength deficits can become apparent, as has been demonstrated by previous studies.3,4,11
Anatomy of the Anterior Cruciate Ligament
Anatomical studies have shown that the ACL consists of two functional bundles, the AM and the posterolateral (PL) bundle, whose nomenclature is related to their insertion in the tibial plateau.1,12 These two bundles are already identifiable between the 16th to 22nd weeks of fetal development. Analyzing the insertions of these two bundles reveals that they do not lie on the same coronal plane; the AM bundle originates more proximally than the PL bundle. Biomechanically, the AM bundle tightens in flexion while the PL bundle slackens. On the other hand, the PL bundle tightens in extension while the AM bundle loosens.1,13 The ACL attaches to the femur and tibia as a collection of fascicles that fan out as they approach their insertions sites.
Scientific Rationale
Early cadaveric investigations performed by Radford and Amis1 demonstrated the superior AP knee stability achieved through various ranges of flexion with a double-bundle reconstruction compared with single-bundle ACL reconstruction. Their investigation, however, did not include tests for rotational stability. Yamamoto et al,14 on the other hand, reported no significant differences between double-bundle and single-bundle ACL reconstruction of the PL bundle in terms of response to rotatory loads. However, single PL bundle reconstruction was found to be associated with increased anterior tibial translation with application of anterior loads. A more recent cadaveric study emphasized that single-bundle ACL reconstruction is mostly successful in restoring AP knee stability but is inadequate in controlling the combined rotatory loads of internal tibial torque and valgus torque.
In a biomechanical study by Yagi et al6 restoration of the knee kinematics, particularly in terms of rotational control, was also demonstrated to be better with a double-bundle versus single-bundle reconstruction technique. Further in vivo studies by Tashman et al5 also revealed that single-bundle reconstruction sufficiently restores AP tibial translation but failed to provide rotational stability during dynamic loading.
In general, the available studies thus far have demonstrated that single-bundle ACL reconstruction can only partially restore the normal knee kinematics because it limits anterior translation but is unable to control pivot shift. In addition, biomechanical analysis of an anatomically reconstructed knee also demonstrated that anterior tibial translation for double-bundle reconstruction is significantly closer to that of an intact knee and produces better rotatory stability.7,8
Surgical Technique
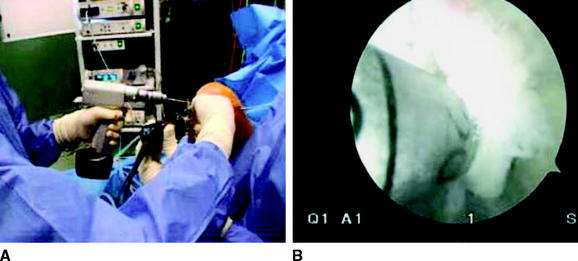
Following the administration of either a spinal or general anesthesia, the patient is positioned supine on the operating table. A tourniquet is placed at the proximal aspect of the thigh with sufficient distance from the expected exit point of the Beath needle in the thigh’s lateral aspect. A lateral post for thigh support and a foot bar are then placed to enable the knee to be positioned at 90 degrees of flexion on the table during surgery. This set-up also allows sufficient provision for full range of motion (Fig. 24-1).
Preparation of the Double-Bundle Semitendinosus Graft
At the back table, while the surgeon prepares the tunnels, the surgical assistant proceeds with the preparation of the double-bundle graft. Once the graft is cleaned and devoid of excess tissues, measurement of the tendon follows. The minimum length needed is 28 cm to allow the possibility of cutting the graft in half, with sufficient length to fold each half of the graft to a length of 7 cm. In such a way, we can have 2 cm of graft length for the femoral and tibial tunnels and 3 cm intra-articularly. The ends of the grafts are then whipstitched using Ticron #5 sutures. The appropriate sizes of the Endobutton-CL (Smith & Nephew Endoscopy, Andover, MA), as determined by the AM and PL tunnel lengths, are then attached at the end of each graft. The diameter of each bundle is then measured using 0.5-mm increment sizers to match the size of the femoral and tibial tunnels. Pretensioning and preconditioning of the grafts with cyclical flexion and extension of the knee under maximal manual tension follow.15,16
Arthroscopic Anterior Cruciate Ligament Reconstruction
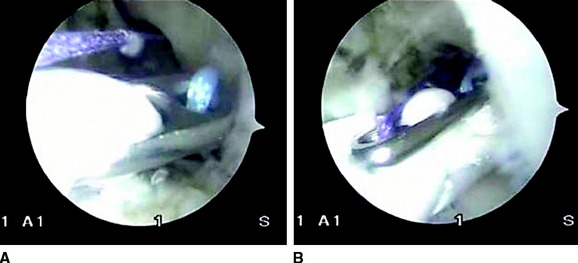
Using standard anterolateral (AL) and AM portals, the knee joint is visualized and prepared for tunnel placements (Fig. 24-2). The anatomical footprints of the native ACL on both the femoral and tibial sides are identified. The PL femoral tunnel is initially prepared using an “outside-in” technique. To properly achieve this step, a customized PL tunnel guide is used. This customized guide has a component arm designed to reach either the 9- or 3-o’clock position. The arm of the PL guide is inserted in the AL portal and positioned at either 9 o’clock or 3 o’clock on the medial wall of the lateral condyle while the handle is maneuvered at the area of the junction of the distal femur and lateral condyle to fix the entry point for the tunnel. A guidewire is inserted from the outside, which is followed by a 4.5-mm cannulated drill to prepare the pilot hole. Once the length of this hole is measured, a 6-mm PL tunnel with its appropriate depth is drilled.
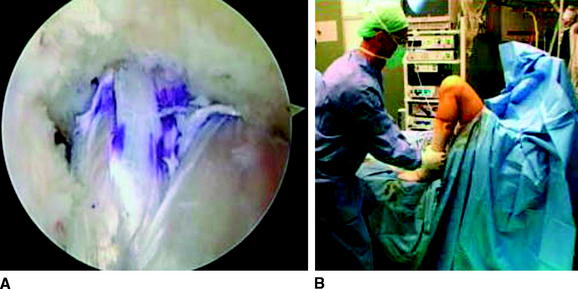
Once the femoral and tibial tunnels are completed, the 6-mm graft is placed inside the PL tunnel and locked in position with an Endobutton. This is then followed by the placement of the 7-mm graft in the AM tunnel (Fig. 24-3). The fixation of both grafts are double-checked to determine whether they are securely anchored against the femoral cortex. At this time, it is also possible to arthroscopically check the grafts for impingement.
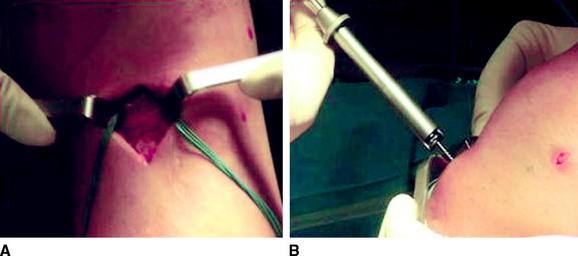
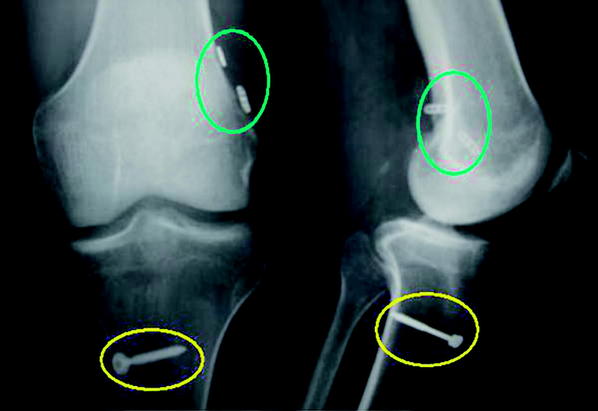
With the femoral end of the grafts securely positioned, fixation on the tibial end is achieved using a single screw-post construct. This simple construct allows fixation of the two bundles at the prescribed angles. The AM bundle is fixed at 40 to 60 degrees of flexion while the PL bundle is fixed at full extension (Fig. 24-4).
Prior to wound closure, the knee is examined for range of motion and stability (Fig. 24-5). Postoperatively, radiographs are taken to check the position of the grafts, and the patient is started on a standard ACL rehabilitation regimen17 (Fig. 24-6).
Special Considerations
The primary concern with this DBST technique is the length of the available ST autograft. Ideally, it is preferable to have a minimum of 70 mm of graft length to have at least 20 mm of graft in the femoral and tibial tunnels and 30 mm intraarticularly. Some surgeons, however, would prefer to have a graft length of 25 mm within the femoral tunnel, whereas others have reported successful outcomes with 15 mm of the graft in contact with the tunnels.17 In our experience using DBST reconstruction, a 20-mm length of graft within the AM and PL femoral tunnels is usually sufficient. With this length, the surgeon then has the option of using a 20- or 25-mm Endobutton-CL for the AM bundle and a 15- or 20-mm Endobutton-CL for the PL bundle, considering that the average AM tunnel length ranges between 40 and 45 mm, whereas PL tunnel length usually ranges from 35 to 40 mm.
1 Radford WJ, Amis AA. Biomechanics of a double prosthetic ligament in the anterior cruciate ligament. J Bone Joint Surg Br. 1990;72:1038-1043.
2 Adachi N, Ochi M, Uchio Y, et al. Reconstruction of the anterior cruciate ligament: single versus double multistranded hamstring tendons. J Bone Joint Surg Br. 2004;86:515-520.
3 Gobbi A, Francisco R. Anatomic double bundle ACL reconstruction with the semitendinosus tendon. Presented at the Multi Media Education Center of the 73rd American Academy of Orthopaedic Surgeons Annual Meeting, March 22–26, 2006, Chicago. 2006.
4 Makihara Y, Nishino A, Fukubayashi T, et al. Decrease of knee flexion torque in patients with ACL reconstruction: combined analysis of the architecture and function of the knee flexor muscles. Knee Surg Sports Traumatol Arthrosc. 2006;14:310-317.
5 Tashman S, Colon D, Anderson K, et al. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:975-983.
6 Yagi M, Wong E, Kanamori A, et al. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2000;28:660-666.
7 Yasuda K, Koga H, Morito T, et al. A retrospective study of the midterm outcome of two-bundle anterior cruciate ligament reconstruction using quadrupled semitendinosus tendon in comparison with one-bundle reconstruction. Arthroscopy. 2006;22:252-258.
8 Yasuda K, Kondo E, Ichiyama H, et al. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparison among different procedures. Arthroscopy. 2006;22:240-251.
9 Hamada M, Shino K, Horibe S, et al. Single versus bi-socket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with Endobutton femoral fixation: a prospective study. Arthroscopy. 2001;17:801-807.
10 Muneta T, Sekiya I, Yagishita K, et al. Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with Endobutton: operative technique and preliminary results. Arthroscopy. 1999;15:618-624.
11 Gobbi A, Domzalski K, Pascual J, et al. Hamstring anterior cruciate ligament reconstruction: is it necessary to sacrifice the gracilis? Arthroscopy. 2005;21:275-280.
12 Woo S. News in biomechanics research on ACL. Presented at the 8th International Conference on Orthopaedics, Biomechanics, and Sports Rehabilitation, Nov 19–21, 2004, Assisi, Italy. 2004.
13 Mae T, Shino K, Matsumoto N, et al. Force sharing between two grafts in the anatomical two-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;6:1-5.
14 Yamamoto Y, Hsu W-H, Woo SL-Y, et al. Knee stability and graft function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:1825-1832.
15 Chen L, Cooley V, Rosenberg T. ACL reconstruction with hamstring tendon. Orthop Clin North Am. 2003;34:9-18.
16 Gobbi A, Mahajan S, Tuy B, et al. Hamstring graft tibial fixation: biomechanical properties of different linkage systems. Knee Surg Sports Traumatol Arthrosc. 2002;10:330-334.
17 Rosenberg TD, Graft B. Techniques for ACL reconstruction with multi-trac drill guide. Mansfield, MA: Acufex Microsurgical, 1994.