Chapter 22 Anatomical Double-Bundle Anterior Cruciate Ligament Reconstruction Procedure Using the Semitendinosus and Gracilis Tendons
Introduction
The anterior cruciate ligament (ACL) is composed of the anteromedial bundle (AMB) and the posterolateral bundle (PLB), each with a different function.1–3 Since 2000, the author has reported the surgical principle4 and the latest procedure5 for an anatomical double-bundle ACL reconstruction that is intended to anatomically reconstruct the AMB and the PLB. In addition, the author’s team reported a prospective cohort study to evaluate this anatomical double-bundle procedure in comparison with single-bundle and nonanatomical double-bundle ACL reconstruction procedures using hamstring tendon grafts.6 Our procedure has several noteworthy characteristics. First, all four ends of two tendon grafts are grafted at the center of the anatomical attachment of the AMB or the PLB, not only on the femur but also on the tibia. Second, we use the transtibial tunnel technique to create femoral tunnels. Third, we use the hamstring tendon-hybrid graft,7,8 in which the femoral end is connected with an Endobutton CL and the tibial end is connected with a polyester tape. Fourth, we fix the polyester tape portion of the graft onto the tibia with two staples at 10 degrees of knee flexion, simultaneously applying a 30N load to each graft. In this chapter, the surgical principle and the procedure of our anatomical double-bundle ACL reconstruction are explained.
Procedure
Creation of Tibial Tunnels
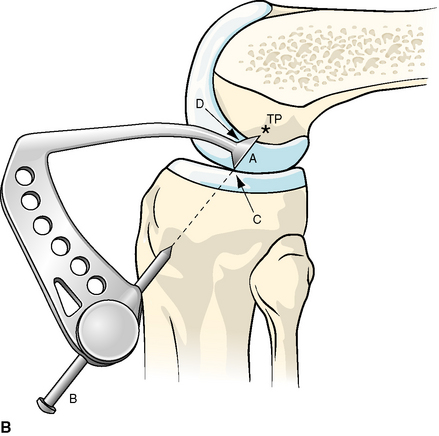
In ACL reconstruction procedures with the transtibial tunnel technique, the greatest key to success is to create a tibial tunnel with an appropriate three-dimensional (3D) direction. In other words, a tibial tunnel should be created so that a guidewire for femoral tunnel creation can be easily inserted at a targeted point on the lateral condyle through the tibial tunnel. To create such a tibial tunnel, we use a specially designed wire guide, called a wire navigator (Fig. 22-1, A), which was developed in our previous study.7,8 This device is composed of a navi-tip and a wire sleeve. The navi-tip consists of sharp tibial and femoral indicators. The axis of the wire sleeve passes through the tip of the tibial indicator (Fig. 22-1, B). First, a tibial tunnel for the PLB is created. The navi-tip is introduced into the joint cavity through the medial infrapatellar portal. The surgeon holds the tibia at 90 degrees of knee flexion, keeping the femur horizontal. The tibial indicator of the navi-tip is placed at the center of the PLB footprint on the tibia, which is located at the most posterior aspect of the area between the tibial eminences and 5 mm anterior to the posterior cruciate ligament (Fig. 22-2). Keeping the tibial indicator on this point, we aim the femoral indicator at the center of the PLB footprint on the femur (Fig. 22-3, A), which is precisely explained in the next section, and the proximal end of the extraarticularly located wire sleeve is fixed on the anteromedial aspect of the tibia through the skin incision made for the graft harvest. The proximal end and the direction of the wire sleeve are automatically determined depending on the direction of the intraarticular navi-tip (see Fig. 22-1, B). A Kirschner wire of 2 mm in diameter is drilled through the sleeve in the tibia. According to our basic studies, this tunnel does not injure this ligament because the insertion point of the wire on the anteromedial aspect of the tibia is located several millimeters anterior to the medial collateral ligament.4 The first tunnel is made with an approximately 6-mm cannulated drill corresponding to the measured diameter of the prepared substitute.
Next, a Kirschner wire for the AMB reconstruction is drilled using the same wire navigator. The tibial indicator is placed at the center of the tibial footprint of the AMB, which is located at a point approximately 7 mm anterior to the center of the first tunnel (see Fig. 22-2). Keeping the tibial indicator on this point, we then aim the femoral indicator at the center of the femoral footprint of the AMB (Fig. 22-3, B). The wire sleeve is fixed on the anteromedial cortex of the tibia. A Kirschner wire is then drilled through the sleeve in the tibia. The knee should be extended to ensure that the tip of the second wire is located at a point 5 mm posterior to the anterior edge of the roof in the intercondylar notch. The second tunnel is drilled with an approximately 7-mm cannulated drill corresponding to the measured diameter of the prepared substitute. Subsequently, two intraarticular outlets are aligned in the sagittal plane (see Fig. 22-2).
Creation of Femoral Tunnels
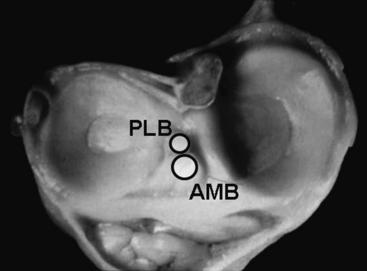
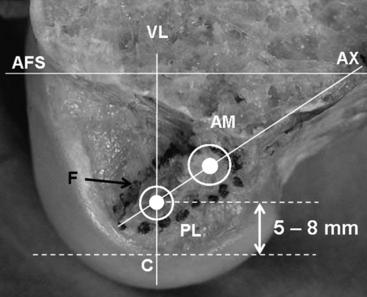
In the anatomical double-bundle procedure, it is essential to precisely understand the attachment of the main ACL fibers that should be reconstructed in ACL reconstruction. Although the normal ACL has a wide footprint on the lateral condyle,9–11 the author has found that the main ACL fiber attachment that should be reconstructed in ACL reconstruction is in the form of an egg, with its long axis inclined toward the posterior direction by 30 degrees to the long axis of the femur on the medial surface of the lateral femoral condyle4 (Fig. 22-4).
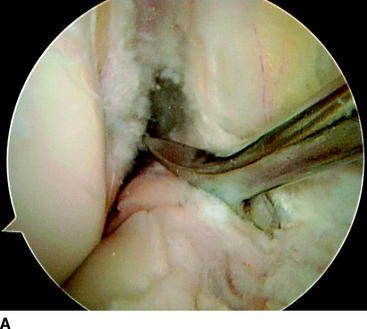
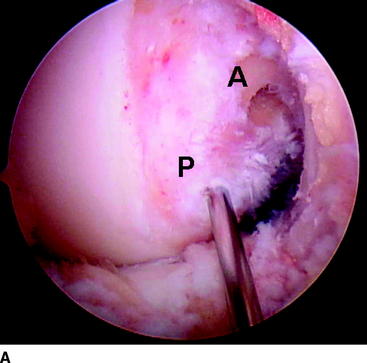
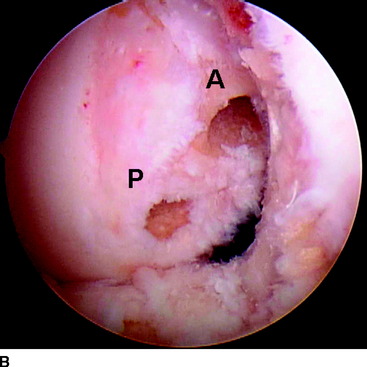
First, a Kirschner wire is drilled at the center of the femoral footprint of the AMB through the second tibial tunnel, using the offset guide system (Transtibial Femoral ACL Drill Guide, Arthrex, Naples, FL). This point is located at the point 5 to 6 mm distal from the back of the femur (see Fig. 22-4). This point is consistent with the 1:30 (or 10:30) orientation for the left (or right) knee. Using this wire as a guide, a tunnel is made with a 4.5-mm cannulated drill. The length of the tunnel is measured with a scaled probe. Then, to precisely observe the lateral condyle in the arthroscopic visual field, the portal for the arthroscope is changed to the medial infrapatellar one. We have developed a reproducible method to identify the targeted point in the arthroscopic visual field.4 When the surgeon holds the tibia at 90 degrees of knee flexion, keeping the femur horizontal, we can draw an imaginary vertical line through the contact point between the femoral condyle and the tibial plateau in the arthroscopic visual field (see Fig. 22-4). The center of the attachment of the PLB is located approximately at the crossing point between the vertical line and the long axis of the ACL attachment. Therefore, when the remnant of the ACL is observed on the lateral condyle, this point can be easily determined. If the remnant of the ACL is not identified on the lateral condyle, the center of the attachment of the PLB can be determined as the point 5 to 8 mm anterior to the edge of the joint cartilage on the imaginary vertical line (see Fig. 22-4). The femoral tunnel that has been created already for the AMB reconstruction can be used as a good landmark to determine the center of the attachment of the PLB. To insert a guidewire at this point, the surgeon manually holds a Kirschner wire and aims it at the center of the attachment of the PLB on the femur through the tibial tunnel, keeping the femur horizontal at 90 degrees of knee flexion. Then the surgeon lightly hammers the wire into this point and drills it (Fig. 22-5, A). A 4.5-mm diameter tunnel is drilled using this wire as a guide. Our cadaveric study showed that this technique provides some benefits for Endobutton fixation, including easy passage of the graft and easy flip of an Endobutton.4 The tunnel length is measured in the same manner.
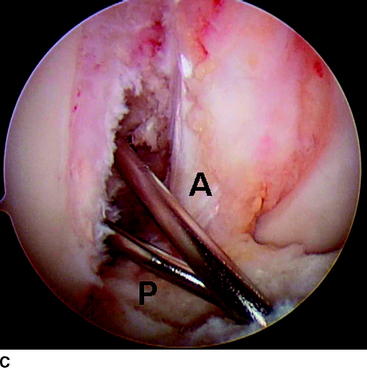
Finally, two sockets are created for the AMB and PLB reconstruction with cannulated drills in the Endobutton fixation system (Acufex Microsurgical, Mansfield, MA), the diameter of which is matched to the two grafts prepared with the technique described in the following section. Thus, two tunnels are created inside the ACL remnant on the lateral condyle (Fig. 22-5, B). The different directions of the two pairs of tunnels are demonstrated by inserting two wires through the tibial tunnel to the femoral tunnel at 90 degrees of knee flexion (Fig. 22-5, C).
Graft Fashioning
The harvested semitendinosus is cut in half. Regarding the gracilis tendon, both ends are resected so that the thickest portion is used for the graft, and the length is matched to half the length of the semitendinosus tendon. One-half of the semitendinosus tendon and the resected gracilis tendon are doubled and used for AMB reconstruction. The remaining half of the semitendinosus tendon is also doubled and used for the PLB reconstruction. Using these tendon materials, the hybrid grafts are fashioned (Fig. 22-6). At the looped end of each doubled tendon graft, an Endobutton-CL (Acufex Microsurgical, Mansfield, MA) is attached. The length of the Endobutton-CL is determined such that a 15- to 20-mm long tendon portion can be placed within the bone tunnel. A commercially available polyester tape (Leeds-Keio Artificial Ligament, Neoligament, Leeds, United Kingdom) is mechanically connected in series with the other end of the doubled tendons, using the original technique5 (see Fig. 22-6). This tape is strong, soft, meshed, 10 mm wide, and 15 cm long. In our experience, the diameter of the tendon portion ranges from 6 to 8 mm for the AMB graft and from 5 to 6 mm for the PLB graft. The first advantage of the hybrid graft is that it is stronger and stiffer than the tendon-suture composite.12,13 The second advantage is that the tape portions of the two grafts can be simultaneously fixed to the tibia with an initial tension.The latter feature is specifically important for anatomical double-bundle reconstruction.
Graft Placement
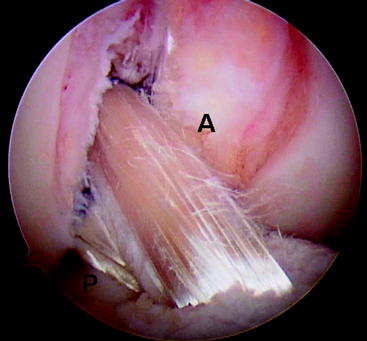
The graft for the PLB reconstruction is introduced through the tibial tunnel to the femoral tunnel using a passing pin and is fixed on the femur by an Endobutton. Then the graft for the AMB is placed in the same manner. Thus, the two bundles having different directions are intraarticularly grafted (Fig. 22-7). The grafts rarely impinge to the femur. Notchplasty is performed only in knees with an extremely narrow notch due to osteochondral spar formation or a similar problem.
Graft Tensioning and Fixation
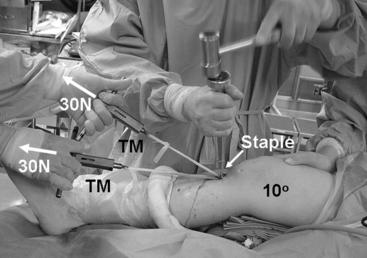
For graft fixation, the knee is flexed to 10 degrees with a sterilized thin pillow placed beneath the thigh, keeping the heel in contact with the operating table (Fig. 22-8). A spring tensiometer (Meira, Nagoya, Japan) is attached at each end of the polyester tape portion of the graft. An assistant surgeon simultaneously applies tension of 30N to each graft for 2 minutes at 10 degrees of knee flexion, and a surgeon simultaneously secures the two tape portions onto the anteromedial aspect of the tibia using two spiked staples in the turn-buckle fashion.5
The mechanism of our tensioning technique is explained as follows14: According to our in vivo measurement studies, when we applied the same initial tension on each bundle at 10 degrees of knee flexion, each tension pattern was similar to that of the normal bundle. This fact suggested that the slight flexion position (10 degrees of knee flexion) is recommended as the most appropriate knee flexion angle for easy graft tensioning. On the other hand, the full extension position may be clinically recommended to avoid flexion contracture of the knee after surgery. However, our previous studies13,15 showed that the initial graft tension in the hamstring tendon graft was dramatically reduced in the early phase after surgery. Therefore, the slight flexion position is again recommended as the most appropriate knee flexion angle for graft tensioning, when we take into account the postoperative graft relaxation. Another important question about graft tensioning is whether we should separately fix the two grafts at different flexion angles. According to our in vivo measurement studies, if we apply a tension to the AMB after fixing the PLB at the extension position, the initial tension applied to the PLB is reduced to an unknown degree. A surgeon cannot sufficiently control the graft tension in this technique. Therefore, in anatomical double-bundle ACL reconstruction, it is important to simultaneously fix the two bundles, applying appropriate initial tensions to the two grafts.
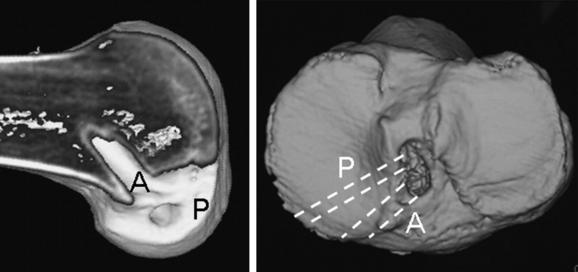
Postoperative 3D computed tomography shows that each tunnel outlet was created at the center of the anatomical attachment of the AMB or the PLB (Fig. 22-9).
Clinical Results
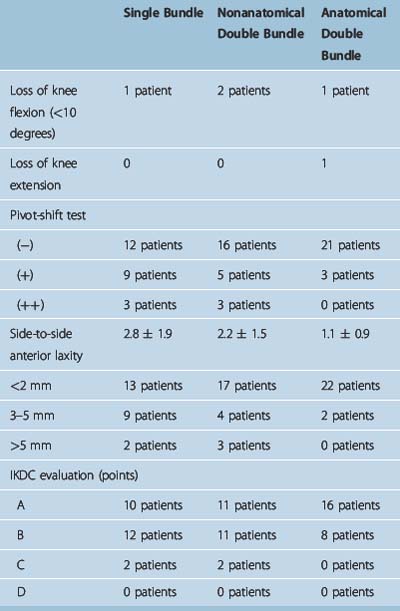
A prospective comparative cohort study was carried out with 72 consecutive patients with chronic ACL deficiency to compare three ACL reconstruction procedures using hamstring tendon grafts.6 The first 24 patients underwent a single-bundle procedure using a six-strand hamstring tendon graft. The next 24 patients underwent a nonanatomical double-bundle procedure using four-strand and two-strand hamstring tendon grafts. The final 24 patients underwent the anatomical double-bundle procedure using the same four-strand and two-strand hamstring tendon grafts. All 72 patients underwent postoperative management with the same rehabilitation protocol.6 There were no significant differences among the background factors. The postoperative anterior laxity measured with the KT-2000 was significantly less after the anatomical double-bundle reconstruction than after the single-bundle reconstruction. Concerning the results of the pivot-shift test, the anatomical double-bundle reconstruction was significantly better than the single-bundle reconstruction, although this test was not an objective evaluation (Table 22-1). In the International Knee Documentation Committee (IKDC) evaluation, the anatomical double-bundle reconstruction clinically tended to be superior to the single-bundle reconstruction, although no statistical significance could be calculated. There were no significant differences in the range of knee motion and the muscle torque. Thus, this study demonstrated that the anatomical double-bundle ACL reconstruction with the hamstring tendons was clinically useful in the treatment for the ACL deficient knee. In addition, this study also showed that in ACL reconstruction with the hamstring tendons, the anatomical double-bundle procedure was superior to the single-bundle procedure, at least in terms of restoration of the anterior and rotational knee stability as measured with the KT-2000 and pivot-shift examinations.
We should consider reasons why the results concerning knee stability are superior in the anatomical double-bundle reconstruction in our clinical study compared with the single-bundle reconstruction. Yagi et al16 reported that anatomical double-bundle reconstruction restores knee kinematics closer to normal than does single-bundle reconstruction. Namely, under a 134N anterior tibial load, anterior tibial translation for the anatomical reconstruction was significantly similar to that of the intact knee than was the single-bundle reconstruction. The in situ force in the ACL reconstructed with the anatomical double-bundle procedure averaged 97% of that in the normal ACL, whereas the force in the ACL reconstructed with the single-bundle procedure averaged only 89%. Therefore we can make the following speculations: First, the reconstructed PLB as well as the reconstructed AMB may be effective to reduce the anterior translation of the tibia in the range of less than 30 degrees. Second, excessively overloading to one bundle can be avoided during the remodeling phase, resulting in good maturation of not only the PLB graft but also the AMB graft. The good maturation of the AMB graft might result in the reduction of the anterior tibial translation at 90 degrees as well as 30 degrees. Third, the graft surface area of the two thin tendon grafts used in the anatomical procedure was greater than the area of the one thick graft used in the single-bundle procedure. Therefore, concerning graft anchoring and revascularization, the two thin bundles in the double-bundle reconstruction may be superior to the one thick bundle in the single-bundle reconstruction, resulting in the reduction of the anterior tibial translation at 30 and 90 degrees of knee flexion.
Thus, there is a high possibility that the anatomical double-bundle ACL reconstruction with the hamstring tendons is clinically useful in the treatment for the ACL deficient knee. However, there are some limitations in our clinical study.6 To establish the clinical utility of the anatomical double-bundle ACL reconstruction for the ACL deficient knee, further clinical studies are needed concerning the effects on rotatory stability, long-term survival of the graft functions, and comparisons with other procedures involving reconstruction with the bone–tendon–bone graft.
1 Kurosawa H, Yamakoshi K, Yasuda K, et al. Simultaneous measurement of changes in length of the cruciate ligaments during knee motion. Clin Orthop. 1991;265:233-240.
2 Amis AA, Dawkins GPC. Functional anatomy of the anterior cruciate ligament. Fiber bundle actions related to ligament replacement and injuries. J Bone Joint Surg. 1991;73B:260-267.
3 Back JM, Hull ML, Patterson HA. Direct measurement of strain in the posterolateral bundle of the anterior cruciate ligament. J Biomechanics. 1997;30:281-283.
4 Yasuda K, Kondo E, Ichiyama H, et al. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Anatomic and clinical studies. Arthroscopy. 2004;20:1015-1025.
5 Yasuda K, Kondo E, Ichiyama H, et al. Surgical and biomechanical concept of anatomic anterior cruciate ligament reconstruction. Oper Tech Orthop. 2005;25:96-102.
6 Yasuda K, Kondo E, Ichiyama H, et al. Anatomic double-bundle reconstruction of the anterior cruciate ligament. Comparisons with non-anatomic single- and double-bundle reconstructions. Arthroscopy. 2006;22:240-251.
7 Yasuda K, Tsujino J, Ohkoshi Y, et al. Graft site morbidity with autogenous semitendinosus and gracilis tendons. Am J Sports Med. 1995;23:706-714.
8 Yasuda K, Tsujino J, Tanabe Y, et al. Effects of initial graft tension on clinical outcome after anterior cruciate ligament reconstruction. Autogenous doubled hamstring tendons connected in series with polyester tapes. Am J Sports Med. 1997;25:99-106.
9 Girgis FG, Marshall JL, Monajem ARS. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop. 1975;106:216-231.
10 Dodds JA, Arnoczky SP. Anatomy of the anterior cruciate ligament: a blueprint for repair and reconstruction. Arthroscopy. 1994;10:132-139.
11 Harner CD, Baek GH, Vogrin TM, et al. Quantitative analysis of human cruciate ligament insertions. Arthroscopy. 1999;15:741-749.
12 Miyata K, Yasuda K, Kondo E, et al. Biomechanical comparisons of anterior cruciate ligament reconstruction procedures with flexor tendon graft. J Orthop Sci. 2000;5:585-592.
13 Yamanaka M, Yasuda K, Nakano H, et al. The effect of cyclic displacement upon the biomechanical characteristics of anterior cruciate ligament reconstructions. Am J Sports Med. 1999;27:772-777.
14 Yasuda K. Author reply to “Letter to editor” on “Anatomical reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Anatomical and clinical studies.”. Arthroscopy. 2005;21:639-640.
15 Numazaki H, Tohyama H, Yasuda K, et al. The effect of initial graft tension on mechanical behaviors of the femur-graft-tibia complex with anterior cruciate ligament reconstruction during cyclic loading. Am J Sports Med. 2002;30:800-805.
16 Yagi M, Wong EK, Kanamori A, et al. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:660-666.