Anaphylactic and anaphylactoid reactions
Pathophysiology
Prior sensitization or cross-sensitization to similar antigens is necessary to activate an anaphylactic reaction. Antigen-antibody interaction links two IgE molecules that, in turn, bind to and initiate mast cell and basophil degranulation and release of vasoactive mediators, including histamine, serum proteases (such as tryptase), proteoglycans, prostaglandins, and leukotrienes (Figure 246-1).
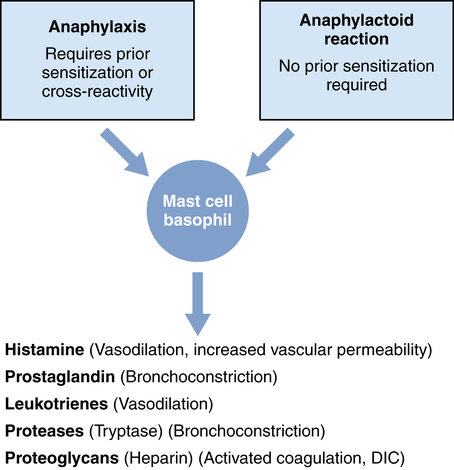
During anaphylactoid reactions, administered medications may cause nonimmunologic mast cell and basophil degranulation by activation of the complement cascade, of the coagulation system, of the kinin-generating system, or of the fibrinolytic system or by direct nonspecific mechanisms (Figure 246-1).
Clinical presentation
Target organs include the skin, upper and lower respiratory tracts, cardiovascular system, hematologic system, and the gastrointestinal tract (Box 246-1); mental status may also be altered. The signs and symptoms of anaphylaxis and anaphylactoid reactions that occur during the perioperative period depend on the types of anesthesia and monitors used. For example, early skin changes may not be appreciated in a covered patient, whereas abdominal and neurologic signs may be apparent only in awake patients.





