Anaesthesia for Orthopaedic Surgery
One in five operations in the United Kingdom is for orthopaedic, spinal or trauma surgery. Anaesthesia for trauma surgery is discussed in Chapter 37. This chapter provides a framework for the conduct of anaesthesia for orthopaedic surgery.
THE PATIENT POPULATION
Concurrent Drug Therapy
Many young healthy patients presenting for orthopaedic surgery do not take concurrent medication. However, use of analgesics is very common in the orthopaedic population because of the painful nature of their disease process. Concurrent therapy with antihypertensive, antianginal, antidepressant or cholesterol-lowering medication is common in older patients presenting for orthopaedic surgery. These patients often present for arthroplasty and this major procedure may place significant demands upon their physiological reserves. Preparation of the patient taking these drugs is discussed in detail in Chapter 18. Patients may also be using orthopaedic disease-modifying drugs such as methotrexate, steroids and gold.
TECHNIQUES OF ANAESTHESIA
Regional Anaesthesia
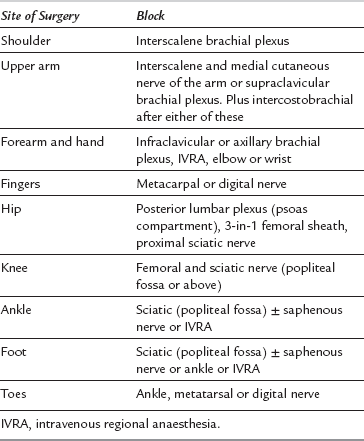
Peripheral nerve block is commonly used as a sole technique for many procedures, with the advantages of excellent pain relief, reduction of surgical stress, avoidance of complications of general anaesthesia and earlier discharge in the day-case setting. Peripheral surgery in ‘high-risk’ patients may also be carried out under peripheral nerve block to avoid the potential complications of general anaesthesia or central neuraxial block. Patients report a high degree of satisfaction following surgery carried out using this form of anaesthesia. Table 28.1 shows the sites at which surgery may be performed in association with specific nerve blocks. This form of anaesthesia requires a high level of expertise and an understanding of the issues of managing a conscious patient during surgery.
Intravenous regional anaesthesia (IVRA) is suitable for manipulation of fractures and brief operations (less than 30 min) on the forearm and lower leg. It is technically easy to perform but fatalities have occurred as a result of a large dose of local anaesthetic reaching the systemic circulation. Before performing IVRA, it is essential to understand how the risk of complications may be minimized and how they may be treated if they occur. Details of the technique and safety precautions are described in Chapter 24.
POSTOPERATIVE ANALGESIA
Central Neuraxial Drugs
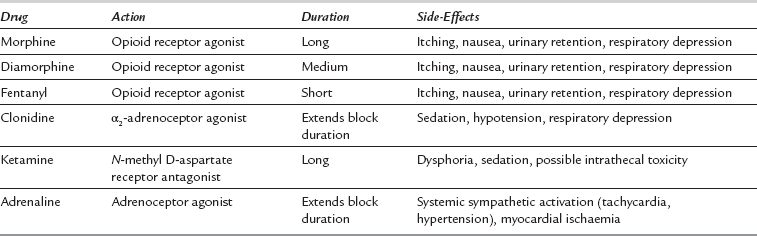
Single-dose spinal or epidural anaesthesia using local anaesthetic alone usually provides analgesia for only a relatively short period of time after operation. An adjuvant administered into the intrathecal or epidural space with the local anaesthetic improves the quality of the block and extends the duration of analgesia. Table 28.2 describes some of the more commonly administered drugs.
Peripheral Nerve Blocks
Nerve injury due to peripheral nerve block is rare (see Ch 43); it occurs in 1:5000 to 1:10 000 blocks performed, and patients with concurrent comorbidity, such as diabetes or vascular disease, may have an increased risk. However, the incidence of nerve injury secondary to orthopaedic surgery (direct trauma, tourniquet or positioning) is more frequent and often occurs in the sensory distribution of the nerve block. This reduces the popularity of peripheral nerve blocks in some institutions lest the block is blamed for nerve damage.
SURGICAL CONSIDERATIONS
Some positions adopted during orthopaedic surgery are associated with venous air embolism. These postures include the lateral position for hip surgery, the sitting position for shoulder surgery and the prone position for spinal surgery. Monitoring for, and treatment of, air embolism are discussed in detail in Chapter 43.
Prophylaxis Against Hypothermia
Following induction of general or regional anaesthesia, heat is redistributed from the core to the peripheries. Following induction of general anaesthesia, there is typically a reduction in core temperature of 1°C in the first 30 min of anaesthesia. Core temperature reduces more slowly after this initial redistribution phase, typically by approximately 0.5°C per hour, although the rate of fall is heavily dependent upon ambient temperature, exposure and insulation, and the use of warming devices (see Ch 11).
Prophylaxis Against Thromboembolism
Deep venous thrombosis (DVT) may complicate any surgery, but is associated particularly with surgery involving the pelvis, hip and knee. Pulmonary embolism (PE) may be fatal and accounts for 50% of all deaths after surgery for hip replacement. Although an infusion of dextran has been shown to reduce the incidence of PE after surgery, there is a relatively high risk of anaphylaxis associated with its administration, and low-dose heparin regimens have become the norm. There is evidence that heparin reduces the incidence of fatal PE in high-risk groups, including patients who undergo surgery on the pelvis, hip or knee. Compared with unfractionated heparins (UFH), low molecular weight heparins (LMWH) inhibit the coagulation enzyme Xa and bind antithrombin-3 to a similar extent, but bind less to thrombin. The use of LMWH might be expected to result in less surgical bleeding than when UFH is used. LMWH probably protects better against DVT after hip replacement but the evidence for better prophylaxis against PE is less firm. The simplicity of once-daily administration of LMWH is an added advantage compared with UFH. Newer oral agents have the potential to provide patients with an even simpler postoperative prophylaxis treatment. This topic is discussed in detail in Chapter 13.
Blood Conservation
Cell Salvage
 Salvage and retransfusion of blood from a wound containing malignant cells is contraindicated because of the risk of dissemination of tumour cells. Malignant cells are incompletely removed by washing and filtration.
Salvage and retransfusion of blood from a wound containing malignant cells is contraindicated because of the risk of dissemination of tumour cells. Malignant cells are incompletely removed by washing and filtration.
 Contamination with bowel contents or infection at the site of blood retrieval is a contraindication to salvage and retransfusion. Washing with antibiotic solutions has been shown to be ineffective in neutralizing all bacteria.
Contamination with bowel contents or infection at the site of blood retrieval is a contraindication to salvage and retransfusion. Washing with antibiotic solutions has been shown to be ineffective in neutralizing all bacteria.
 Salvaged blood which contains topical haemostatic agents such as collagen, cellulose, gelatin and thrombin should not be retransfused as it may result in intravascular coagulation.
Salvaged blood which contains topical haemostatic agents such as collagen, cellulose, gelatin and thrombin should not be retransfused as it may result in intravascular coagulation.
 Salvaged blood which contains surgical irrigants, liquid methylmethacrylate or antibiotics not licensed for parenteral use (e.g. neomycin) should not be retransfused.
Salvaged blood which contains surgical irrigants, liquid methylmethacrylate or antibiotics not licensed for parenteral use (e.g. neomycin) should not be retransfused.
SPECIFIC SURGICAL PROCEDURES
Auroy, Y., Narchi, P., Messiah, A., et al. Serious complications related to regional anesthesia: results of a prospective survey in France. Anesthesiology. 1997;87:479–486.
British Medical Association and Royal Pharmaceutical Society. Cautions and contra-indications of corticosteroids. In: British National Formulary, June 2013. http://www.medicinescomplete.com/mc/
Singelyn, F.J., Deyaert, M., Joris, D., et al. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth. Analg. 1998;87:88–92.