Chapter 19 Anaesthesia and neuromuscular block
General anaesthesia
Until the mid-19th century such surgery as was possible had to be undertaken at tremendous speed. Surgeons did their best for terrified patients by using alcohol, opium, cannabis, hemlock or hyoscine.1 With the introduction of general anaesthesia, surgeons could operate for the first time with careful deliberation. The problem of inducing quick, safe and easily reversible unconsciousness for any desired length of time in humans began to be solved only in the 1840s when the long-known substances nitrous oxide, ether and chloroform were introduced in rapid succession.
• 1842 – W E Clarke of Rochester, New York, administered ether for a dental extraction; however, the event was not made widely known at the time.
• 1844 – Horace Wells, a dentist in Hartford, Connecticut, introduced nitrous oxide to produce anaesthesia during dental extraction.
• 1846 – On 16 October William Morton, a Boston dentist, successfully demonstrated the anaesthetic properties of ether.
• 1846 – On 21 December Robert Liston performed the first surgical operation in England under ether anaesthesia.2
• 1847 – James Y Simpson, professor of midwifery at the University of Edinburgh, introduced chloroform for the relief of labour pain.
The next important developments in anaesthesia were in the 20th century when the appearance of new drugs, both as primary general anaesthetics and as adjuvants (muscle relaxants), new apparatus and clinical expertise in rendering prolonged anaesthesia safe enabled surgeons to increase their range. No longer was the duration and type of surgery determined by patients’ capacity to endure pain.
Phases of general anaesthesia
Before surgery,
All of these may influence the choice of anaesthetic technique and anaesthetic drugs.
Before surgery (premedication)
During surgery
Induction
1. Usually intravenous: pre-oxygenation followed by a small dose of an opioid, e.g. fentanyl or alfentanil to provide analgesia and sedation, followed by propofol or, less commonly, thiopental, etomidate or ketamine to induce anaesthesia. Airway patency is maintained with a supraglottic airway device (e.g. laryngeal mask airway (LMA)), a tracheal tube or, for very short procedures, an oral airway and facemask. Insertion of a tracheal tube usually requires paralysis with a neuromuscular blocker and is undertaken if there is a risk of pulmonary aspiration from regurgitated gastric contents or from blood.
2. Inhalational induction, usually with sevoflurane, is undertaken less commonly. It is used in children, particularly if intravenous access is difficult, and in patients at risk from upper airway obstruction.
Maintenance
1. Most commonly with oxygen and air, or nitrous oxide and oxygen, plus a volatile agent, e.g. sevoflurane, desflurane or isoflurane. Additional doses of a neuromuscular blocker or opioid are given as required.
2. A continuous intravenous infusion of propofol can be used to maintain anaesthesia. This technique of total intravenous anaesthesia is relatively common because the quality of recovery may be better than after inhalational anaesthesia. The propofol infusion is often combined with an infusion of remifentanil, an ultra-short-acting opioid.
When appropriate, peripheral nerve block with a local anaesthetic, or neural axis block, e.g. spinal or epidural, provides intraoperative analgesia and muscle relaxation. These local anaesthetic techniques provide excellent postoperative analgesia.
Some special techniques
Dissociative anaesthesia
is a state of profound analgesia and anterograde amnesia with minimal hypnosis during which the eyes may remain open; it can be produced by ketamine (see p. 301). It is particularly useful where modern equipment is lacking or where access to the patient is limited, e.g. in prehospital or military settings.
Sedation and amnesia
without analgesia is provided by intravenous midazolam or, less commonly nowadays, by diazepam. These drugs can be used alone for procedures causing mild discomfort, e.g. endoscopy, and with a local anaesthetic where more pain is expected, e.g. removal of impacted wisdom teeth. Benzodiazepines produce anterograde, but not retrograde, amnesia. By definition, the sedated patient remains responsive and cooperative. (For a general account of benzodiazepines and the competitive antagonist flumazenil, see Ch. 20.)
Inhalation anaesthetics
Nitrous oxide
Halogenated anaesthetics
Halothane
Halothane has the highest blood/gas partition coefficient of the volatile anaesthetic agents and recovery from halothane anaesthesia is comparatively slow. It is pleasant to breathe. Halothane reduces cardiac output more than any of the other volatile anaesthetics. It sensitises the heart to the arrhythmic effects of catecholamines and hypercapnia; arrhythmias are common, in particular atrioventricular dissociation, nodal rhythm and ventricular extrasystoles. Halothane can trigger malignant hyperthermia in those who are genetically predisposed (see p. 309).
Intravenous anaesthetics
Pharmacokinetics
Intravenous anaesthetics enable an extremely rapid induction because the blood concentration can be raised quickly, establishing a steep concentration gradient and expediting diffusion into the brain. The rate of transfer depends on the lipid solubility and arterial concentration of the unbound, non-ionised fraction of the drug. After a single induction dose of an intravenous anaesthetic, recovery occurs quite rapidly as the drug is redistributed around the body and the plasma concentration reduces. Recovery from a single dose of intravenous anaesthetic is thus dependent on redistribution rather than rate of metabolic breakdown. With the exception of propofol, repeated doses or infusions of intravenous anaesthetics will cause considerable accumulation and prolong recovery. Attempts to use thiopental as the sole anaesthetic in war casualties led to it being described as an ideal form of euthanasia.3
Thiopental
Thiopental is a very short-acting barbiturate4 that induces anaesthesia smoothly, within one arm-to-brain circulation time. The typical induction dose is 3–5 mg/kg. Rapid distribution (initial t½ 4 min) allows swift recovery after a single dose. The terminal t½ of thiopental is 11 h and repeated doses or continuous infusion lead to significant accumulation in fat and very prolonged recovery. Thiopental is metabolised in the liver. The incidence of nausea and vomiting after thiopental is slightly higher than that after propofol. The pH of thiopental is 11 and extravasation causes considerable local damage. Accidental intra-arterial injection will also cause serious injury distal to the injection site.
Ketamine
Ketamine is a phencyclidine (hallucinogen) derivative and an antagonist of the NMDA receptor.5 In anaesthetic doses it produces a trance-like state known as dissociative anaesthesia (sedation, amnesia, dissociation, analgesia).
Muscle relaxants
Neuromuscular blocking drugs
Neuromuscular blocking drugs first attracted scientific notice because of their use as arrow poisons by the natives of South America, who used the most famous of all, curare, for killing food animals6 as well as enemies. In 1811 Sir Benjamin Brodie smeared ‘woorara paste’ on wounds of guinea pigs and noted that death could be delayed by inflating the lungs through a tube introduced into the trachea. Though he did not continue until complete recovery, he did suggest that the drug might be of use in tetanus.
Drugs acting at the myoneural junction produce complete paralysis of all voluntary muscle so that movement is impossible and mechanical ventilation is needed. It is plainly important that a paralysed patient should be unconscious during surgery.7
Using modern anaesthetic techniques and monitoring, awareness while paralysed for a surgical procedure is extremely rare. In the UK, general anaesthesia using volatile agents should always be monitored with agent analysers, which measure and display the end-tidal concentration of volatile agent. Increasing use of depth of anaesthesia monitors (e.g. bispectral index (BIS), which is based on the processed electroencephalogram) should further reduce the incidence of awareness. In the past, misguided concerns about the effect of volatile anaesthetics on the newborn led many anaesthetists to use little, if any, volatile agent when giving general anaesthesia for caesarean section. Under these conditions some mothers were conscious and experienced pain while paralysed and therefore unable to move. Despite its extreme rarity nowadays,8 fear of awareness under anaesthesia is still a leading cause of anxiety in patients awaiting surgery.
Mechanisms
1. By competition with acetylcholine (atracurium, cisatracurium, mivacurium, pancuronium, rocuronium, vecuronium). These drugs are competitive antagonists of acetylcholine. They do not cause depolarisation themselves but protect the endplate from depolarisation by acetylcholine. The result is a flaccid paralysis. Reversal of this type of neuromuscular block can be achieved with anticholinesterase drugs, such as neostigmine, which prevent the destruction by cholinesterase of acetylcholine released at nerve endings, enable the concentration to build up and so reduce the competitive effect of a blocking agent. Rocuronium and vecuronium can also be reversed with the modified γ-cyclodextrin, sugammadex (see below).
2. By depolarisation of the motor endplate (suxamethonium). Such agonist drugs activate the acetylcholine receptor on the motor endplate; at their first application voluntary muscle contracts but, as they are not destroyed immediately, like acetylcholine, the depolarisation persists. It might be expected that this prolonged depolarisation would cause muscles to remain contracted, but this is not so (except in chickens). With prolonged administration, a depolarisation block changes to a competitive block (dual block). Because of the uncertainty of this situation, a competitive blocking drug is preferred for anything other than short procedures.
Competitive antagonists
Antagonism of competitive neuromuscular block
Neostigmine
The action of competitive acetylcholine blockers is antagonised by anticholinesterase drugs, which enable accumulation of acetylcholine. Neostigmine (see also p. 375) is given intravenously, mixed with glycopyrronium to prevent bradycardia caused by the parasympathetic autonomic effects of the neostigmine. It acts in 4 min and its effects last for about 30 min. Too much neostigmine can cause neuromuscular block by depolarisation, which will cause confusion unless there have been some signs of recovery before neostigmine is given. Progress can be monitored with a nerve stimulator.
Depolarising neuromuscular blocker
Suxamethonium (succinylcholine)
Suxamethonium is destroyed by plasma pseudocholinesterase and so its persistence in the body is increased by neostigmine, which inactivates that enzyme, and in patients with hepatic disease or severe malnutrition whose plasma enzyme concentrations are lower than normal. Approximately 1 in 3000 of the European population have hereditary defects in amount or kind of enzyme, and cannot destroy the drug as rapidly as normal individuals.9 Paralysis can then last for hours and the individual requires ventilatory support and sedation until recovery occurs spontaneously.
Local anaesthetics
Pharmacokinetics
For topical effect on intact skin for needling procedures, a eutectic10 mixture of bases of prilocaine or lidocaine is used (EMLA – eutectic mixture of local anaesthetics). Absorption is very slow and a cream is applied under an occlusive dressing for at least 1 h. Tetracaine gel 4% (Ametop) is more effective than EMLA cream and enables pain-free venepuncture 30 min after application.
Other effects
Local anaesthetics also have the following clinically important effects in varying degree:
Uses
Local anaesthetics may be used in several ways to provide the following:
• Surface anaesthesia, as solution, jelly, cream or lozenge.
• Infiltration anaesthesia, to block the sensory nerve endings and small cutaneous nerves.
Regional anaesthesia
Subarachnoid (intrathecal) block (spinal anaesthesia)
Serious local neurological complications, e.g. infection and nerve injury, are extremely rare.
Opioid analgesics
are used intrathecally and extradurally. They diffuse into the spinal cord and act on its opioid receptors (see p. 282); they are highly effective in skilled hands for post-surgical and intractable pain. Respiratory depression may occur. The effect begins in 20 min and lasts for up to 12 h.
Diamorphine or other more lipid-soluble opioids, such as fentanyl, may be used.
Individual local anaesthetics
Amides
Prilocaine
is used similarly to lidocaine (t½ 1.5 h), but it is slightly less toxic. It used to be the preferred drug for intravenous regional anaesthesia but it is no longer available as a preservative-free solution and most clinicians now use lidocaine instead. Crystals of prilocaine and lidocaine base, when mixed, dissolve in one another to form a eutectic emulsion that penetrates skin and is used for dermal anaesthesia (EMLA; see p. 305), e.g. before venepuncture in children.
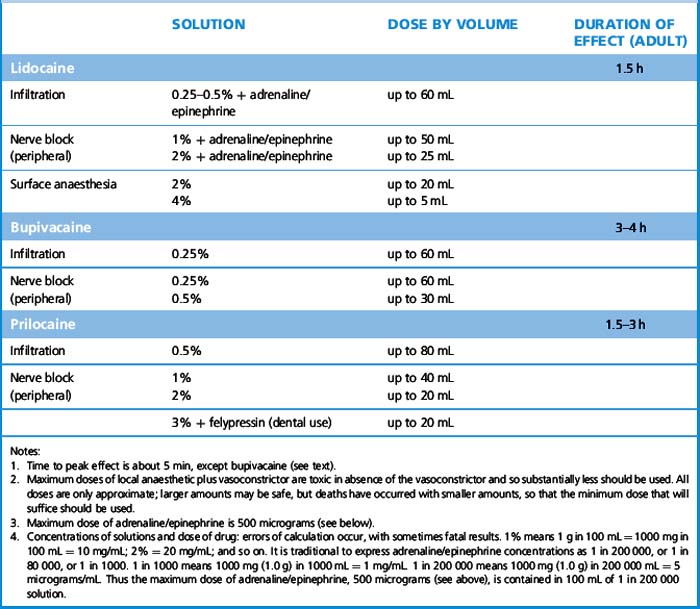
Bupivacaine
is long acting (t½ 3 h) (see Table 19.1) and is used for peripheral nerve blocks, and for epidural and spinal anaesthesia. Although onset of effect is comparable to that of lidocaine, peak effect occurs later (30 min).
Esters
Cocaine
(alkaloid) is used medicinally solely as a surface anaesthetic (for abuse toxicity, see p. 157) usually as a 4% solution, because adverse effects are both common and dangerous when it is injected. Even as a surface anaesthetic, sufficient absorption may take place to cause serious adverse effects and cases continue to be reported; only specialists should use it and the dose must be checked and restricted.
Obstetric analgesia and anaesthesia
Although this soon ceased to be considered immoral on religious grounds, it has been a technically controversial topic since 1853 when it was announced that Queen Victoria had inhaled chloroform during the birth of her eighth child. The Lancet recorded ‘intense astonishment … throughout the profession’ at this use of chloroform, ‘an agent which has unquestionably caused instantaneous death in a considerable number of cases’. But the Queen (perhaps ignorant of these risks) took a different view, writing in her private journal of ‘that blessed chloroform’ and adding that ‘the effect was soothing, quieting and delightful beyond measure’.11
General anaesthesia
during labour presents special problems. Gastric regurgitation and aspiration are a particular risk (see p. 296). The safety of the fetus must be considered; all anaesthetics and analgesics in general use cross the placenta in varying amounts and, apart from respiratory depression, produce no important effects except that high doses interfere with uterine contraction and may be followed by uterine haemorrhage. Neuromuscular blocking agents can be used safely.
Anaesthesia in patients already taking medication
Drugs that affect anaesthesia
Adrenal steroids
Chronic corticosteroid therapy with the equivalent of prednisolone 10 mg daily within the previous 3 months suppresses the hypothalamic–pituitary–adrenal (HPA) system. Without corticosteroid supplementation perioperatively the patient may fail to respond appropriately to the stress of surgery and become hypotensive (see Ch. 35).
Oral contraceptives
containing oestrogen, and post-menopausal hormone replacement therapy predispose to thromboembolism (see p. 621).
Anaesthesia in the diseased, and in particular patient groups
Malignant hyperthermia
Anaesthesia in MH-susceptible patients is achieved safely with total intravenous anaesthesia using propofol and opioids. Dantrolene for intravenous use must be available immediately in every location where general anaesthesia is given. The relation of malignant hyperthermia syndrome with neuroleptic malignant syndrome (for which dantrolene may be used as adjunctive treatment, see p. 328) is uncertain.
The elderly
(see p. 105) are liable to become confused by cerebral depressants, especially by hyoscine. Atropine also crosses the blood–brain barrier and can cause confusion in the elderly; glycopyrronium is preferable. In general, elderly patients require smaller doses of all drugs than the young. The elderly tolerate hypotension poorly; they are prone to cerebral and coronary ischaemia.
Children
(see p. 103). The problems with children are more technical, physiological and psychological than pharmacological.
Chau P.L. New insights into the molecular mechanisms of general anaesthetics. Br. J. Pharmacol.. 2010;161:288–307.
Columb M.O., Ramsaran R. Local anaesthetic agents. Anaesthesia and Intensive Care Medicine. 2010;11:113–117.
Farooq K., Hunter J.M. Neuromuscular blocking and reversal agents. Anaesthesia and Intensive Care Medicine. 2008;9:240–243.
Pandit J.J. Intravenous anaesthetic agents. Anaesthesia and Intensive Care Medicine. 2008;9:154–159.
Smith. S., Scarth E., Sasada. M. Drugs in Anaesthesia and Intensive Care, fourth ed, Oxford: Oxford University Press, 2011. ISBN 9780199599387
Sneyd J.R., Rigby-Jones A.E. New drugs and technologies, intravenous anaesthesia is on the move (again). Br. J. Anaesth.. 2010;105:246–254.
1 A Japanese pioneer in about 1800 wished to test the anaesthetic efficacy of a herbal mixture including solanaceous plants (hyoscine-type alkaloids). His elderly mother volunteered as subject as she was anyway expected to die soon. But the pioneer administered it to his wife for, ‘as all three agreed, he could find another wife, but could never get another mother’ (Journal of the American Medical Association 1966; 197:10).
2 Frederick Churchill, a butler from Harley Street, had his leg amputated at University College Hospital, London. After removing the leg in 28 s, a skill necessary to compensate for the previous lack of anaesthetics, Robert Liston turned to the watching students, and said, ‘This Yankee dodge, gentlemen, beats mesmerism hollow’. That night he anaesthetised his house surgeon in the presence of two women (Merrington W R 1976 University College Hospital and its Medical School: A History. Heinemann, London).
3 Halford J J 1943 A critique of intravenous anaesthesia in war surgery. Anesthesiology 4:67.
4 Johan Adolf Bayer discovered malonylurea (the parent compound of barbiturates) on 4 December 1863. That same day he visited a tavern patronised by artillery officers and it transpired that 4 December was also the feast day of Saint Barbara, the patron saint of artillery officers, so he named the new compound ‘barbituric acid’ (Cozanitis D A 2004 One hundred years of barbiturates and their saint. Journal of the Royal Society of Medicine 97:594–598).
6 Curare was obtained from several sources but most commonly from the vine Chondrodendron tomentosum. The explorers Humboldt and Bonpland in South America (1799–1804) reported that an extract of its bark was concentrated as a tar-like mass and used to coat arrows. The potency was designated ‘one tree’ if a monkey, struck by a coated arrow, could make only one leap before dying. A more dilute (‘three tree’) form was used to paralyse animals so that they could be captured alive – an early example of a dose–response relationship.
7 The introduction of tubocurarine into surgery made it desirable to decide once and for all whether the drug altered consciousness. Doubts were resolved in a single experiment: A normal subject was slowly paralysed (curarised) after arranging a detailed and complicated system of communication. Twelve minutes after beginning the slow infusion of curare, the subject, having artificial respiration, could move only his head. He indicated that the experience was not unpleasant, that he was mentally clear and did not want an endotracheal tube inserted. After 22 min, communication was possible only by slight movement of the left eyebrow, and after 35 min paralysis was complete and direct communication lost. An airway was inserted. The subject’s eyelids were then lifted for him and the resulting inhibition of alpha rhythm of the electroencephalogram suggested that vision and consciousness were normal. After recovery, aided by neostigmine, the subject reported that he had been mentally ‘clear as a bell’ throughout, and confirmed this by recalling what he had heard and seen. The insertion of the tracheal tube had caused only minor discomfort, perhaps because of the prevention of reflex muscle spasm. During artificial respiration he had ‘felt that (he) would give anything to be able to take one deep breath’ despite adequate oxygenation (Smith S M et al 1947 Anesthesiology 8:1). Note: a randomised controlled trial is not required for this kind of investigation.
8 In a prospective series of 11 785 general anaesthetics, 18 patients recalled awareness during surgery (Sandin R H, Enlund G, Samuelsson P et al 2000 Awareness during anaesthesia: a prospective case study. Lancet 355:707–711).
9 There are wide inter-ethnic differences. When cases are discovered the family should be investigated for low plasma cholinesterase activity and affected individuals warned.
10 A mixture of two solids that becomes a liquid because the mixture has a lower melting point than either of its components.
11 The chloroform was administered by John Snow (1813–1858) who invented the ether inhaler and first applied science to anaesthesia. This was the same John Snow who in 1854 traced the source of an outbreak of cholera to sewage contamination of a well in Soho in London. When the pump handle was removed the number of cases declined dramatically, so helping to demonstrate that cholera was a specific, water-borne disease and not a ‘miasma’ in the air.