Chapter 5 AMENORRHEA: SECONDARY
Secondary amenorrhea is the absence of menses for 3 months in women with previously normal menstruation or for 9 months in women with previous oligomenorrhea. Secondary amenorrhea is more common than primary amenorrhea. The most common cause of secondary amenorrhea is pregnancy. Thyroid disease and hyperprolactinemia are also common causes of secondary amenorrhea.
Once pregnancy, thyroid disease, and hyperprolactinemia are ruled out as potential causes (Fig. 5-1), the remaining causes of secondary amenorrhea are classified as eugonadotropic amenorrhea, hypogonadotropic hypogonadism, and hypergonadotropic hypogonadism. Outflow tract obstruction and hyperandrogenic chronic anovulation are two common causes of eugonadotropic amenorrhea. Polycystic ovary syndrome is the most common cause of hyperandrogenic chronic anovulation.
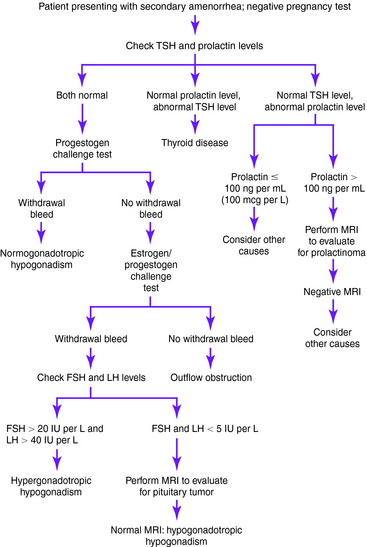
Figure 5-1. Evaluation of secondary amenorrhea.
(From Master-Hunter T, Heiman DL: Amenorrhea: evaluation and treatment. Am Fam Physician 2006;73:1374-1382.)
Causes of Secondary Amenorrhea
Key Historical Features
Key Physical Findings
✓ Height and weight compared against normative data
✓ Pubertal development according to Tanner staging
✓ Signs of an eating disorder, such as parotid gland enlargement, Russell’s sign, or dental erosions
✓ Abdominal examination for masses
✓ Pelvic examination for imperforate hymen, transverse vaginal septum, clitoral hypertrophy, or undescended testes
✓ Rectal examination for skin tags, fissures, or occult blood that may indicate inflammatory bowel disease
✓ Evaluation for striae, buffalo hump, central obesity, or proximal muscle weakness
Suggested Work-Up
| Pregnancy test | To evaluate for pregnancy |
| Prolactin level measurement | To evaluate for hyperprolactinemia |
| Thyroid-stimulating hormone (TSH) measurement | To evaluate for subclinical hypothyroidism |
| Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) measurement | If polycystic ovarian syndrome is suspected (LH/FSH ratio may be elevated) |
Additional Work-Up
| Progestogen challenge test | If prolactin and TSH levels are normal, progestogen challenge is used to help evaluate for a patent outflow tract |
| A negative progestogen challenge test result indicates an outflow tract abnormality or inadequate estrogenization | |
| Estrogen/progestogen challenge test | Used to differentiate abnormal outflow tract from inadequate estrogenization; a negative finding usually indicates an outflow tract obstruction, and a positive finding indicates an abnormality within the hypothalamic-pituitary-ovarian axis |
| Testosterone and dehydroepiandrosterone sulfate (DHEAS) measurements | If signs of androgen excess are present, these evaluations are for adrenal disease and androgen-secreting ovarian tumors |
| Estradiol level | To confirm hypoestrogenism if premature ovarian failure is suspected |
| 17-Hydroxyprogesterone measurement before and after ACTH injection | If adult-onset congenital adrenal hyperplasia is suspected |
| Measurement of urinary free cortisol and serum electrolytes | If Addison disease is suspected clinically in the setting of premature ovarian failure |
| Magnetic resonance imaging (MRI) of the sella turcica | To evaluate for pituitary tumor if the prolactin level exceeds 100 ng/mL |
| Hysterosalpingography, hysteroscopy, or sonohysterography | If Asherman syndrome is suspected in the setting of outflow tract obstruction |
Adams Hillard PJ, Deitch HR. Menstrual disorders in the college age female. Pediatr Clin North Am. 2005;52:179-197.
Kazis K, Iglesias E. The female athlete triad. Adolesc Med. 2003;14:87-95.
Kiningham RB, Apgar BS, Schwenk TL. Evaluation of amenorrhea. Am Fam Physician. 1996;53:1185-1194.
Master-Hunter T, Heiman DL. Amenorrhea: evaluation and treatment. Am Fam Physician. 2006;73:1374-1382.
Pickett CA. Diagnosis and management of pituitary tumors: recent advances. Primary Care. 2003;30:765-789.
Pletcher JR, Slap GB. Menstrual disorders: amenorrhea. Pediatr Clin North Am. 1999;46:505-518.
Speroff L, Fritz MA. Amenorrhea. In Clinical Gynecologic Endocrinology and Infertility, 7th, Philadelphia: Lippincott Williams & Wilkins; 2005:401-464.
Warren MP. Evaluation of secondary amenorrhea. J Clin Endocrinol Metab. 1996;81:437-442.




