Alternative and specialized imaging modalities
Introduction
An array of medical imaging modalities has been developed in recent years and these continue to be developed at a phenomenal rate. Totally new imaging techniques have been introduced, while the resolution and image quality of existing systems are continually being refined and improved. Research and development have focused on manipulating and altering all three of the basic requirements for image production – the patient, the image-generating equipment (to find alternatives to ionizing radiation) and the image receptor. Digital image receptors (solid-state and photostimulable phosphor plates) are now used routinely (see Ch. 4). More and more sophisticated computer software is being developed to manipulate the image itself, once it has been captured. Many of these imaging modalities are playing an increasingly important role in dentistry. As a result, clinicians need to be aware of them and their application in the head and neck region. The main specialized imaging modalities include:
This chapter provides a summary of these modalities and their main applications in the head and neck region.
Contrast studies
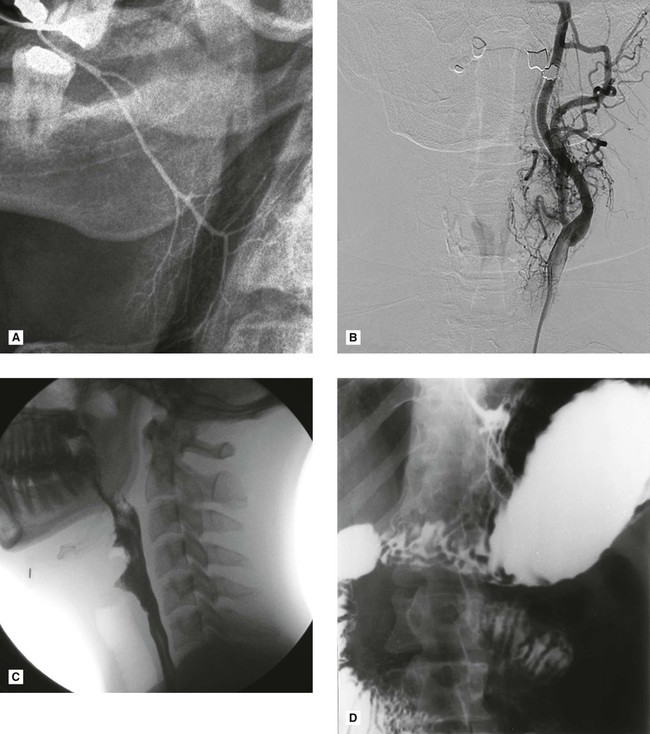
These investigations use contrast media, radiopaque substances that have been developed to alter artificially the density of different parts of the patient, so altering subject contrast – the difference in the X-ray beam transmitted through different parts of the patient’s tissues (see Ch. 17). Thus, by altering the patient, certain organs, structures and tissues, invisible using conventional means, can be seen (see Fig. 18.1). Contrast studies, and the tissues imaged, include:
• Sialography – salivary glands
• Lymphography – lymph nodes and vessels
Main contrast studies used in the head and neck
• Computed tomography – to provide general enhancement (see later)
• Barium swallow – to image the oesophagus
• Angiography – aqueous iodine-based contrast media introduced into selected blood vessels, e.g., the carotids (common, internal or external) or the vertebral arteries.
The procedure usually entails introducing a catheter into a femoral artery followed by selective catheterization of the carotid or vertebral arteries, as required, using fluoroscopic control. Once the catheter is sited correctly, the contrast medium is injected and radiographs of the appropriate area taken (see Fig. 18.1B).
Main indications for angiography in the head and neck
• To show the vascular anatomy and feeder vessels associated with haemangiomas
• To show the vascular anatomy of arteriovenous malformations
• Investigation of suspected subarachnoid haemorrhage resulting from an aneurysm in the Circle of Willis
• Investigation of transient ischaemic attacks possibly caused by emboli from atheromatous plaques in the carotid arteries.
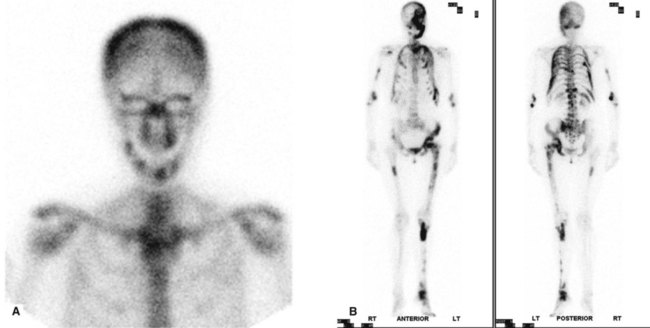
Radioisotope imaging
Radioisotope imaging relies upon altering the patient by making the tissues radioactive and the patient becoming the source of ionizing radiation. This is done by injecting certain radioactive compounds into the patient that have an affinity for particular tissues – so-called target tissues. The radioactive compounds become concentrated in the target tissue and their radiation emissions are then detected and imaged, usually using a stationary gamma camera (see Fig. 18.2). This investigation allows the function and/or the structure of the target tissue to be examined under both static and dynamic conditions.
Radioisotopes and radioactivity
Radioisotopes, as defined in Chapter 2, are isotopes with unstable nuclei that undergo radioactive disintegration. This disintegration is often accompanied by the emission of radioactive particles or radiation. The important emissions include:
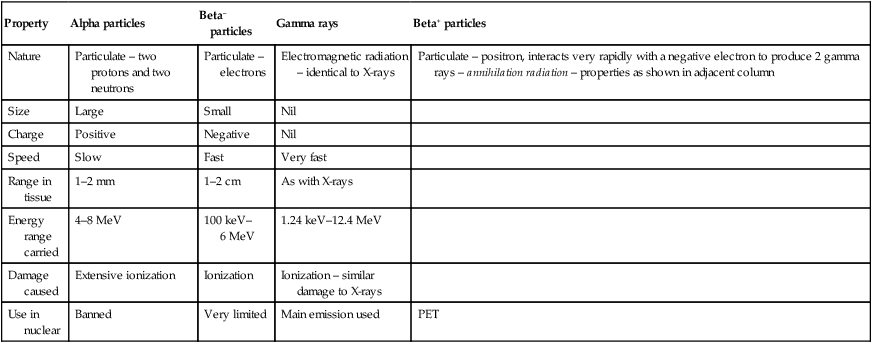
The main properties and characteristics of these emissions are summarized in Table 18.1.
Table 18.1
Summary of the main properties and characteristics of radioactive emissions
| Property | Alpha particles | Beta– particles | Gamma rays | Beta+ particles |
| Nature | Particulate – two protons and two neutrons | Particulate – electrons | Electromagnetic radiation – identical to X-rays | Particulate – positron, interacts very rapidly with a negative electron to produce 2 gamma rays – annihilation radiation – properties as shown in adjacent column |
| Size | Large | Small | Nil | |
| Charge | Positive | Negative | Nil | |
| Speed | Slow | Fast | Very fast | |
| Range in tissue | 1–2 mm | 1–2 cm | As with X-rays | |
| Energy range carried | 4–8 MeV | 100 keV–6 MeV | 1.24 keV–12.4 MeV | |
| Damage caused | Extensive ionization | Ionization | Ionization – similar damage to X-rays | |
| Use in nuclear | Banned | Very limited | Main emission used | PET |
Radioisotopes used in conventional nuclear medicine
• Technetium (99mTc) – salivary glands, thyroid, bone, blood, liver, lung and heart
99mTc is the most commonly used radioisotope. Its main properties include:
• Single 141 keV gamma emissions which are ideal for imaging purposes
• A short half-life of  hours which ensures a minimal radiation dose
hours which ensures a minimal radiation dose
• It is readily attached to a variety of different substances that are concentrated in different organs, e.g.:
• It can be used on its own in its ionic form (pertechnetate 99mTcO4–), since this is taken up selectively by the thyroid and salivary glands
Main indications for conventional isotope imaging in the head and neck
• Tumour staging – the assessment of the sites and extent of bone metastases
• Investigation of salivary gland function, particularly in Sjögren’s syndrome (see Ch. 32)
• Assessment of continued growth in condylar hyperplasia
• Investigation of the thyroid
• Brain scans and assessment of a breakdown of the blood–brain barrier.
Disadvantages
• There is poor image resolution – often only minimal information is obtained on target tissue anatomy.
• The radiation dose to the whole body can be relatively high.
• Images are not usually disease-specific.
• Difficult to localize exact anatomical site of source of emission.
Further developments in radioisotope imaging techniques include:
• Single photon emission computed tomography (SPECT), where the photons (gamma rays) are emitted from the patient and detected by a gamma camera rotating around the patient and the distribution of radioactivity is displayed as a cross-sectional image or SPECT scan enabling the exact anatomical site of the source of the emissions to be determined (see Fig. 18.3A).
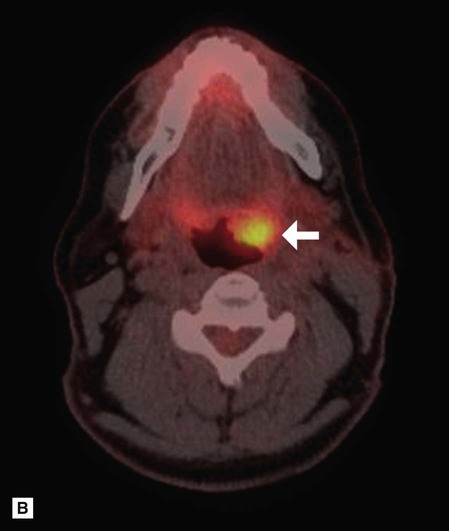
• Positron emission tomography (PET). As shown in Table 18.1, some radioactive isotopes decay by the emission of a positively charged electron (positron) from the nucleus. This positron usually travels a very short distance (1–2 mm) before colliding with a free electron. In the ensuing reaction, the mass of the two particles is annihilated with the emission of two (photons) gamma rays of high energy (511 keV) at almost exactly 180° to each other. These emissions, known as annihilation radiation, can then be detected simultaneously (in coincidence) by opposite radiation detectors which are arranged in a ring around the patient. The exact site of origin of each signal is recorded and a cross-sectional slice is displayed as a PET scan (see Fig. 18.3B). The major advantages of PET as a functional imaging technique are due to this unique detection method and the variety of new radioisotopes which can now be used clinically. These include:
Computed tomography (CT)
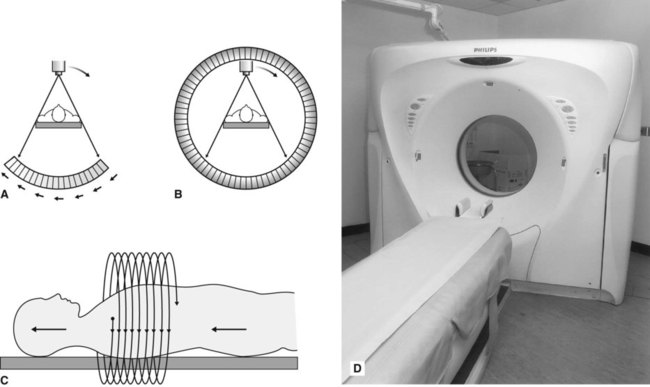
CT scanners use X-rays to produce computer generated tomographs – sectional or slice images (see Ch. 15). In CT the radiographic film is replaced by very sensitive crystal or gas detectors. The detectors measure the intensity of the X-ray beam emerging from the patient and convert this into digital data which are stored and can be manipulated by a computer, as described in Chapter 7. This numerical information is converted into a grey scale representing different tissue densities, thus allowing a visual image to be generated (see Fig. 18.4).

Equipment and theory
The CT scanner is essentially a large square piece of equipment (the gantry) with a central circular hole, as shown in Fig. 18.5A. The patient lies down with the part of the body to be examined within this circular hole. The gantry houses the X-ray tubehead and the detectors. The mechanical geometry of scanners varies. In so-called third-generation scanners, both the X-ray tubehead and the detector array revolve around the patient, as shown in Fig. 18.5. In so-called fourth-generation scanners, there is a fixed circular array of detectors (as many as 1000) and only the X-ray tubehead rotates, as shown in Fig. 18.5B. Whatever the mechanical geometry, each set of detectors produces an attenuation or penetration profile of the slice of the body being examined. The patient is then moved further into the gantry and the next sequential adjacent slice is imaged. The patient is then moved again, and so on until the part of the body under investigation has been completed. This stop–start movement means the investigation takes several minutes to complete and the radiation dose to the patient is high.
As a result, spiral CT has been developed in recent years. Acquiring spiral CT data requires a continuously rotating X-ray tubehead and detector system in the case of third-generation scanners or, for fourth-generation systems, a continuously rotating X-ray tubehead. This movement is achieved by slip-ring technology. The patient is now advanced continuously into the gantry while the equipment rotates, in a spiral movement, around the patient, as shown in Fig. 18.5C. The investigation time has been shortened to only a few seconds with a radiation dose reduction of up to 75%.
Whatever type of scanner is used, the level, plane and thicknesses (usually between 1.5 mm and 6 mm) of the slices to be imaged are selected and the X-ray tubehead rotates around the patient, scanning the desired part of the body and producing the required number of slices. These are usually in the axial plane, as was shown in Fig. 18.4.
The sequence of events in image generation can be summarized as follows:
• As the tubehead rotates around the patient, the detectors produce the attenuation or penetration profile of the slice of the body being examined.
• The computer calculates the absorption at points on a grid or matrix formed by the intersection of all the generation profiles for that slice.
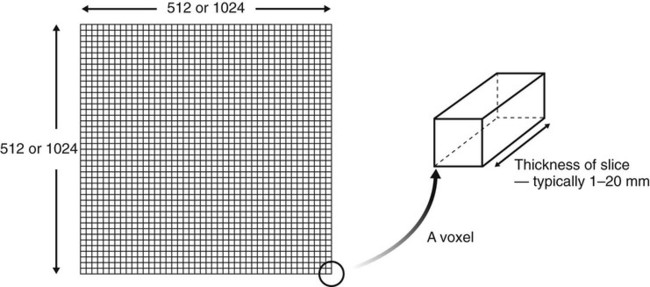
• Each point on the matrix is called a pixel and typical matrix sizes comprise either 512 × 512 or 1024 × 1024 pixels. The smaller the individual pixel the greater the resolution of the final image (as described for digital imaging in Chs 4 and 5).
• The area being imaged by each pixel has a definite volume, depending on the thickness of the tomographic slice, and is referred to as a voxel (see Fig. 18.6).
• Each voxel is given a CT number or Hounsfield unit between, for example, +1000 and −1000, depending on the amount of absorption within that block of tissue (see Table 18.2).
Table 18.2
Typical CT numbers for different tissues
| Tissue | CT number | Colour |
| Air | –1000 | Black |
| Fat | –100 to –60 | |
| Water | 0 | |
| Soft tissue | +40 to +60 | |
| Blood | +55 to +75 | |
| Dense bone | +1000 | White |
• Each CT number is assigned a different degree of greyness, allowing a visual image to be constructed and displayed on the monitor.
• The patient moves through the gantry and sequential adjacent sections are imaged.
• The selected images are photographed subsequently to produce the hard copy pictures, with the rest of the images remaining on disc.
Image manipulation
The major benefits of computer-generated images are the facilities to manipulate or alter the image and to reconstruct new ones, without the patient having to be re-exposed to ionizing radiation (see also Ch. 7).
Window level and window width
• Window level – this is the CT number selected for the centre of the range, depending on whether the lesion under investigation is in soft tissue or bone.
• Window width – the range selected to view on the screen for the various shades of grey, e.g. a narrow range allows subtle differences between very similar tissues to be detected.
Reconstructed images
The information obtained from the original axial scan can be manipulated by the computer to reconstruct tomographic sections in the coronal, sagittal or any other plane that is required, or to produce three-dimensional images, as shown in Fig. 18.7. However, to minimize the step effect evident in these reconstructed images, the original axial scans need to be very thin and contiguous or overlapping with a resultant relatively high dose of radiation to the patient.
Main indications for CT in the head and neck
• Investigation of intracranial disease including tumours, haemorrhage and infarcts
• Investigation of suspected intracranial and spinal cord damage following trauma to the head and neck
• Assessment of fractures involving:
• Assessment of the site, size and extent of cysts, giant cell and other bone lesions (see Fig. 18.8).
• Assessment of disease within the paranasal air sinuses (see Ch. 31)
• Tumour staging – assessment of the site, size and extent of tumours, both benign and malignant, affecting:
• Investigation of tumours and tumour-like discrete swellings both intrinsic and extrinsic to the salivary glands
• Investigation of osteomyelitis
• Preoperative assessment of maxillary and mandibular alveolar bone height and thickness before inserting implants (see Ch. 23).
Advantages over conventional film-based tomography
• Very small amounts, and differences, in X-ray absorption can be detected. This in turn enables:
– Detailed imaging of intracranial lesions
– Imaging of hard and soft tissues
– Excellent differentiation between different types of tissues, both normal and diseased.
• Axial tomographic sections are obtainable.
• Reconstructed images can be obtained from information obtained in the axial plane.
• Images can be enhanced by the use of IV contrast media to delineate blood vessels.
Disadvantages
• The equipment is very expensive.
• Very thin contiguous or overlapping slices result in a generally high dose investigation (see Ch. 3).
• Metallic objects, such as fillings, may produce marked streak or star artefacts across the CT image.
• There are inherent risks associated with IV contrast agents (see earlier).
Ultrasound
Diagnostic ultrasound is now established as the first choice imaging modality for soft tissue investigations of the face and neck, particularly of the salivary glands (see Ch. 32). It is a non-invasive investigation that uses a very high frequency (7.5–20 MHz) pulsed ultrasound beam, rather than ionizing radiation, to produce high resolution images of more superficial structures. The use of colour power Doppler allows blood flow to be detected.
Equipment and theory
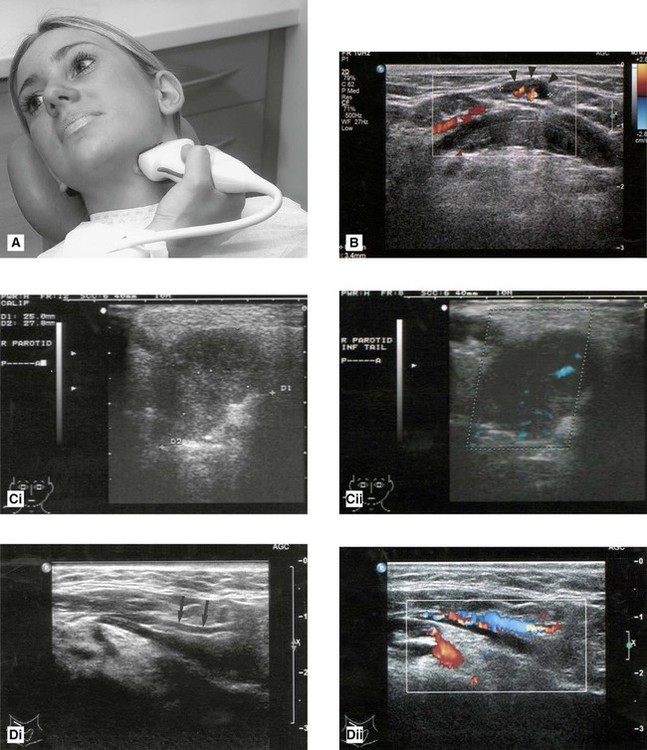
Several machines are available – an example is shown in Fig. 18.9. The high frequency ultrasound beam is directed into the body from a transducer placed in contact with the skin. Jelly is placed between the transducer and the skin to avoid an air interface, as shown in Fig. 18.10A. As the ultrasound travels through the body, some of it is reflected back by tissue interfaces to produce echoes, which are picked up by the same transducer and converted into an electrical signal and then into a real-time black, white and grey visual echo picture, which is displaced on a computer screen. Examples are shown in Fig. 18.10.
Utilization of the Doppler effect – a change in the frequency of sound reflected from a moving source – allows the detection of arterial and/or venous blood flow, as shown in Fig. 18.10. As can be seen, the computer adds the appropriate colour, red or blue, to the vascular structures in the visual echo picture image, making differentiation between structures straightforward.
Main indications for ultrasound in the head and neck
• Evaluation of swellings of the neck, particularly those involving the thyroid, cervical lymph nodes or the major salivary glands – ultrasound is now regarded as the investigation of choice for detecting solid and cystic soft tissue masses
• Detection of salivary gland and duct calculi (see Ch. 32)
• Determination of the relationship of vascular structures and vascularity of masses with the addition of colour flow Doppler imaging
• Assessment of blood flow in the carotids and carotid body tumours
• Assessment of the ventricular system in babies by imaging through the open fontanelles
• Therapeutically, in conjunction with the sialolithotripter, to break up salivary calculi into approximately 2-mm fragments which can then pass out of the ductal system so avoiding major surgery
Advantages over conventional X-ray imaging
• Sound waves are NOT ionizing radiation.
• There are no known harmful effects on any tissues at the energies and doses currently used in diagnostic ultrasound.
• Images show good differentiation between different soft tissues and are very sensitive for detecting focal disease in the salivary glands.
• The technique is widely available and relatively inexpensive.
Disadvantages
• Ultrasound has limited use in the head and neck region because sound waves are blocked by bone. Its use is therefore restricted to the superficial structures.
• The technique is operator-dependent.
• Images can be difficult to interpret for inexperienced operators.
• Real-time imaging means that the radiologist must be present during the investigation.
Magnetic resonance (MR)
Essentially it involves the behaviour of protons (positively charged nuclear particles, see Ch. 2) in a magnetic field. The simplest atom is hydrogen, consisting of one proton in the nucleus and one orbiting electron, and it is the hydrogen protons that are used to create the MR image. The image itself is another example of a tomograph or sectional image that at first glance resembles a CT image.
Equipment and theory
An example of an MR machine is shown in Fig. 18.11. The basic principles on how it works can be summarized as follows:

• The patient is placed within a very strong magnetic field (usually 1–3 Tesla). The patient’s hydrogen protons, which normally spin on an axis, behave like small magnets to produce the net magnetization vector (NMV) which aligns itself readily with the long axis of the magnetic field. This contributes to the longitudinal magnetic force or magnetic moment which runs along the long axis of the patient.
• Radiowaves are pulsed into the patient by the body coil transmitter at 90° to the magnetic field. These radiowaves are chosen to have the same frequency as the spinning hydrogen protons. This energy input is thus readily absorbed by the protons inducing them to resonate.
• The excited hydrogen protons then do two things:
First, they begin to precess like many small gyroscopes and their long axes move away from the long axis of the main magnetic field. This causes the longitudinal magnetic moment to diminish and the transverse magnetic moment to grow.
Second, their spins synchronize so that they behave like many small bar magnets spinning like tops in phase with each other. Together their total magnetic moment can be detected as a magnetic force precessing within the patient.
• This magnetic moment now lies transversely across the patient and since it is moving around the patient, it is in effect a fluctuating magnetic force and is therefore capable of inducing an electrical current in a neighbouring conductor or receiver.
• Surface coils act as receiver coils and detect the small electrical current induced by the signal for a long time and appear white on so-called T2-weighted images. Fat on the other hand has a short T2, produces a weak signal and appears dark on a T2-weighted image.
• As the hydrogen atoms relax, they drop back into the long axis of the main magnetic field and the longitudinal moment begins to increase. The rate at which it returns to normal is described by the time constant T1. Fluids have a long T1 (i.e. they take a long time to re-establish their longitudinal magnetic moment), produce a weak signal and appear dark on so-called T1-weighted images. Again fat behaves in the opposite manner and has a short T1, produces a strong signal and appears white on a T1-weighted image.
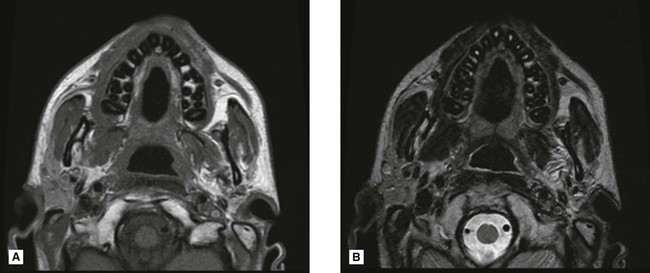
• The computer correlates this information and images may be produced that are either T1– or T2-weighted to show up differences in the T1 or T2 characteristics of the various tissues (see Fig. 18.12). Essentially T1-weighted images with a strong longitudinal signal show normal anatomy well, whereas T2-weighted images with a strong transverse signal show disease well.
• Alternatively, since the signal emanates principally from excited hydrogen protons, an image can be produced which indicates the distribution of protons in the tissues – the so-called proton density image where neither T1 or T2 effects predominate.
• By varying the frequency and timing of the radiofrequency input, the hydrogen protons can be excited to differing degrees allowing different tissue characteristics to be highlighted on a variety of imaging sequences. In addition, tissue characteristics can be changed by using gadolinium as a contrast agent, which shortens the T1 relaxation time of tissues giving a high signal on a T1-weighted image.
Main indications for MR in the head and neck
• Assessment of intracranial lesions involving particularly the posterior cranial fossa, the pituitary and the spinal cord
• Investigation of the salivary glands (see Ch. 32)
• Tumour staging – evaluation of the site, size and extent of soft and hard tissue tumours including nodal involvement, involving all areas in particular:
• Investigation of the TMJ to show both the bony and soft tissue components of the joint including the disc position (see Ch. 30). MR may be indicated:
Advantages
• Ionizing radiation is not used.
• No adverse effects have yet been demonstrated.
• Image manipulation is available.
• High-resolution images can be reconstructed in all planes (using 3-D volume techniques).
• Excellent differentiation between different soft tissues is possible and between normal and abnormal tissues, enabling useful differentiation between benign and malignant disease and between recurrence and postoperative effects.
Disadvantages
• Bone does not give an MR signal, a signal is only obtainable from bone marrow, although this is of less importance now that radiologists are used to looking at MR images.
• Scanning time can be long and is thus demanding on the patient.
• It is contraindicated in patients with certain types of surgical clips, cardiac pacemakers, cochlear implants and in the first trimester of pregnancy.
• Equipment tends to be claustrophobic and noisy.
• Metallic objects, e.g. endotracheal tubes, need to be replaced by non-ferromagnetic alternatives.
• The equipment is very expensive.
• The very powerful magnets can pose problems with siting of equipment although magnet shielding is now becoming more sophisticated.
• Bone, teeth, air and metallic objects all appear black, making differentiation difficult.
To access the self assessment questions for this chapter please go to www.whaitesessentialsdentalradiography.com