W8 Rehabilitation after Carpal Ligament Injury
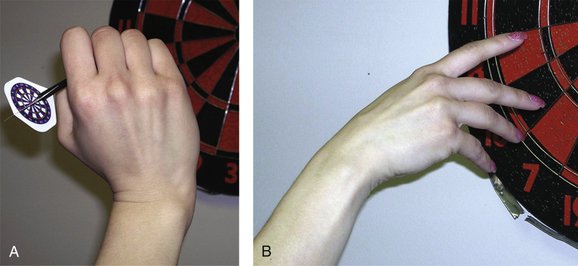
Relevant to this approach are the studies of functional ROM that were published in the 1980s, which illustrate that the wrist ROM required to perform most ADL tasks is less than what is considered normal ROM. Palmer and colleagues,1 in a study evaluating wrist motion used by normal subjects in the performance of standardized tasks, found that functional wrist ROM is between 5 degrees of flexion and 30 degrees of extension, 10 degrees of radial deviation, and 15 degrees of ulnar deviation. In this study, Palmer and colleagues1 described a “dart thrower’s motion” pattern (i.e., extension/radial deviation to flexion/ulnar deviation) that was used to perform many of the tasks. Ryu and associates2 found that 40 degrees of wrist extension, 40 degrees of wrist flexion, and a total of 40 degrees of radial and ulnar deviation are needed to perform most ADL.
Wrist Evaluation Procedures
The foundation for a wrist rehabilitation program is a thorough assessment. The components of the wrist assessment include a detailed history; visual inspection; objective measurements of ROM, strength, and sensibility; palpation and provocative testing; a functional assessment; and administration of an outcome measure appropriate for the wrist, such as MacDermid’s patient-rated wrist evaluation.3 If the patient has been referred to therapy from a nonspecialized practitioner with a vague diagnosis such as wrist pain or sprain, the clinical examination takes on even greater importance. In this instance, undiagnosed pathology may exist, therapy may not be indicated, and the patient may need to be referred to a hand surgeon for definitive diagnosis.
A baseline of the patient’s status and function is established with specific measurements of active ROM and passive ROM of all planes of wrist motion and of supination and pronation. Care must be taken when measuring passive ROM to stay within the patient’s comfort range and to avoid forceful end range overpressure. In some cases, passive ROM measurements may be deferred at the initial evaluation depending on the patient’s pain level and healing status. A goniometer is used to insure accuracy of measurement. The most reliable method for measuring wrist flexion and extension is with the goniometer placed on the dorsum of the wrist for flexion and on the volar aspect of the wrist for extension.4 Wrist ROM varies in the normal wrist; measurements of the uninvolved side should be taken for comparison.
The size of the wrist can be documented with circumference and volumetric measurements. For more acute conditions, the size of the wrist compared with the uninvolved side may be larger reflecting the presence of swelling, and with more chronic conditions, it may be smaller reflecting disuse and loss of muscle bulk. van Velze and colleagues5 found that the left nondominant side was 3.3% smaller than the dominant side with volume measurement in a study of 263 male laborers. The volumeter has been found to be reliable to within 1% of the total volume when one examiner performs the measurement.6
Grip strength measurement is performed with the use of a dynamometer. In some instances, measurement of grip strength may be deferred. In the case of a patient with an incompletely healed condition, referred after cast removal for early phase rehabilitation, grip testing would not be relevant and if attempted could potentially overstress the healing wrist. Guidelines for the recommended method of measurement have been published by the American Society of Hand Therapists.7 Regular calibration and maintenance of grip gauges is important to ensure accuracy and comparability of repeated measurements.
A sensibility screen is performed to help detect the presence of nerve compressions. The median, ulnar, and dorsal radial sensory nerve can be compressed or irritated with a wrist injury, and the cutaneous distribution of these nerves is examined. Semmes-Weinstein light touch threshold testing has been found to be the most sensitive clinical test for detecting nerve compression.8
In cases with a nonspecific diagnosis, such as “wrist pain or strain,” referred from a nonspecialized practitioner, a physical examination with palpation and provocative testing should be performed to identify the symptomatic regions and structures, and to determine if the patient should be referred to a hand surgeon for definitive diagnosis. Important for the performance of a physical examination is a thorough knowledge of surface anatomy and an understanding of the biomechanics and pathomechanics of the wrist and of the common conditions that may occur as a result of injury. Piecing together details from the history of the mechanism or onset of the injury or condition, and correlating this information with the physical findings can help in the process of determining what structures may be involved. The provocative clinical tests are used to identify the clicks, clunks, snaps, and pops of the various instability patterns and conditions that can occur. Examples of provocative tests include the scaphoid shift test, also referred to as the Watson test or radial stress test, used to assess scaphoid stability.9 The midcarpal shift test is performed to detect midcarpal instability,10 and the lunotriquetral ballottement test is used to detect lunotriquetral instability.11 These are only a few of a plethora of clinical provocative maneuvers that have been described and are helpful in the evaluation of a painful wrist.12 The importance of an accurate diagnosis cannot be overstated. If the therapist has any suspicion that more than a minor soft tissue strain has occurred, or the patient fails to improve after an initial brief trial of therapy, the patient should be referred to a specialist for further evaluation.
Selected Conditions and Guidelines for Rehabilitation
Scapholunate Instability
Scapholunate instability is an example of carpal instability dissociative, and is the most frequent form of carpal instability.13 Carpal instability dissociative refers to instability between carpal bones of the same carpal row.14 This instability is caused by partial or complete disruption of the intrinsic interosseous ligaments. Scapholunate instability refers to a spectrum of conditions, including subtle instability without overt anatomical disruption, but with insufficient load-bearing capacity; dynamic instability that occurs only under load; static instability with full dislocation/rotary subluxation of the scaphoid; and scapholunate advanced collapse.15 Rehabilitation for scapholunate ligament injuries depends on whether the injury is acute or chronic, the presence and degree of instability, and whether the therapy is to be provided preoperatively or postoperatively. A clinical provocative test for scapholunate instability is the scaphoid shift test, also known as the Watson test and the radial stress test.9 The scaphoid shift test is performed by the application of pressure over the volar prominence of the scaphoid as the wrist is moved from ulnar to radial deviation with slight flexion. A positive test reproduces the patient’s symptoms, usually a painful clunk.16
Nonoperative Management
ROM exercises in the “dart thrower’s”17 pattern may be better tolerated initially because during this pattern of motion there is minimal scaphoid and lunate motion and minimal scapholunate interosseous ligament elongation.18,19 This pattern involves the combined motions of wrist extension and radial deviation to wrist flexion and ulnar deviation. The dart thrower’s path of wrist motion allows a degree of radiocarpal stability; this direction, rather than the anatomical directions of flexion/extension and radial/ulnar deviation, may be the primary functional direction of the radiocarpal joint (Fig. W8-1).20 As the patient exhibits tolerance for this pattern of motion, standard wrist ROM exercises can be introduced.
With mild scapholunate instability, strengthening of the flexor carpi radialis has been suggested.15 The flexor carpi radialis passes over the scaphoid tuberosity on its path toward its distal insertion at the base of the second metacarpal; contraction of the flexor carpi radialis provides a volar restraint for the unstable scaphoid and an extension moment as long as the dorsal scapholunate ligaments are intact. Strengthening of the flexor carpi radialis without intact dorsal scapholunate ligaments could induce a dorsal translation of the proximal pole of the scaphoid with subluxation of the proximal pole.15 In this case, isometric radial deviation exercise involving the simultaneous contraction of the flexor carpi radialis and the extensor carpi radialis longus may be helpful in reinforcing scaphoid stability.
Postoperative Therapy
After scapholunate ligament repair or reconstruction, the wrist is immobilized in a thumb spica splint or cast for 8 weeks. After this initial period of immobilization, a removable thermoplastic thumb spica splint may be used for intermittent protection and support during the early phase of rehabilitation. Active ROM exercises for the wrist are initiated at this time. The “dart thrower’s” pattern of wrist ROM can be incorporated initially to minimize stress on the healing ligaments. Incision or portal scar massage and desensitization are begun. Light isometric strengthening can begin at 12 weeks; loading, power grip, weight bearing, and lifting all are avoided for 6 months.21
After a ligament augmentation procedure such as a dorsal capsulodesis, patients are immobilized in a thumb spica splint or cast for 8 weeks. At 8 weeks after pin removal, active ROM exercises for the wrist are initiated. A removable thermoplastic thumb spica splint is used for intermittent protection and support. Scar massage and desensitization are begun at this time. At 12 weeks, light strengthening with isometric exercises can begin; patients are progressed slowly with continuous monitoring of symptoms. No stress loading is permitted for 6 months, and wrist flexion is limited by 15 to 20 degrees.22 If by 12 weeks after surgery, wrist ROM is significantly limited, gentle static progressive splinting may be used to help increase wrist ROM.
After a limited intercarpal fusion, such as the scapholunate advanced collapse wrist procedure, the wrist is immobilized with a cast or splint up to 12 weeks until bony consolidation occurs. With more rigid internal fixation, motion may begin earlier. During the phase of immobilization, digital motion and edema control measures are included in a home program. Active ROM exercises are begun for the wrist when sufficient healing of the fusion has occurred as determined by the surgeon. ROM of the wrist is limited depending on the specific fusion performed and should not be stressed. Strengthening can begin when there is radiographic confirmation that bony union is achieved.23
Lunotriquetral Instability
Lunotriquetral instability is the second most frequent form of carpal instability and is an example of carpal instability dissociative.13 Lunotriquetral instability results from disruption of the lunotriquetral supporting ligaments from either a traumatic or a degenerative etiology. Volar rotation of the scaphoid and lunate with extension of the triquetrum can be seen with lunotriquetral instability. This pattern is termed volar intercalated segment instability. The rehabilitation program for a lunotriquetral injury must take into consideration whether the injury is acute or chronic, whether the condition resulted from an isolated tear or is part of a degenerative wear pattern seen with ulnocarpal abutment, and whether the plan is for operative versus nonoperative management.
Examples of clinical tests used in the detection of lunotriquetral instability include the ballottement test, the shear test, and the ulnar snuffbox test. The ballottement test is performed by stabilizing the lunate and attempting to displace the triquetrum volarly and dorsally with the other hand. A positive test elicits pain, clicking, or laxity.11
The shear test was described by Kleinman.13 The examiner’s fingers are placed dorsal to the lunate, and the thumb is placed on the pisotriquetral complex. With the lunate supported, the pisotriquetral complex is loaded in the anteroposterior plane, creating a shear force across the lunotriquetral joint. The wrist is ulnarly and radially deviated. The test is positive if pain or clicking is produced.
The ulnar snuffbox test involves lateral pressure on the triquetrum in the space distal to the ulnar head formed by the extensor carpi ulnaris and the flexor carpi ulnaris tendons. A positive test reproduces the patient’s pain.24
Nonoperative Management
Acute lunotriquetral ligament injuries treated nonoperatively are immobilized for 3 to 8 weeks with a short arm cast, an above-elbow cast or thermoplastic splint. The rationale for including the elbow is to eliminate the motion at the lunotriquetral joint that occurs during forearm rotation.15 A pad beneath the pisiform and over the dorsal distal radius may be used to maintain optimal alignment.15 During this initial period of immobilization, the patient performs finger ROM exercises and digital tendon gliding exercises. After the immobilization phase and during the early phases of rehabilitation from 2 to 4 weeks, the wrist is protected intermittently with a removable splint to protect against inadvertent stresses to the wrist from ADL. Active ROM exercises are begun to resolve stiffness and promote recovery of motion lost secondary to cast immobilization. Gradual resumption of ADL and progressive strengthening begins typically 2 to 4 weeks after the initial phase of therapy and as symptoms permit. The goal of the rehabilitation program is to prepare the wrist to handle the specific demands of ADL and work and leisure activities. Isometric exercises are generally better tolerated than isotonic exercises. Continuous monitoring of symptoms is stressed. Persistence of tenderness and swelling over the lunotriquetral interval with inability to progress to preinjury activity levels most likely indicates the need for re-evaluation by the referring hand surgeon.
Postoperative Management
After lunotriquetral repair and reconstruction with pinning, a short arm cast or splint is used for 8 weeks; digital motion and edema control are addressed during this phase of initial immobilization. After removal of pins usually at 8 weeks, a volar splint for the wrist is used for protection for an additional 4 weeks and is removed for ROM exercises and bathing. Active ROM exercises for the wrist begin at 8 weeks after pin removal. Desensitization, scar massage, and edema management are incorporated as needed. Light strengthening can begin at 12 weeks. Impact loading and forceful rotational motions should be avoided for 4 to 6 months.21
After lunotriquetral arthrodesis, a short arm cast or splint is used for 8 weeks; digital motion and edema control techniques are stressed during the phase of continuous immobilization. Active ROM exercises for the wrist begin at 8 weeks, and a removable volar wrist splint is used for protection until healing is complete. Desensitization, scar massage, and edema management are incorporated as needed. Light strengthening can begin at 12 weeks if healing of the arthrodesis is complete.25 Close communication with the referring surgeon is essential for the progression of the therapy program to increasing levels of load and resistance.
Midcarpal Instability
Midcarpal instability is an example of the Mayo Clinic’s category of carpal instability nondissociative and refers to instability between the proximal and distal carpal rows.14 Lichtman’s classification10 includes three categories of midcarpal instability. The first two are palmar and dorsal midcarpal instability depending on the direction of the instability. The third category is extrinsic midcarpal instability, which refers to instability that occurs as a result of an extrinsic cause, such as a distal radius fracture malunion. Palmar midcarpal instability is the more frequently encountered form of midcarpal instability and is characterized by a volar sag on the ulnar side of the wrist, a clunk that occurs at the end of the range of ulnar deviation with forearm pronation, tenderness over the triquetral-hamate and capitolunate intervals, and weakness of grip. A lateral radiograph of the wrist in neutral deviation often shows a volar intercalated segment instability pattern with slight palmar translation of the distal carpal row.26
The metacarpal shift test has been described by Lichtman and colleagues10 and is used to detect midcarpal instability. The test is performed by applying a volar load across the midcarpal joint and then ulnarly deviating the wrist with simultaneous axial load. A positive test is one that causes a painful clunk and reproduces the patient’s symptoms. Feinstein and associates26 described a grading system for the midcarpal shift test based on the degree of volar translation possible and on the presence of a clunk that occurs at the end range of ulnar deviation (Table W8-1). As with any of the wrist examination procedures, it is important to test the contralateral side. Often a painless clunk may be present on the uninvolved side, indicating laxity rather than pathology.
| Grade | Palmar Translation | Clunk |
|---|---|---|
| 1 | None | None |
| 2 | Minimal | Minimal |
| 3 | Moderate | Moderate |
| 4 | Maximal | Significant |
| 5 | Self-induced | Self-induced |
Alexander CE, Lichtman DM: Triquetrolunate instability. In Lichtman DM, Alexander AH, eds: The Wrist and Its Disorders. 2nd ed. Philadelphia: WB Saunders, 1997.
Nonoperative Management
Nonoperative management for midcarpal instability includes the use of wrist splints and supports, symptom-relieving measures and modalities, activity analysis and modifications as needed, and strengthening exercises for stabilization of the midcarpal joint. A midcarpal stabilization splint has been developed for palmar midcarpal instability (Fig. W8-2).27
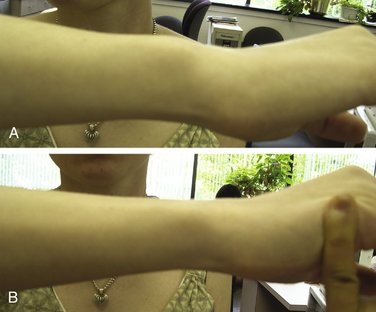
Isometric exercises are emphasized particularly for the extensor carpi ulnaris and the flexor carpi ulnaris. The combined action of the extensor carpi ulnaris and flexor carpi ulnaris during isometric exercise for ulnar deviation provides a degree of stabilization for the ulnar wrist (Fig. W8-3). Exercises can be done in supination, which is a more stable position for the wrist.28 Supination causes a decrease in ulnar variance with a tightening effect on the ulnar wrist ligaments. Exercises are progressed by altering the forearm position to perform the exercises in neutral and then in pronation. Grip strengthening exercises also can be done in supination. The patient’s symptom response must be monitored and used as a guide to the modification of and progression of the exercise program. Lichtman and colleagues10 described dynamic muscle compression achieved by activation of the extensor carpi ulnaris, flexor carpi ulnaris, and hypothenar muscles reproducing the normal joint contact forces in the absence of adequate ligament support.
Postoperative Rehabilitation
After soft tissue repair and reconstruction and pinning, the patient’s wrist is typically immobilized in a short arm cast or splint for 8 weeks. During this initial period of immobilization, the patient is instructed to perform digital motion and techniques of edema control if needed. When the pins are removed, usually at 8 to 10 weeks, a volar splint for the wrist is used for protection for an additional 4 weeks. The splint is removed for active ROM exercises and bathing. After this time, a Neoprene support can be used as the patient weans from the rigid splint. Aggressive passive motion or vigorous stretching is avoided to prevent overstress of the wrist and healing ligaments, which could potentially undermine the results of the surgery. Desensitization and scar massage are incorporated as needed. Light isometric strengthening can begin typically by 12 weeks. The patient is instructed to avoid unrestricted loading, power grip, weight bearing, and lifting for 6 months.10
After limited wrist fusion, wrist immobilization with a cast or splint is required for 12 weeks until bony consolidation occurs. With more rigid internal fixation, motion may begin earlier as determined by the surgeon. During the phase of immobilization, digital motion and edema control measures are included in a home program. Active ROM exercises are begun for the wrist when sufficient healing of the fusion has occurred as determined by the surgeon. ROM of the wrist is limited depending on the specific fusion performed and should not be stressed. Strengthening can begin when there is radiographic confirmation that bony union is achieved.23
1. Palmer AK, Werner FW, Murphy D, et al. Functional wrist motion: a biomechanical study. J Hand Surg [Am]. 1985;10:39.
2. Ryu J, Cooney WP, Askew LJ, et al. Functional ranges of motion of the wrist joint. J Hand Surg [Am]. 1991;16:409.
3. MacDermid JC. Development of a scale for patient rating of wrist pain and disability. J Hand Ther. 1996;9:178.
4. LaStayo PC, Wheeler DL. Reliability of passive wrist flexion and extension goniometric measurements: a multicenter study. Phys Ther. 1994;74:162.
5. van Velze CA, Kluever I, van der Merwe CA, et al. The difference in volume of dominant and non-dominant hands. J Hand Ther. 1991;4:6-9.
6. Waylett-Rendall J, Seibly DS. A study of the accuracy of a commercially available volumeter. J Hand Ther. 1991;4:10.
7. American Society of Hand Therapists. Clinical Assessment Recommendations, 2nd ed. Chicago: American Society of Hand Therapists; 1992.
8. Gelberman RH, Szabo RM, Williamson RV, Dimick MP. Sensibility testing in peripheral nerve compression syndrome: an experimental study in humans. J Bone Joint Surg Am. 1983;65:632.
9. Watson HK, Ashmead D, Makhlouf MV. Examination of the scaphoid. J Hand Surg [Am]. 1988;13:657.
10. Lichtman DM, Gaenslen ES, Pollack GR. Midcarpal and proximal carpal instabilities. In: Lichtman DM, Alexander CE, editors. The Wrist and Its Disorders. Philadelphia: WB Saunders, 1997.
11. Reagan DS, Linscheid RL, Dobyns JH. Lunotriquetral sprains. J Hand Surg [Am]. 1984;9:502.
12. Skirven TM, Osterman AL. Clinical examination of the wrist. In Mackin EJ, Callahan AD, Skirven TM, editors: Hunter, Mackin and Callahan Rehabilitation of the Hand and Upper Extremity, 5th ed, St. Louis: Mosby, 2002.
13. Bednar JM, Osterman AL. Carpal instability: evaluation and treatment. J Am Acad Orthop Surg. 1993;1:10-17.
14. Dobyns JH, Cooney WP. Classification of carpal instability. In: Cooney WP, Linscheid RL, Dobyns JH, editors. The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.
15. Garcia-Elias M, Geissler WB. Carpal instability. In Green DP, Hotchkiss RN, Pederson WC, editors: Green’s Operative Hand Surgery, 5th ed, Philadelphia: Elsevier, 2005.
16. Watson HK. Comments on the wrist: a comprehensive approach to challenging wrist problems. St. Louis: American Society of Hand Therapists Continuing Education Meeting; 1993.
17. Wolfe SW, Crisco JJ, Orr CM, et al. The dart-throwing motion of the wrist: is it unique to humans? J Hand Surg [Am]. 2006;31:1429.
18. Werner FW, Green JK, Short WH, et al. Scaphoid and lunate motion during a wrist dart throw motion. J Hand Surg [Am]. 2004;29:418.
19. Upal MA, Crisco JJ, Moore DC, et al. In vivo elongation of the palmar and dorsal scapholunate interosseous ligament. J Hand Surg [Am]. 2006;31:1326.
20. Crisco JJ, Coburn JC, Moore DC, et al. In vivo radiocarpal kinematics and the dart thrower’s motion. J Bone Joint Surg. 2005;87:2729.
21. Whipple TL. Arthroscopic Surgery: The Wrist. Philadelphia: JB Lippincott; 1992.
22. Blatt G. Capsulodesis in reconstructive hand surgery: dorsal capsulodesis for unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3:81-102.
23. Feldon PG, Nalebuff EA, Terrono AL. Partial wrist fusions: intercarpal and radiocarpal. In Lichtman DM, Alexander AH, editors: The Wrist and Its Disorders, 2nd ed, Philadelphia: WB Saunders, 1997.
24. Ambrose L, Posner M. Lunate-triquetral and midcarpal joint instability. Hand Clin. 1992;8:653.
25. Alexander CE, Lichtman DM. Triquetrolunate instability. In Lichtman DM, Alexander AH, editors: The Wrist and Its Disorders, 2nd ed, Philadelphia: WB Saunders, 1997.
26. Feinstein WK, Lichtman DM, Noble PC, et al. Quantitative assessment of the midcarpal shift test. J Hand Surg [Am]. 1999;24:977-983.
27. Skirven TM, DeTullio LM. Carpal fractures and instabilities. In: Burke SL, Higgins JP, McClinton MA, et al, editors. Hand and Upper Extremity Rehabilitation: A Practical Guide. Philadelphia: Elsevier, 2006.
28. Palmer AK, Glisson RR, Werner FW. Ulnar variance determination. J Hand Surg. 1982;7:376-379.