2 Advanced Airway Techniques
• Advanced airway management is predicated on selecting the right technical approach for a given patient.
• Anticipated difficult airway management often relies on a sedated (or “awake”) technique.
• An organized approach (and backup plan) is essential for success with an unanticipated difficult airway.
Perspective
The cognitive skills to determine when a patient requires airway support are as important as the manual skills to accomplish the task. Currently, rapid-sequence intubation (RSI) is the most frequently used and successful means of intubating the trachea in emergency medical practice.1–4 It is clear that combining the use of a paralytic agent with a sedative agent has resulted in more successful laryngoscopy.5,6 This has led to fewer failed airways. Because every attempt at intubation may be difficult, a prepared and practiced backup or contingency plan is vital. The discussion of the various techniques and adjunctive measures that follows in this chapter reflects their application within an overall strategy.
In some cases the use of paralytics (i.e., RSI) is inappropriate because of a relatively high likelihood of intubation failure and subsequent worsening of the clinical condition linked to intubation attempts and the probability of failed ventilation. Accordingly, it is important to distinguish patients who are likely to be difficult to intubate, ventilate, and rescue (which often means performing a cricothyrotomy). These concepts are emphasized by the LEMON, MOANS, and SHORT mnemonics7 covered in Chapter 1. What follows is an overview of a strategic approach to advanced emergency airway management.
Epidemiology
A difficult airway (a case in which intubation is difficult to achieve) in the emergency department (ED) is far less studied but is probably experienced more frequently than in the more controlled environment of the operating suite. Patient extremis and lack of patient preparation make encountering both anticipated and unanticipated difficult airways more likely, with some estimates as high as 20%.8 Fortunately, however, the frequency of intubation failure in the ED is much lower and approximates 1%.3,9,10 The prevalence of airways requiring rescue from previous failed attempts in the ED is difficult to determine. What is apparent is that rescue devices are not used routinely, although they are commonly available.11,12
Anticipated Difficulty
Multiple predictors related to airway anatomy have been reported in the anesthesia literature, but none have been shown to be useful in isolation for predicting intubation difficulty.13–18 However, some evidence suggests the use of a limited set of assessments in patients undergoing airway management in the ED. The LEMON mnemonic has been proposed for this purpose19,20 (Box 2.1) (see Chapter 1). If difficulty is predictable and the patient is not a suitable candidate for RSI, the optimal approach depends on the previous training of the intubator and the availability of advanced airway tools.
Anticipated Difficult Airway
Only a small fraction of patients undergoing ED intubation are actually deemed poor candidates for RSI, even though many patients are expected to be difficult to intubate. No discreet threshold at which RSI is deemed to be safe and when it is contraindicated has ever been determined, partly because of the lack of sensitivity of the various difficult airway prediction tools. Importantly, many ED patients are in extremis and unable to cooperate with a preprocedural examination.21,22 Much of what is discussed in the current literature is based on the anesthesia experience, which generally reflects the “elective” intubation of cooperative patients. Nevertheless, it is often useful to perform a preprocedural assessment, as allowed by time constraints and the patient’s condition. Some evaluation is necessary to be able to accurately estimate the potential for encountering a difficult airway.
The algorithm presented in Figure 2.1 represents a clinical approach to a difficult airway.7 Application of such an approach is predicated on the answers to several key questions:
• Is there enough time to plan a methodic approach?
• Despite the identified presence of difficult airway predictors, can RSI still be used safely?
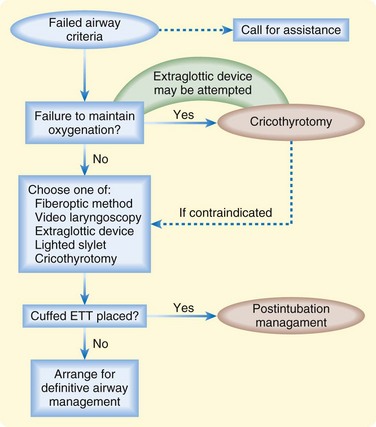
Fig. 2.1 Difficult airway algorithm.
(Adapted from Walls BM. The emergency airway algorithms. In: Walls RM, Murphy MF, editors. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008.)
Optimized Laryngoscopy
Head and Neck Positioning
In the absence of cervical spine immobilization, active range of neck flexion and extension can frequently provide markedly improved visualization.23
External Laryngeal Manipulation
External manipulation of the larynx is distinct from the familiar cricoid pressure concept (e.g., the Sellick maneuver). It is, however, related to BURP (backward, upward, rightward pressure). The process of laryngeal manipulation is active. It requires that the intubator actively move the larynx to maximize visualization of the laryngeal structures. Generally, once the view is optimized, an assistant will be required to maintain the preferred positioning.24–26
Alternative Techniques for the Anticipated Difficult Airway
Fiberoptics
As a class, directable and flexible scopes have been available for decades. They have recently been made more portable by replacing the heavy light source with a battery pack. These devices are consequently more convenient in the harried ED. The majority of the products currently on the market consist of a directable cable mechanism associated with a light source and fiberoptic bundle. Notable issues are that the glass fibers that constitute the optics are breakable and small amounts of debris can greatly diminish viewing quality. Historically, these devices were considered too expensive or impractical. In the future, however, these type of flexible and directable devices will probably become more available. To date, relatively little research relevant to emergency medicine practice has been conducted.2,27–29 A recent query of emergency medicine training programs in the United States suggests that the majority maintain this type of equipment,11 but clinical expertise is variable.
Flexible and Directable Fiberoptics
Flexible and directable fiberoptic models are portable and have variable diameters and lengths. This equipment varies depending on its intended purpose. The shorter nasopharyngoscope is approximately 35 cm in length, in contrast to the 60-cm bronchoscope. The goal is to directly visualize the glottis via the nares or mouth. Once the cords are visualized, the tip of the fiberoptic scope is advanced into the airway to the level of the carina. The preloaded endotracheal tube is then advanced over the scope and into the airway. Efficacy of this technique in an awake patient requires adequate patient and equipment preparation (Box 2.2).
Box 2.2 Patient Preparation
If using a nasal approach, adequate topical anesthesia and vasoconstriction can be achieved with various agents via an atomizer.
If using an oral approach, various spray anesthetic agents can be used in addition to a nebulized agents (e.g., lidocaine). Additionally, gargled lidocaine (4%) can be effective, patient cooperation permitting.
An antisialagogue (e.g., glycopyrrolate) can be useful to allow better tissue absorption of topical anesthetic agents. However, at least 20 minutes is needed for efficacy as a drying agent.
Sedation is used, as necessary, to achieve reasonable anxiolysis to improve patient cooperation.
Preoxygenation, as always, is fundamental to procedural sedation and airway management.
Tips and Tricks
1. Recognize that the procedure will take at least 15 to 20 minutes to accomplish. If the patient cannot tolerate such a wait, use of this technique may be misguided.
2. Stay in the anatomic midline at all times during the procedure. Straying laterally will often result in poor visualization and inability to pass the vocal cords.
3. Keep the slack out of the scope. If slack is present along the length of the scope, rotation of the body of the scope will not translate into rotation of the tip.
4. The size of the working channel in many scopes is often too small for suction to be effective.
5. If the tube is resistant to passage of the scope into the airway, it is likely that the tip of the tube, or Murphy’s eye, is caught at the level of the arytenoids. Rotation of the entire tube-scope apparatus 45 to 90 degrees will probably overcome the obstruction.
Semirigid Fiberoptics
The semirigid fiberoptic scope is, conceptually, a semimalleable stylet with internal fiberoptic bundles.34 These devices are similar to the nondirectable class of fiberoptics with respect to image quality and durability. An example of this type of device is the Shikani optical stylet (Clarus Medical, LLC, Minneapolis, MN).
Rigid Fiberoptics
Rigid fiberoptic scopes consist of an imaging bundle enclosed within a rigid L– or J-shaped assembly. This shape is designed for placement into the hypopharynx with subsequent indirect visualization of the glottis. One of the chief advantages of these devices is that limited head, neck, and jaw mobility is less of a concern because of the ability to “look around the corner” of the hypopharynx. Examples in this class are the Bullard (Circon Corporation, Stanford, CT),35–37 WuScope Tubular Fiberoptic Laryngoscope (Achi Corporation, San Jose, CA),38–41 and UpsherScope (Mercury Medical, Inc., Clearwater, FL).42,43 These scopes are relatively expensive and their availability in the ED has been limited.11
Optical Laryngoscopy
Optical laryngoscopes use a series of lenses to provide a view of the anterior aspect of the glottis that is often not possible with direct laryngoscopy. Although image quality is inferior to that of video laryngoscopes, optical laryngoscopes are inexpensive, durable, and portable tools for difficult airway management. An example is the Airtraq, a disposable optical laryngoscope with a J-shaped blade that allows visualization of the glottis with the head and neck in a neutral position. In small randomized and nonrandomized studies, the Airtraq improved glottic exposure, reduced intubation difficulty scores, decreased cervical spine motion, and caused less change in the heart rate than did direct laryngoscopy with a Macintosh laryngoscope.44–46
Video Laryngoscopy
Video laryngoscopes use either a micro video camera or more traditional fiberoptic bundles encased in a laryngoscope handle design. Placement of the camera is meant to provide a wide-angle view of the glottis but is somewhat more removed from the various debris issues often encountered with the optics-in-the-tube format. The GlideScope (Verathon, Inc., Bothell, WA) is an example of the micro video camera design. This device is relatively new with limited ED experience.47 The literature that exists suggests that it can be used with very little motion of the cervical spine and that glottic visualization is generally excellent.48–51 However, actual intubation may be a bit more of a challenge because it requires an extreme “hockey stick” angulation of the styletted endotracheal tube to reach the glottis. Currently, laryngoscope sizes available correspond roughly to Macintosh No. 4 and No. 2, as well as pediatric sizes.
Additionally, video has been adapted to the more familiar Macintosh blade format in the current C-MAC (Karl Storz, Tuttlingen, Germany). The video element has been shown to improve the grade of view in ED patients52 and in simulated patients with difficult airways.53
Tips and Tricks
GlideScope Use
The GlideScope handle stays in the midline—no tongue sweep.
The handle is not used to lift, unlike a more familiar laryngoscope.
To accommodate the approach to the glottis, the endotracheal tube with stylet will need an acute angle (approximately 90 degrees).
To accommodate advancement of the tube off the stylet, it may help to partially withdraw the stylet during tube advancement. Generally, this last step will require coordination with an assistant.
Awake Techniques
The term “awake” is a misnomer. It is important to realize that a better descriptor of this concept would be “sedated.” In a patient who is currently maintaining some airway tone and respiratory drive, this approach may be indicated when difficult intubation and ventilation are both anticipated. This approach may be somewhat time consuming because adequate sedation and topical anesthesia of the airway are required (Box 2.3). However, its advantage is that patients will be able to breathe on their own during attempts at definitively controlling the airway. It is important to understand the underlying pathologic process with respect to its dynamic impact on the airway. For instance, a quick look to determine the risks associated with RSI may be misleading if rapid swelling from burns or angioedema are evolving during the process. This concept should be kept in mind inasmuch as an initial look may be reassuring but subsequent attempts may be profoundly disappointing because of a dynamic clinical process.
Blind Nasotracheal Intubation
The overall success rate of blind nasotracheal intubation is lower than that of RSI.54,55 Additionally, such intubation can be complicated by nasal hemorrhage and induction of vomiting (with its associated risk of aspiration). However, it is often an expedient option in patients who still have fairly vigorous spontaneous respirations.
Light Wand
In general, light wand intubation does not rely on visualization of any internal structure. Instead, it relies on a transmitted glow of light through the soft tissues of the neck. The skill required for its application depends largely on recognizing midline (i.e., tracheal) versus lateral soft tissue placement. The Trachlight has been shown to be useful in the operating suite,56–60 but ED experience has been limited. Its design and the necessity for a pronounced L-shaped curve in the stylet and endotracheal tube make it rather forgiving of difficult anatomy that might otherwise inhibit direct laryngoscopy. It is important to note that proper tube placement and preparation of the device do take a few minutes. To make it more useful as a rescue device and more amenable to quick grab deployment, it should be prepared and stored in a ready-to-use condition.
The Unanticipated Difficult Airway
The difficult airway and failed airway are related but distinct concepts. A difficult airway becomes a failed airway after three attempts at intubation by a skilled operator. From this point, subsequent maneuvers are in large part directed by operator familiarity and skill. However, the key branch point in the decision-making process depends on the adequacy of ventilation. The “can’t intubate, can ventilate” scenario is managed differently from the “can’t intubate, can’t ventilate” scenario. Each of these situations will be approached within the concept of the failed airway algorithm (Fig. 2.2).
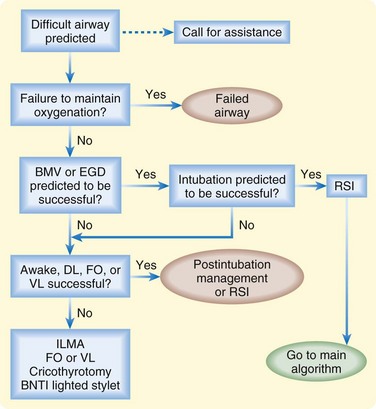
Fig. 2.2 Failed airway algorithm.
(Adapted from Walls RM. The emergency airway alorithm. In: Walls RM, Murphy MF, editors. Manual of emergency airway management. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008.)
Can’t Intubate, Can Ventilate
Tracheal Introducer
The tracheal introducer has been in use since the 1940s, and several products are currently available on the market. The Eschmann introducer is also known as the gum elastic bougie. Incidentally, this term is a misnomer because it is not a bougie (e.g., dilator), nor is it made from gum. Instead, it is a woven Dacron rod 30 cm long that is coated with resin for durability and added stiffness. Newer products have also recently arrived on the market (e.g., Frova, Cook Medical, Bloomington, IN). These introducers are used in conjunction with direct laryngoscopy, especially when the vocal cords cannot be visualized. Their design helps access an extremely anterior trachea and confirm proper placement. One of these design features is an angulated tip that allows directable manipulation and tactile feedback. The tip clicks as it bumps along the anterior tracheal rings. The absence of clicks may suggest esophageal placement. Additionally, if the introducer is in the airway, a hard stop will be felt as the introducer gently passes from the trachea into a small-diameter airway. In contrast, if the introducer is mistakenly placed in the esophagus, the operator will be able to advance the introducer without a firm end point as the introducer enters the stomach.61–65 Once these tactile indicators suggest tracheal placement, a standard endotracheal tube can then be advanced over the introducer and into the trachea.
Tips and Tricks
Success with a Tracheal Introducer
Ideal use is when the vocal cords are too anterior to visualize them well with direct laryngoscopy.
Have a helper ready to assist in advancing the tube over the introducer.
Once the introducer is in trachea, keep the laryngoscope in place and continue lifting. This will straighten the path for the endotracheal tube to slide over the introducer into the trachea.
If resistance is met as the endotracheal tube is advanced to the level of the glottis, the tube should be withdrawn slightly, rotated 45 to 90 degrees, and then advanced with gentle pressure.
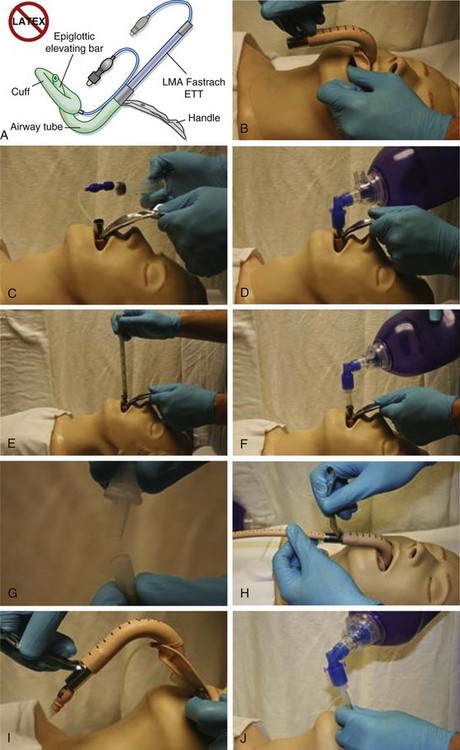
The Laryngeal Mask Airway
The laryngeal mask airway (LMA) currently has several variations in format, one of which, the intubating LMA (ILMA, e.g., Fastrach), is shown in Figure 2.3. This device has been demonstrated to provide adequate ventilation and a good opportunity for success with blind intubation through the LMA.66–73 Placement of the ILMA is nearly identical to that for a standard LMA, with one notable difference: the rigid handle of the ILMA allows easier manipulation of the device and does not require the operator to place fingers inside the patient’s mouth to guide placement. Once the ILMA is placed in the hypopharynx and the cuff is inflated, bag ventilation can begin. If ventilation is adequate (which is the case in the majority of patients and implies good ILMA positioning), the proprietary nonkinking endotracheal tube can be advanced through the lumen of the ILMA. In anesthesia reports such intubation has a high rate of success. The ILMA cuff is then deflated, the ILMA is removed over the endotracheal tube, and the tube is left in place as a definitive airway. The success rate in emergency patients in whom prior intubation attempts have failed and who often have full stomachs is thus far unpublished and unknown.
Can’t Intubate, Can’t Ventilate
Rescue Airway Devices
The LMA and ILA are two devices designed to create a mask seal over the laryngeal inlet to ventilate and oxygenate patients for short to intermediate periods during elective anesthesia or emergency airway management. The mask portions of each of these devices are similar in shape, but the ILA mask is slightly stiffer to prevent folding of the leading edge during insertion. Many clinicians have familiarity with laryngeal masks, thus making them useful rescue devices. Anesthesia studies report that the ILMA is effective in managing difficult and failed airways, but its performance in ED airway management has not been adequately studied.69,72,74,75 Several models are commercially available, but only two allow placement of a cuffed endotracheal tube in the trachea through the device (ILMA and ILA) and may therefore be more appropriate as rescue devices in the ED.
An additional type of extraglottic device is a laryngeal tube such as the Combitube and the King LT. These devices have a pharyngeal cuff and an esophageal cuff with a port between the cuffs at the level of the laryngeal inlet for ventilation. The King LT is shorter and simpler than the Combitube, has one large lumen instead of two smaller ones, and uses only one inflation valve to fill both cuffs. Few studies comparing extraglottic rescue airway devices have been performed, and data regarding superiority of one over another as rescue devices are lacking.76,77
Invasive Intubation
Studies done since the common acceptance of RSI in the ED show that approximately 1% of patients at large trauma centers still require cricothyrotomy.1,3,10 These procedures have generally been performed via an open surgical technique. However, newer developments have provided a percutaneous option. The advantage of this technique may lie in its familiarity of use because it relies on the routinely used Seldinger technique.
Several key considerations need to be taken into account with respect to cricothyrotomy. First, it should be recognized that providers are often hesitant to perform what may be perceived as a highly problematic and complicated procedure. In current practice it is not uncommon for the person performing the intubation to be the same individual who needs to recognize failure. Additionally, it is this same provider who will need to change course and provide an invasive airway. In this circumstance, overcoming cognitive inertia can be difficult and contribute to a disastrous delay. Many practitioners say that the most difficult portion of performing a cricothyrotomy is simply making the decision to do so. Such a decision is mandated in a “can’t intubate, can’t ventilate” scenario unless a bridging device can be used successfully. The presence of certain features may influence the actual approach chosen. It should be kept in mind that certain clinical circumstance may make an invasive airway particularly challenging. The mnemonic SHORT (Box 2.4) has been proposed for use when considering an invasive airway. Several technical variants of cricothyrotomy are in common use.
Open Surgical Technique
Among the techniques described in the literature, two are commonly referenced.
Standard Technique
The standard technique generally involves the surgeon being positioned over the right shoulder of the patient. The incision is midline and vertical, and a tracheal hook is placed into the thyroid cartilage. Cephalad traction is applied and a horizontal incision of the cricothyroid membrane is created. Dilation of the incision is followed by intubation (Fig. 2.4).78,79
Rapid Four-Step Technique
This technique has evolved from the standard technique for sake of expediency. The procedure is initiated from the head of the gurney, where the intubator is most likely to be positioned. If the pertinent anatomy is clearly palpable (step 1), the skin and cricothyroid membrane are incised simultaneously with a No. 20 scalpel in a horizontal orientation (step 2). A blunt hook is then applied along the caudal side of the scalpel. The hook is used to apply traction to the cricoid ring (step 3). The incision is thus stabilized and widened for subsequent intubation (step 4) (Fig. 2.5). This technique may be a favorable alternative to the standard technique for several reasons. First, the operator performs the procedure from the head of the bed instead of having to step around to the side of the bed. Second, the traction applied to the cricoid ring obliterates the pretracheal potential space, which may inadvertently be intubated when using the standard technique. Third, hand positioning when applying cricoid traction is somewhat similar to that with laryngoscopy. This familiarity can be beneficial in view of the infrequency of performing the procedure and the associated potential for atrophy of skills.80–84
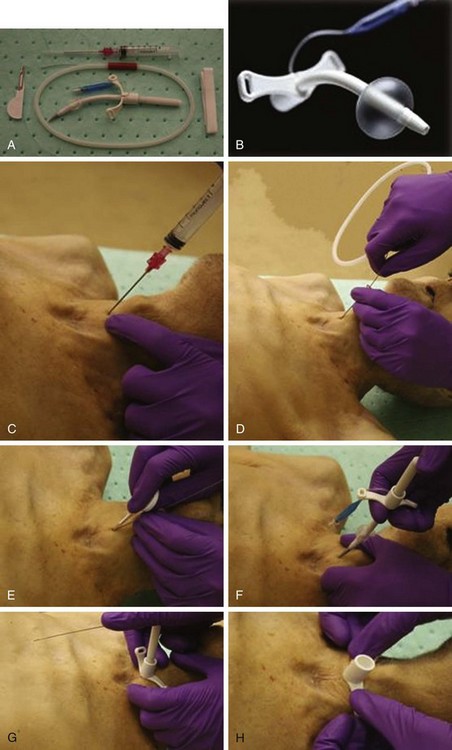
Percutaneous Technique
In contrast to the open techniques just described, this technique relies on a wire-through-needle (e.g., Seldinger) method for accessing the airway. Recent technologic advances have resulted in the production of cuffed endotracheal tubes that can be placed within the airway by using a dilator over a wire (Fig. 2.6).85,86
Pediatric Considerations
Invasive Considerations
In children younger than 10 years, open cricothyrotomy is contraindicated because of airway size. Currently, the only invasive method that is available for use in young children and infants is needle cricothyrotomy, which is commonly discussed in the context of jet insufflation. Such high-pressure oxygen has been shown to provide adequate short-term oxygenation with somewhat less successful ventilation. This technique does nothing to protect the airway because a cuffed tube is not present in the airway. Various adapted combinations have been described to allow the use of a ventilation bag (plus adaptor) with a cricothyrotomy needle. The pressure generated with such a bag is generally inadequate for all except small infants. In general, jet ventilation catheters such as the VBM catheter (Medizintechnik GmbH, Sulz am Neckar, Germany) are used with high-pressure jet ventilation systems (Fig. 2.7). Barotrauma is often a concern, and kinking or egress of the catheter from its original placement as a result of the high pressure can be an issue. In such a case, manual stabilization of the catheter assembly is prudent until a definitive airway can be established.
1 Sagarin MJ, Barton ED, Chang YM, et al. Airway management by US and Canadian emergency medicine residents: a multicenter analysis of more than 6,000 endotracheal intubation attempts. Ann Emerg Med. 2005;46:328–336.
2 Bair AE, Filbin MR, Kulkarni RG, et al. The failed intubation attempt in the emergency department: analysis of prevalence, rescue techniques, and personnel. J Emerg Med. 2002;23:131–140.
3 Sakles JC, Laurin EG, Rantapaa AA, et al. Airway management in the emergency department: a one-year study of 610 tracheal intubations. Ann Emerg Med. 1998;31:325–332.
4 Mandavia DP, Qualls S, Rokos I. Emergency airway management in penetrating neck injury. Ann Emerg Med. 2000;35:221–225.
5 Li J, Murphy-Lavoie H, Bugas C, et al. Complications of emergency intubation with and without paralysis. Am J Emerg Med. 1999;17:141–143.
6 Sivilotti ML, Filbin MR, Murray HE, et al. Does the sedative agent facilitate emergency rapid sequence intubation? Acad Emerg Med. 2003;10:612–620.
7 Walls RM, Murphy MF. Manual of emergency airway management, 3rd ed, Philadelphia: Lippincott Williams & Wilkins, 2008.
8 Orebaugh SL. Difficult airway management in the emergency department. J Emerg Med. 2002;22:31–48.
9 Tayal VS, Riggs RW, Marx JA, et al. Rapid-sequence intubation at an emergency medicine residency: success rate and adverse events during a two-year period. Acad Emerg Med. 1999;6:31–37.
10 Bair AE, Panacek EA, Wisner DH, et al. Cricothyrotomy: a 5-year experience at one institution. J Emerg Med. 2003;24:151–156.
11 Levitan RM, Kush S, Hollander JE. Devices for difficult airway management in academic emergency departments: results of a national survey. Ann Emerg Med. 1999;33:694–698.
12 Walsh K, Cummins F. Difficult airway equipment in departments of emergency medicine in Ireland: results of a national survey. Eur J Anaesthesiol. 2004;21:128–131.
13 Mallampati SR. Clinical sign to predict difficult tracheal intubation (hypothesis). Can Anaesth Soc J. 1983;30:316–317.
14 Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32:429–434.
15 Eberhart LH, Arndt C, Cierpka T, et al. The reliability and validity of the upper lip bite test compared with the Mallampati classification to predict difficult laryngoscopy: an external prospective evaluation. Anesth Analg. 2005;101:284–289.
16 Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42:487–490.
17 Tse JC, Rimm EB, Hussain A. Predicting difficult endotracheal intubation in surgical patients scheduled for general anesthesia: a prospective blind study. Anesth Analg. 1995;81:254–258.
18 Levitan RM, Ochroch EA, Kush S, et al. Assessment of airway visualization: validation of the percentage of glottic opening (POGO) scale. Acad Emerg Med. 1998;5:919–923.
19 Walls RM, ed. Manual of emergency airway management. Philadelphia: Lippincott Williams & Wilkins, 2004.
20 Reed MJ, Dunn MJ, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. 2005;22:99–102.
21 Bair AE, Caravelli R, Tyler K, et al. Feasibility of the preoperative Mallampati airway assessment in emergency department patients. J Emerg Med. 2010;38:677–680.
22 Levitan RM, Everett WW, Ochroch EA. Limitations of difficult airway prediction in patients intubated in the emergency department. Ann Emerg Med. 2004;44:307–313.
23 Levitan RM, Mechem CC, Ochroch EA, et al. Head-elevated laryngoscopy position: improving laryngeal exposure during laryngoscopy by increasing head elevation. Ann Emerg Med. 2003;41:322–330.
24 Benumof JL, Cooper SD. Quantitative improvement in laryngoscopic view by optimal external laryngeal manipulation. J Clin Anesth. 1996;8:136–140.
25 Ho AM, Chung DC. Use of external laryngeal manipulation to facilitate laryngoscopy. Ann Emerg Med. 2003;41:587. author reply 587-8
26 Knopp RK. External laryngeal manipulation: a simple intervention for difficult intubations. Ann Emerg Med. 2002;40:38–40.
27 Mlinek EJ, Jr., Clinton JE, Plummer D, et al. Fiberoptic intubation in the emergency department. Ann Emerg Med. 1990;19:359–362.
28 Delaney KA, Hessler R. Emergency flexible fiberoptic nasotracheal intubation: a report of 60 cases. Ann Emerg Med. 1988;17:919–926.
29 Schafermeyer RW. Fiberoptic laryngoscopy in the emergency department. Am J Emerg Med. 1984;2:160–163.
30 Birmingham B, Mentzer SJ, Body SC. Laryngeal mask airway for therapeutic fiberoptic bronchoscopic procedures. J Cardiothorac Vasc Anesth. 1996;10:519–520.
31 Benumof JL. A new technique of fiberoptic intubation through a standard LMA. Anesthesiology. 2001;95:1541.
32 Ianchulev SA. Through-the-LMA fiberoptic intubation of the trachea in a patient with an unexpected difficult airway. Anesth Analg. 2005;101:1882–1883.
33 Johr M, Berger TM. Fiberoptic intubation through the laryngeal mask airway (LMA) as a standardized procedure. Paediatr Anaesth. 2004;14:614.
34 Liem EB, Bjoraker DG, Gravenstein D. New options for airway management: intubating fibreoptic stylets. Br J Anaesth. 2003;91:408–418.
35 Cohn AI, Hart RT, McGraw SR, et al. The Bullard laryngoscope for emergency airway management in a morbidly obese parturient. Anesth Analg. 1995;81:872–873.
36 Wackett A, Anderson K, Thode H. Bullard laryngoscopy by naive operators in the cervical spine immobilized patient. J Emerg Med. 2005;29:253–257.
37 Watts AD, Gelb AW, Bach DB, et al. Comparison of the Bullard and Macintosh laryngoscopes for endotracheal intubation of patients with a potential cervical spine injury. Anesthesiology. 1997;87:1335–1342.
38 Smith CE, Sidhu TS, Lever J, et al. The complexity of tracheal intubation using rigid fiberoptic laryngoscopy (WuScope). Anesth Analg. 1999;89:236–239.
39 Smith CE, Pinchak AB, Sidhu TS, et al. Evaluation of tracheal intubation difficulty in patients with cervical spine immobilization: fiberoptic (WuScope) versus conventional laryngoscopy. Anesthesiology. 1999;91:1253–1259.
40 Wu TL, Chou HC. A new laryngoscope: the combination intubating device. Anesthesiology. 1994;81:1085–1087.
41 Wu TL, Chou HC. WuScope versus conventional laryngoscope in cervical spine immobilization. Anesthesiology. 2000;93:588–589.
42 Pearce AC, Shaw S, Macklin S. Evaluation of the Upsherscope. A new rigid fibrescope. Anaesthesia. 1996;51:561–564.
43 Fridrich P, Frass M, Krenn CG, et al. The UpsherScope in routine and difficult airway management: a randomized, controlled clinical trial. Anesth Analg. 1997;85:1377–1381.
44 Maharaj CH, O’Croinin D, Curley G, et al. A comparison of tracheal intubation using the Airtraq or the Macintosh laryngoscope in routine airway management: a randomised, controlled clinical trial. Anaesthesia. 2006;61:1093–1099.
45 Maharaj CH, Costello JF, McDonnell JG, et al. The Airtraq as a rescue airway device following failed direct laryngoscopy: a case series. Anaesthesia. 2007;62:598–601.
46 Hirabayashi Y, Fujita A, Seo N, et al. A comparison of cervical spine movement during laryngoscopy using the Airtraq or Macintosh laryngoscopes. Anaesthesia. 2008;63:635–640.
47 Platts-Mills TF, Campagne D, Chinnock B, et al. A comparison of GlideScope video laryngoscopy versus direct laryngoscopy intubation in the emergency department. Acad Emerg Med. 2009;16:866–871.
48 Cooper RM, Pacey JA, Bishop MJ, et al. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–198.
49 Agro F, Barzoi G, Montecchia F. Tracheal intubation using a Macintosh laryngoscope or a GlideScope in 15 patients with cervical spine immobilization. Br J Anaesth. 2003;90:705–706.
50 Turkstra TP, Craen RA, Pelz DM, et al. Cervical spine motion: a fluoroscopic comparison during intubation with lighted stylet, GlideScope, and Macintosh laryngoscope. Anesth Analg. 2005;101:910–915.
51 Sun DA, Warriner CB, Parsons DG, et al. The GlideScope Video Laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth. 2005;94:381–384.
52 Brown CA, 3rd., Bair AE, Pallin DJ, et al. Improved glottic exposure with the Video Macintosh Laryngoscope in adult emergency department tracheal intubations. Ann Emerg Med. 2010;56:83–88.
53 Bair AE, Olmsted K, Brown CA, 3rd., et al. Assessment of the Storz video Macintosh laryngoscope for use in difficult airways: a human simulator study. Acad Emerg Med. 2010;17:1134–1137.
54 Van Elstraete AC, Mamie JC, Mehdaoui H. Nasotracheal intubation in patients with immobilized cervical spine: a comparison of tracheal tube cuff inflation and fiberoptic bronchoscopy. Anesth Analg. 1998;87:400–402.
55 van Elstraete AC, Pennant JH, Gajraj NM, et al. Tracheal tube cuff inflation as an aid to blind nasotracheal intubation. Br J Anaesth. 1993;70:691–693.
56 Hung OR, Pytka S, Morris I, et al. Lightwand intubation: II—clinical trial of a new lightwand for tracheal intubation in patients with difficult airways. Can J Anaesth. 1995;42:826–830.
57 Hung OR, Stewart RD. Lightwand intubation: I—a new lightwand device. Can J Anaesth. 1995;42:820–825.
58 Agro F, Hung OR, Cataldo R, et al. Lightwand intubation using the Trachlight: a brief review of current knowledge. Can J Anaesth. 2001;48:592–599.
59 Hirabayashi Y, Hiruta M, Kawakami T, et al. Effects of lightwand (Trachlight) compared with direct laryngoscopy on circulatory responses to tracheal intubation. Br J Anaesth. 1998;81:253–255.
60 Croinin DF, Coleman MM. The Trachlight compared to laryngeal mask airway assisted intubation. Anaesthesia. 2002;57:715–716. author reply 716
61 Bair AE, Laurin EG, Schmitt BJ. An assessment of a tracheal tube introducer as an endotracheal tube placement confirmation device. Am J Emerg Med. 2005;23:754–758.
62 Carley S, Jackson R. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Gum elastic bougies in difficult intubation. Emerg Med J. 2001;18:376–377.
63 Combes X, Dumerat M, Dhonneur G. Emergency gum elastic bougie–assisted tracheal intubation in four patients with upper airway distortion. Can J Anaesth. 2004;51:1022–1024.
64 Phelan MP. Use of the endotracheal bougie introducer for difficult intubations. Am J Emerg Med. 2004;22:479–482.
65 Morton T, Brady S, Clancy M. Difficult airway equipment in English emergency departments. Anaesthesia. 2000;55:485–488.
66 Levitan RM, Ochroch EA, Stuart S, et al. Use of the intubating laryngeal mask airway by medical and nonmedical personnel. Am J Emerg Med. 2000;18:12–16.
67 Pollack CV, Jr. The laryngeal mask airway: a comprehensive review for the emergency physician. J Emerg Med. 2001;20:53–66.
68 Foley LJ, Ochroch EA. Bridges to establish an emergency airway and alternate intubating techniques. Crit Care Clin. 2000;16:429–444. vi
69 Parmet JL, Colonna-Romano P, Horrow JC, et al. The laryngeal mask airway reliably provides rescue ventilation in cases of unanticipated difficult tracheal intubation along with difficult mask ventilation. Anesth Analg. 1998;87:661–665.
70 Stanwood PL. The laryngeal mask airway and the emergency airway. AANA J. 1997;65:364–370.
71 Young B. The intubating laryngeal-mask airway may be an ideal device for airway control in the rural trauma patient. Am J Emerg Med. 2003;21:80–85.
72 Ferson DZ, Rosenblatt WH, Johansen MJ, et al. Use of the intubating LMA-Fastrach in 254 patients with difficult-to-manage airways. Anesthesiology. 2001;95:1175–1181.
73 Wakeling HG, Bagwell A. The intubating laryngeal mask (ILMA) in an emergency failed intubation. Anaesthesia. 1999;54:305–306.
74 Fukutome T, Amaha K, Nakazawa K, et al. Tracheal intubation through the intubating laryngeal mask airway (LMA-Fastrach) in patients with difficult airways. Anaesth Intensive Care. 1998;26:387–391.
75 Rosenblatt WH, Murphy M. The intubating laryngeal mask: use of a new ventilating-intubating device in the emergency department. Ann Emerg Med. 1999;33:234–238.
76 Russi CS, Miller L, Hartley MJ. A comparison of the King-LT to endotracheal intubation and Combitube in a simulated difficult airway. Prehosp Emerg Care. 2008;12:35–41.
77 Calkins MD, Robinson TD. Combat trauma airway management: endotracheal intubation versus laryngeal mask airway versus Combitube use by Navy SEAL and Reconnaissance combat corpsmen. J Trauma. 1999;46:927–932.
78 Mace S, Hedges J. Cricothyrotomy and translaryngeal jet insufflation. In: Roberts JR, Hedges JR. Clinical procedures in emergency medicine. Philadelphia: Saunders, 2004.
79 Walls RM. Cricothyroidotomy. Emerg Med Clin North Am. 1988;6:725–736.
80 Brofeldt BT, Osborn ML, Sakles JC, et al. Evaluation of the rapid four-step cricothyrotomy technique: an interim report. Air Med J. 1998;17:127–130.
81 Brofeldt BT, Panacek EA, Richards JR. An easy cricothyrotomy approach: the rapid four-step technique. Acad Emerg Med. 1996;3:1060–1063.
82 Holmes JF, Panacek EA, Sakles JC, et al. Comparison of 2 cricothyrotomy techniques: standard method versus rapid 4-step technique. Ann Emerg Med. 1998;32:442–446.
83 Bair AE, Laurin EG, Karchin A, et al. Cricoid ring integrity: implications for cricothyrotomy. Ann Emerg Med. 2003;41:331–337.
84 Davis DP, Brkamwell KJ, Vilke GM, et al. Cricothyrotomy technique: standard versus the rapid four-step technique. J Emerg Med. 1999;17:17–21.
85 Chan TC, Bilke GM, Bramwell KJ, et al. Comparison of wire-guided cricothyrotomy versus standard surgical cricothyrotomy technique. J Emerg Med. 1999;17:957–962.
86 Eisenburger P, Laczika K, List M, et al. Comparison of conventional surgical versus Seldinger technique emergency cricothyrotomy performed by inexperienced clinicians. Anesthesiology. 2000;92:687–690.