Chapter 52 Adrenal Insufficiency in the Intensive Care Unit
2 Describe the main types of adrenal insufficiency seen in patients in the ICU
 Relative adrenal insufficiency: This is the most common and perplexing type of adrenal insufficiency seen in patients in the ICU. Patients with relative adrenal insufficiency may present with vasopressor dependency, acute multiple organ dysfunction, hypothermia, or an inability to wean from mechanical ventilation. These patients can be identified by their limited response to adrenal stimulation tests or lower-than-expected basal cortisol levels despite critical illness.
Relative adrenal insufficiency: This is the most common and perplexing type of adrenal insufficiency seen in patients in the ICU. Patients with relative adrenal insufficiency may present with vasopressor dependency, acute multiple organ dysfunction, hypothermia, or an inability to wean from mechanical ventilation. These patients can be identified by their limited response to adrenal stimulation tests or lower-than-expected basal cortisol levels despite critical illness.
 Acute adrenal crisis or insufficiency: The acute clinical presentation typically includes profound hypotension, fever, and hypovolemia. These patients will have very low cortisol levels (<3 mcg/dL).
Acute adrenal crisis or insufficiency: The acute clinical presentation typically includes profound hypotension, fever, and hypovolemia. These patients will have very low cortisol levels (<3 mcg/dL).
5 How is adrenal insufficiency diagnosed?
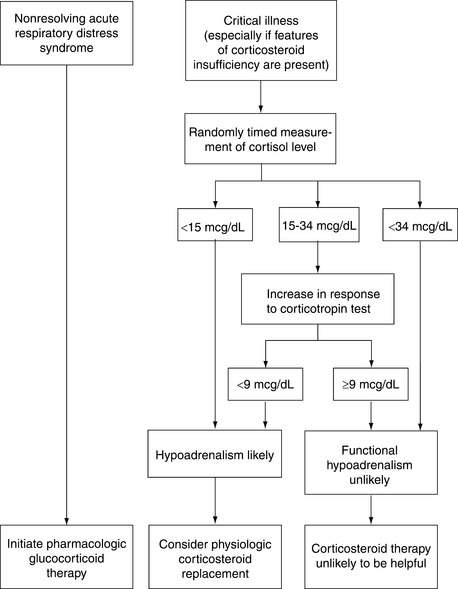
 In ICU patients: The use of provocative adrenal stimulation tests in critically ill patients remains controversial. Perhaps the most widely used protocol (from Annane et al.) identifies patients with septic shock as having relative adrenal insufficiency if their baseline cortisol level is <35 mcg/dL and they respond to an ACTH stimulation test (250 mcg corticotropin) with a bump in cortisol of <10 mcg/dL (see Fig. 52-1). The patients identified as nonresponders appeared to have a reduction in mortality when given stress-dose steroids. However, in a large subsequent study, no mortality benefit with stress-dose steroids was observed for patients with or without evidence of relative adrenal insufficiency.
In ICU patients: The use of provocative adrenal stimulation tests in critically ill patients remains controversial. Perhaps the most widely used protocol (from Annane et al.) identifies patients with septic shock as having relative adrenal insufficiency if their baseline cortisol level is <35 mcg/dL and they respond to an ACTH stimulation test (250 mcg corticotropin) with a bump in cortisol of <10 mcg/dL (see Fig. 52-1). The patients identified as nonresponders appeared to have a reduction in mortality when given stress-dose steroids. However, in a large subsequent study, no mortality benefit with stress-dose steroids was observed for patients with or without evidence of relative adrenal insufficiency.
 In non-ICU patients: In a nonstressed patient, a random cortisol level >20 mcg/dL may rule out the diagnosis of adrenal insufficiency. A random cortisol level <3 mcg/dL confirms the diagnosis of adrenal insufficiency.
In non-ICU patients: In a nonstressed patient, a random cortisol level >20 mcg/dL may rule out the diagnosis of adrenal insufficiency. A random cortisol level <3 mcg/dL confirms the diagnosis of adrenal insufficiency.
11 What ICU patient groups are at high risk for adrenal insufficiency?
 Patients taking chronic steroids: See question 10.
Patients taking chronic steroids: See question 10.
 Patients with HIV disease: The adrenal gland may be involved in >50% of patients infected with HIV. However, because adrenal function requires <20% of the gland to function, adrenal insufficiency in this population is uncommon (3%).
Patients with HIV disease: The adrenal gland may be involved in >50% of patients infected with HIV. However, because adrenal function requires <20% of the gland to function, adrenal insufficiency in this population is uncommon (3%).
 Patients with cancer: Even when cancers metastasize to the adrenal gland, adrenal dysfunction is uncommon.
Patients with cancer: Even when cancers metastasize to the adrenal gland, adrenal dysfunction is uncommon.
 High-risk postoperative patients: Patients >55 years old, patients undergoing major operations (e.g., coronary artery bypass grafting, abdominal aortic aneurysm repair, Whipple procedure), patients with multiple trauma, and postoperative patients requiring vasopressors or failing to wean from mechanical ventilation appear to be at higher risk for adrenal insufficiency.
High-risk postoperative patients: Patients >55 years old, patients undergoing major operations (e.g., coronary artery bypass grafting, abdominal aortic aneurysm repair, Whipple procedure), patients with multiple trauma, and postoperative patients requiring vasopressors or failing to wean from mechanical ventilation appear to be at higher risk for adrenal insufficiency.
13 Should every critically ill ICU patient with relative adrenal insufficiency receive stress-dose steroids?
14 What are the indicated therapies for ICU patients with septic shock who may or may not have adrenal insufficiency?
 Fluid resuscitation: Patients with septic shock typically require multiple large boluses of intravenous fluids and often vasopressors to maintain effective arterial circulation. If the patient’s blood pressure responds poorly to fluids and vasopressors, the administration of stress-dose steroids should be initiated.
Fluid resuscitation: Patients with septic shock typically require multiple large boluses of intravenous fluids and often vasopressors to maintain effective arterial circulation. If the patient’s blood pressure responds poorly to fluids and vasopressors, the administration of stress-dose steroids should be initiated.
 Steroid dosing: Administration of hydrocortisone, 300 to 400 mg/day given intravenously in three or four divided doses with or without fludrocortisone (50 mcg enterally every day), is accepted practice.
Steroid dosing: Administration of hydrocortisone, 300 to 400 mg/day given intravenously in three or four divided doses with or without fludrocortisone (50 mcg enterally every day), is accepted practice.
 Steroid duration: For adult patients with septic shock whose blood pressure is poorly responsive to multiple intravenous fluid boluses and vasopressor for >1 to 2 hours, the author recommends administration of stress-dose hydrocortisone (300 mg/day) for 4 days. If the patient shows rapid clinical improvement, the steroids may be stopped or tapered over 1 to 2 days. If significant hypotension recurs, steroid dosing should return to the initial dose, and a rapid taper can be undertaken after 7 days.
Steroid duration: For adult patients with septic shock whose blood pressure is poorly responsive to multiple intravenous fluid boluses and vasopressor for >1 to 2 hours, the author recommends administration of stress-dose hydrocortisone (300 mg/day) for 4 days. If the patient shows rapid clinical improvement, the steroids may be stopped or tapered over 1 to 2 days. If significant hypotension recurs, steroid dosing should return to the initial dose, and a rapid taper can be undertaken after 7 days.
15 Should stress-dose steroid supplementation be strongly considered in all patients with septic shock?
Because of conflicting studies, opinions on this point differ.
 Yes, of course: A majority of patients with septic shock have relative adrenal insufficiency. The mortality rate for such patients is 30% to 60%. A landmark randomized control trial found an absolute mortality reduction of 10% among patients with severe sepsis or septic shock and relative adrenal insufficiency who received stress-dose steroids versus placebo. This finding is supported by a recent systematic review that concluded that prolonged low-dose steroid use reduces all-cause mortality among adult patients with septic shock. Steroid supplementation for most ICU patients with septic shock makes sense given the modest risk of a short course of low-dose steroids.
Yes, of course: A majority of patients with septic shock have relative adrenal insufficiency. The mortality rate for such patients is 30% to 60%. A landmark randomized control trial found an absolute mortality reduction of 10% among patients with severe sepsis or septic shock and relative adrenal insufficiency who received stress-dose steroids versus placebo. This finding is supported by a recent systematic review that concluded that prolonged low-dose steroid use reduces all-cause mortality among adult patients with septic shock. Steroid supplementation for most ICU patients with septic shock makes sense given the modest risk of a short course of low-dose steroids.
 No, the data are too mixed: The Annane trial did not demonstrate across-the-board mortality reduction in the steroid group with severe sepsis and septic shock. The subsequent CORTICUS study showed no mortality benefit after hydrocortisone therapy in patients with septic shock. No mortality benefit of steroids was seen even among patients who met criteria for relative adrenal insufficiency. In addition, the steroid arm of the CORTICUS trial had significantly more superinfections. Early, smaller studies indicated a survival benefit from using steroids in septic shock. However, this benefit was not seen in meta-analysis of later and larger studies. The Surviving Sepsis Campaign International Guidelines recommend using steroids for patients with septic shock unresponsive to fluids and vasopressors. This is largely a consensus-based recommendation rather than an evidence-based conclusion. The scientific evidence to support even this limited use of steroids in patients with septic shock is modest.
No, the data are too mixed: The Annane trial did not demonstrate across-the-board mortality reduction in the steroid group with severe sepsis and septic shock. The subsequent CORTICUS study showed no mortality benefit after hydrocortisone therapy in patients with septic shock. No mortality benefit of steroids was seen even among patients who met criteria for relative adrenal insufficiency. In addition, the steroid arm of the CORTICUS trial had significantly more superinfections. Early, smaller studies indicated a survival benefit from using steroids in septic shock. However, this benefit was not seen in meta-analysis of later and larger studies. The Surviving Sepsis Campaign International Guidelines recommend using steroids for patients with septic shock unresponsive to fluids and vasopressors. This is largely a consensus-based recommendation rather than an evidence-based conclusion. The scientific evidence to support even this limited use of steroids in patients with septic shock is modest.
Key Points Adrenal insufficiency
1. Relative adrenal insufficiency is common in ICU patients with septic shock, but its clinical importance remains controversial.
2. To decide if and when a patient should receive hydrocortisone therapy for septic shock, there is no need to evaluate the patient for relative adrenal insufficiency.
3. ICU patients with septic shock whose blood pressure does not respond to fluid boluses and vasopressors should receive stress-dose steroids.
4. Critically ill ICU patients who recently received a prednisone equivalent to ≥5 mg/day for ≥7 days should probably receive stress-dose steroid coverage.
1 Albert S.G., Ariyan S., Rather A. The effect of etomidate on adrenal function in critical illness: a systematic review. Intensive Care Med. 2011;37:901–910.
2 Annane D., Bellissant E., Bollaert P., et al. Corticosteroids in the treatment of severe sepsis and septic shock in adults. JAMA. 2009;301:2362–2375.
3 Annane D., Sebille V., Charpentier C., et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2005;288:862–871.
4 Brown C.J., Buie W.D. Perioperative stress dose steroids: do they make a difference? J Am Coll Surg. 2001;193:678–686.
5 Cohan C., Wang C., McArthur D., et al. Acute secondary adrenal insufficiency after traumatic brain injury: a prospective study. Crit Care Med. 2005;22:2358–2366.
6 Cooper M.S., Stewart P.M. Corticosteroid insufficiency in acutely ill patients. N Engl J Med. 2003;348:727–734.
7 Dellinger R.P., Levy M.M., Carlet J.M., et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med. 2008;36:296–327.
8 Ehrman R., Wira C., Lomax A., et al. Etomidate use in severe sepsis and septic shock patients does not contribute to mortality. Intern Emerg Med. 2011;6:253–257.
9 Hamrahian A.H., Oseni T.S., Arafah B.M. Measurements of serum free cortisol in critically ill patients. N Engl J Med. 2004;50:1629–1638.
10 Krasner A.S. Glucocorticoid-induced adrenal insufficiency. JAMA. 1999;282:671–676.
11 Mayo J., Collazos J., Martinez E., et al. Adrenal function in the human immunodeficiency virus–infected patient. Arch Intern Med. 2002;162:1095–1098.
12 Rivers E.P., Gaspari M., Saad G.A., et al. Adrenal insufficiency in high-risk surgical ICU patients. Chest. 2001;119:889–896.
13 Sligl W.I., Milner D.A., Sundar S., et al. Safety and efficacy of corticosteroids for the treatment of septic shock: a systematic review and meta-analysis. Clin Infect Dis. 2009;49:93–101.
14 Sprung C.L., Annane D., Key D., et al. The CORTICUS randomized, double-blind, placebo-controlled study of hydrocortisone therapy in patients with septic shock. N Engl J Med. 2008;358:111–124.
15 Sprung C.L., Brezis M., Goodman S., et al. Corticosteroid therapy for patients in septic shock: some progress in a difficult decision. Crit Care Med. 2011;39:571–574.
16 Zaloga G.P., Marik P. Hypothalamic-pituitary-adrenal insufficiency. Crit Care Clin. 2001;17:25–41.