Acute Respiratory Distress Syndrome
After reading this chapter, you will be able to:
• List the anatomic alterations of the lungs associated with acute respiratory distress syndrome.
• Describe the causes of acute respiratory distress syndrome.
• List the cardiopulmonary clinical manifestations associated with acute respiratory distress syndrome.
• Describe the general management of acute respiratory distress syndrome.
• Describe the clinical strategies and rationales of the SOAPs presented in the case study.
• Define key terms and complete self-assessment questions at the end of the chapter and on Evolve.
Anatomic Alterations of the Lungs
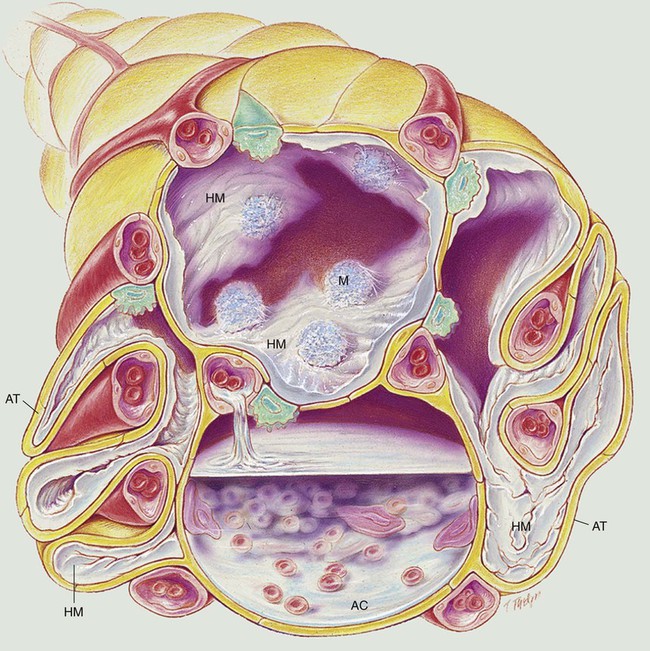
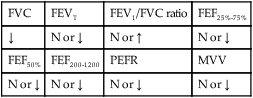
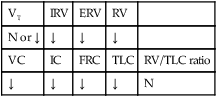
In gross appearance the lungs of patients with ARDS are heavy and “red,” “beefy,” or “liver-like.” The anatomic alterations that develop in ARDS create a restrictive lung disorder (see Figure 27-1).
The major pathologic or structural changes associated with ARDS are as follows:
• Interstitial and intra-alveolar edema and hemorrhage
• Intraalveolar hyaline membrane formation
Historically, ARDS was first referred to as the “shock lung syndrome” when the disease was first identified in combat casualties during World War II. Since that time, the disease has appeared in the medical literature under many different names, all based on the conditions believed to be responsible for the disease. In 1967 the disease was first described as a specific entity, and the term acute respiratory distress syndrome was suggested. This term is predominantly used today. Box 27-1 provides some of the other names that have appeared in the medical journals to identify ARDS.
General Management of Acute Respiratory Distress Syndrome
Respiratory Care Treatment Protocols
Oxygen Therapy Protocol
Oxygen therapy is used to treat hypoxemia, decrease the work of breathing, and decrease myocardial work. Because of the hypoxemia associated with ARDS, supplemental oxygen often is required. The hypoxemia that develops in ARDS most commonly is caused by widespread alveolar consolidation, atelectasis, increased alveolar capillary thickening. Hypoxemia caused by capillary shunting often is refractory to oxygen therapy (see Oxygen Therapy Protocol, Protocol 9-1).
Mechanical Ventilation Protocol
Mechanical ventilation is often needed to provide and support alveolar gas exchange and eventually return the patient to spontaneous breathing. Continuous mechanical ventilation is justified when the acute ventilatory failure is thought to be reversible (see Protocols 9-5, 9-6, and 9-7).
Ventilation Strategy for Adult Respiratory Distress Syndrome*
The therapeutic goal of low tidal volume ventilation is to (1) decrease high transpulmonary pressures, (2) reduce overdistention of the lungs, and (3) decrease barotrauma. (See Mechanical Ventilation Protocols, Protocol 9-5, Protocol 9-6, and Protocol 9-7.)
CASE STUDY
Acute Respiratory Distress Syndrome (ARDS)
Admitting History and Physical Examination
Respiratory Assessment and Plan
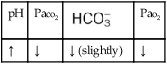
O Patient is comatose. BP 100/60; HR 114; RR 28; T 101.5° F; bilateral crackles; CXR: bilateral infiltrates, worse on right side; ABGs on 5 L/min O2: pH 7.51, Paco2 29,  23, and Pao2 52.
23, and Pao2 52.
• Sedative drug overdose with coma (history)
• Acute alveolar hyperventilation with moderate hypoxemia (ABGs)
• Impending ventilatory failure
• Aspiration pneumonitis without previous history of pulmonary disease vs ARDS (history and x-ray film)
P Oxygen Therapy Protocol: (100% O2 via nonrebreathing mask). Confer with physician regarding Mechanical Ventilation Protocol. Arterial line placement. Continuous oximetry. Repeat ABG 1 hour after intubation and prn.
Respiratory Assessment and Plan
O Patient remains comatose. BP 90/60, HR 130, T 100.2° F. Bilateral crackles, rhonchi, and wheezes. ABGs on decreased VT of 400 mL, rate 20, Fio2 1.0, and +20 PEEP: pH 7.31, Paco2 49,  25, and Pao2 38. Spo2: 70%. CXR: ARDS with bilateral infiltrates and atelectasis, worse on the right side. Purulent sputum. PA pressure (mean) 27 mm Hg.
25, and Pao2 38. Spo2: 70%. CXR: ARDS with bilateral infiltrates and atelectasis, worse on the right side. Purulent sputum. PA pressure (mean) 27 mm Hg.
• Persistent coma (physical exam)
• Aspiration pneumonitis progressing to ARDS with bilateral infiltrates and atelectasis (x-ray film)
• Increasing airway secretions with infection (fever, crackles, rhonchi, and purulent sputum)
• Acute ventilatory failure on present ventilator settings (acceptable hypercapnia)
P Call physician to discuss worsening Pao2 and to confirm an acceptable hypercapnia level and PEEP upper limit. Bronchopulmonary Hygiene Therapy Protocol and Aerosolized Medication Protocol (add 2 mL 10% acetylcysteine to 0.5 mL albuterol and aerosolize q2h; suction prn). Adjust Mechanical Ventilation Protocol (titrate tidal volume and rate to raise Paco2 to permissive hypercapnia range). Gram stain and culture sputum. Closely monitor and reevaluate.
Discussion
This was possibly a preventable death. Gastric lavage never should be performed on an unconscious patient unless the airway is first protected with a cuffed endotracheal tube. This is one of the very few categoric imperatives in pulmonary medicine. The following three causative factors known to produce ARDS may have been operative in this patient: (1) drug overdose, (2) aspiration of gastric contents, and (3) breathing an excessive Fio2 for a long period. As time progressed, the patient’s lungs became stiffer and physiologically nonfunctional as a result of the anatomic alterations associated with ARDS. Careful measurement of the alveolar-arterial oxygen tension difference (P[A-a]O2) would have detected this (see page 72).
As documented in the first assessment, her crackles, rhonchi, refractory hypoxemia, and x-ray findings all reflected the pathophysiologic changes seen in patients with Atelectasis (see Figure 9-8) and/or Increased Alveolar-Capillary Membrane Thickening (see Figure 9-10). Aggressive Lung Expansion Therapy (see Protocol 9-3), in the form of PEEP, was used with mechanical ventilation right from the start. When the chest radiograph confirmed severe ARDS after 72 hours of therapy, the immediate changes in the mechanical ventilator settings—the reduction in the patient’s tidal volume to 350 mL, the increased respiratory rate of 20 breaths/min, and permissive hypercapnia—were all clearly indicated and appropriate. Unfortunately, these therapeutic techniques and use of ECMO to manage the condition were not enough in the final analysis.
*Over the past several decades, a number of ventilation strategies have been used, studied, and evaluated for the treatment of ARDS. Such ventilation strategies have included high-frequency ventilation (HFV), tracheal gas insufflation (TGI), inverse-ratio ventilation (IRV), airway pressure release ventilation (APRV), patient repositioning (including prone position), extracorporeal membrane oxygenation (ECMO), extracorporeal carbon dioxide removal (ECCO2R), exogenous surfactant administration, liquid (perfluorocarbon) mechanical ventilation, inhaled nitric oxide (NO), and corticosteroid administration. Despite some encouraging results with some of these ventilation strategies, the safety, effectiveness, and survival benefits associated with these ventilation modes have not been established.



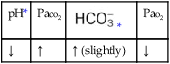
 values will be lower than expected for a particular Pa
values will be lower than expected for a particular Pa

 )
)
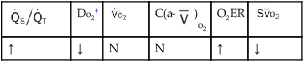
 )O2, Arterial-venous oxygen difference; DO2, total oxygen delivery; O2ER, oxygen extraction ratio;
)O2, Arterial-venous oxygen difference; DO2, total oxygen delivery; O2ER, oxygen extraction ratio;  , pulmonary shunt fraction;
, pulmonary shunt fraction;  , mixed venous oxygen saturation;
, mixed venous oxygen saturation;  , oxygen consumption.
, oxygen consumption.
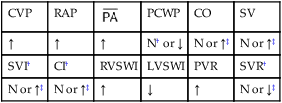
 , mean pulmonary artery pressure; PCWP, pulmonary capillary wedge pressure; PVR, pulmonary vascular resistance; RAP, right atrial pressure; RVSWI, right ventricular stroke work index; SV, stroke volume; SVI, stroke volume index; SVR, systemic vascular resistance.
, mean pulmonary artery pressure; PCWP, pulmonary capillary wedge pressure; PVR, pulmonary vascular resistance; RAP, right atrial pressure; RVSWI, right ventricular stroke work index; SV, stroke volume; SVI, stroke volume index; SVR, systemic vascular resistance.
 23, and Pa
23, and Pa 25, and Pa
25, and Pa