Chapter 47 Acute Pancreatitis
9 How do you determine the severity and prognosis of AP?
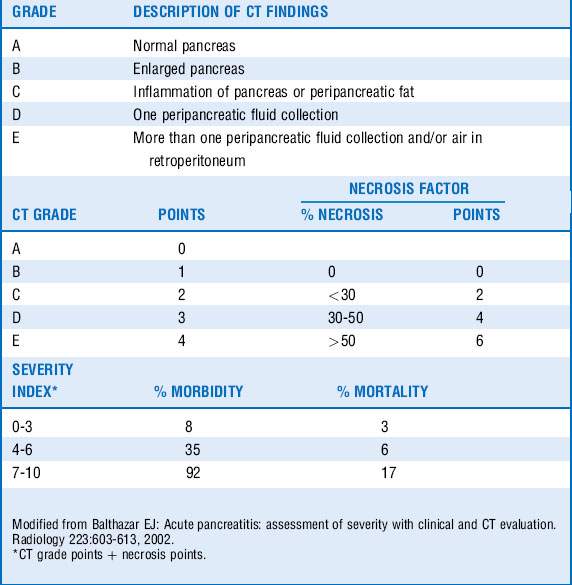
Ranson criteria (Table 47-1) were one of the earliest and widely used scoring systems. Their major disadvantage was that they required 48 hours to complete. The Acute Physiology and Chronic Health Evaluation (APACHE) II system, developed to evaluate critically ill patients, has also been used to differentiate mild AP from SAP. The major disadvantage of this system is that many find it cumbersome as it requires 12 physiologic measures to calculate. A CT severity index (Balthazar score, Table 47-2), has been developed and often used to predict severity of pancreatitis on the basis of radiographic features. The bedside index of severity in AP (BISAP) score (Table 47-3) integrates the systemic inflammatory response syndrome (SIRS) criteria and can be calculated relatively quickly on admission.
| Etiology of pancreatitis | ||
|---|---|---|
| Nongallstone | Gallstone | |
| At initial presentation | ||
| Age (yr) | > 55 | > 70 |
| White blood cell count (k/mm3) | >16 | >18 |
| Glucose (mg/dL) | > 200 | > 220 |
| Lactate dehydrogenase (U/L) | > 350 | >400 |
| Aspartate (AST) (U/L) | > 250 | >250 |
| During first 48 hours | ||
| Decrease in hematocrit (%) | ≥10 | >10 |
| Elevation in blood urea nitrogen (mg/dL) | >5 | >2 |
| Serum total calcium (mg/dL) | <8 | < 8 |
| Partial pressure of oxygen (mm Hg) | < 60 | NA |
| Base deficit (mmol/L) | >4 | > 5 |
| Fluid sequestration (L) | > 6 | > 4 |
| Prognosis | No. of Criteria Met | Predicted Mortality |
|---|---|---|
| ≤2 | 0.9% | |
| 3-4 | 16% | |
| 5-6 | 40% | |
| 7-8 | 100% |
NA, Not applicable.
Modified from Ranson JH, Rifkind KM, Roses DF, et al: Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet 139:69-81, 1974; and Ranson JH: Etiological and prognostic factors in human acute pancreatitis: a review. Am J Gastroenterol 77:633-638, 1982.
| 1 point for each of the following if present, 0 points if absent |
| BUN > 25 mg/dL (8.9 mmol/L) |
| Impaired mental status |
| BISAP score | Mortality (%) |
|---|---|
| 0-2 | <1 |
| 2 | 2 |
| 3-5 | 5-20 |
BUN, Blood urea nitrogen; WBC, white blood cells.
Modified from Wu BU, Johannes RS, Sun X, et al: The early prediction of mortality in acute pancreatitis: a large population-based study. Gut 57:1698-1703, 2008.
1 Cheung M.T., Li W.H., Kwok P.C., et al. Surgical management of pancreatic necrosis: towards lesser and later. J Hepatobiliary Pancreat Sci. 2010;17:338–344.
2 Lindkvist B., Appelros S., Manjer J., et al. A prospective cohort study of smoking in acute pancreatitis. Pancreatology. 2008;8:63–70.
3 McClave S.A., Chang W.K., Dhaliwal R., et al. Nutrition support in acute pancreatitis: a systematic review of the literature. JPEN J Parenter Enteral Nutr. 2006;30:143–156.
4 Moretti A., Papi C., Aratari A., et al. Is early endoscopic retrograde cholangiopancreatography useful in the management of acute biliary pancreatitis? A meta-analysis of randomized controlled trials. Dig Liver Dis. 2008;40:379–385.
5 Spanier B.W., Nio Y., van der Hulst R.W., et al. Practice and yield of early CT scan in acute pancreatitis: a Dutch Observational Multicenter Study. Pancreatology. 2010;10:222–228.
6 Talukdar R. Swaroop Vege S: Early management of severe acute pancreatitis. Curr Gastroenterol Rep. 2011;13:123–130.
7 Thrower E.C., Gorelick F.S., Husain S.Z. Molecular and cellular mechanisms of pancreatic injury. Curr Opin Gastroenterol. 2010;26:484–489.
8 Uhl W., Buchler M.W., Malfertheiner P., et al. A randomised, double blind, multicentre trial of octreotide in moderate to severe acute pancreatitis. Gut. 1999;45:97–104.
9 van Baal M.C., van Santvoort H.C., Bollen T.L., et al. Systematic review of percutaneous catheter drainage as primary treatment for necrotizing pancreatitis. Br J Surg. 2011;98:18–27.
10 Villatoro E., Mulla M., Larvin M. Antibiotic therapy for prophylaxis against infection of pancreatic necrosis in acute pancreatitis. Cochrane Database Syst Rev. 5, 2010. CD002941
11 Warndorf M.G., Kurtzman J.T., Bartel M.J., et al. Early fluid resuscitation reduces morbidity among patients with acute pancreatitis. Clin Gastroenterol Hepatol. 2011;9:705–709.
12 Wittau M., Mayer B., Scheele J., et al. Systematic review and meta-analysis of antibiotic prophylaxis in severe acute pancreatitis. Scand J Gastroenterol. 2011;46:261–270.