Chapter 24 Acute Elbow Dislocations and Management
Introduction
The elbow is the second most commonly dislocated major joint in the body after the shoulder, with an annual incidence of 6.1 dislocations per 100 000 population. Elbow dislocations constitute approximately 10–25% of all elbow injuries and approximately 6.8% of all treated fractures or dislocations.1–3
The most common mechanism of injury is a fall onto the outstretched hand in which the elbow is extended and the shoulder is abducted. This is most often seen with high-energy mechanisms such as motor vehicle accidents and sports injuries. The median age for an elbow dislocation is 30 years.3 Almost all complete elbow dislocations without large periarticular fractures cause rupture of the medial and lateral collateral ligaments. Fortunately, the vast majority of these injuries can be treated conservatively without surgical intervention.
Elbow dislocations are classified according to the direction of forearm displacement relative to the distal humerus. Most consist of posterior or posterolateral displacement although less commonly lateral and anterior displacement of the forearm can also occur. Elbow dislocations can also be classified as simple or complex, and this is determined by the presence or absence of concomitant bony fractures. Simple dislocations are characterized by the absence of associated fractures, while complex dislocations are associated with large periarticular fractures. It should be noted that although pre- and post-reduction radiographs reveal large periarticular fractures in 12–60% of cases (complex elbow dislocations), operative exploration has documented unrecognized soft tissue injuries in nearly 100% of elbow dislocations.4 The most common complex dislocation pattern is an acute elbow dislocation with a fracture of the radial head. However, complex elbow dislocations encompass a wide range of bony and ligamentous injuries that result in elbow instability and usually require surgical intervention. As a result, the rest of this chapter will focus on the anatomy, diagnosis, treatment and outcomes of simple elbow dislocations.
Background/aetiology
Dunning et al performed a biomechanical cadaveric study in which sequential sectioning of the radial collateral and lateral ulnar collateral ligaments was performed in 12 cadaveric elbows. After each stage of the sectioning protocol, internal/external rotation and varus/valgus laxity were evaluated with an electromagnetic tracking device. They noted no significant difference in the magnitude of internal/external rotation and varus/valgus laxity of the ulna, with only the radial collateral or lateral ulnar collateral ligament intact. It was therefore concluded that, when the annular ligament is intact, either the radial collateral ligament or the lateral ulnar collateral ligament can be transected without inducing posterolateral rotatory instability of the elbow.5 The results of this study suggest that surgical approaches which violate only the anterior or posterior half of the lateral collateral ligament complex should not result in posterolateral rotatory instability of the elbow. Therefore a surgical approach to the radial head, for example, can transect the radial collateral ligament and not result in instability. Similarly, a surgical approach that violates the lateral ulnar collateral ligament would also not result in instability provided the radial collateral ligament complex was intact.
Some osseous relationships have also been described in the context of simple elbow dislocation. Wadstrom et al evaluated the anatomical relationship of the semilunar notch of the ulna in patients with elbow dislocation. They compared lateral radiographic views of 100 patients with elbow dislocations with radiographs from 150 patients without dislocation or other radiographic pathology. They noted a lower coronoid process as well as a more prominent tip of the olecranon in the radiographs of patients who had sustained an elbow dislocation. They concluded that the dislocation mechanism was at least partially hyperextension, with the tip of the olecranon acting as the pivot point.6
Presentation, evaluation and initial treatment
Patients with acute elbow dislocation tend to present with pain, soft tissue swelling and an obvious deformity of the elbow (Fig. 24.1). A thorough neurovascular examination of the upper extremity should always be performed. Closed elbow dislocations are rarely associated with vascular injury, and only a handful of brachial artery injuries associated with closed simple elbow dislocation have been reported.7 In open dislocations, however, the brachial artery is more often disrupted due to the forcible hyperextension of the elbow. Median and/or ulnar nerve injury is also commonly associated with such injuries. Neurapraxia has been reported to occur in approximately 20% of elbow dislocations and usually involves the anterior interosseous branch of the median nerve and/or the ulnar nerve. Ulnar nerve palsy has been reported in 14% of adult elbow dislocations, and the incidence is much higher in paediatric elbow dislocations with an associated medial epicondyle fracture. Most neurological deficits are transient, but entrapment of the median nerve within the elbow joint following reduction is relatively common in paediatric elbow dislocations and if not recognized will cause permanent disability.8 The wrist and shoulder joints should be carefully examined to rule out a concomitant upper extremity injury, which have been noted in 10–15% of acute elbow dislocations.9 Of note, the distal radio-ulnar joint (DRUJ) and forearm interosseous membrane should always be examined for tenderness and instability to rule out an associated interosseous membrane disruption.
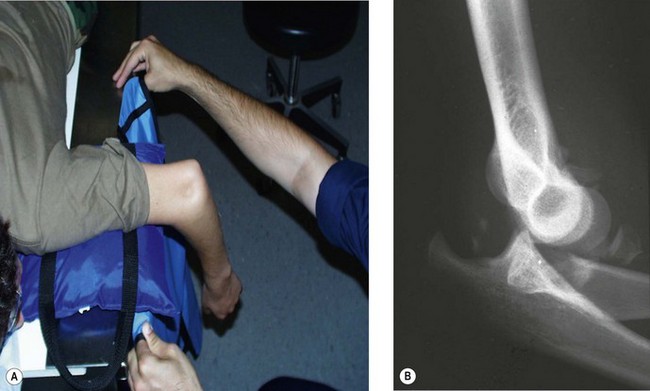
Simple elbow dislocations are acutely treated with reduction. Reduction requires adequate muscular relaxation and appropriate analgesia. This is usually done in the emergency department with intravenous or intramuscular medication. The acute treatment of the posterior or posterolateral dislocated elbow in the emergency department is to place the patient in the prone position and to supinate the patient’s arm. With the proximal part of the arm over a padded bolster on the edge of the examining table, pressure is applied to the olecranon tip in a distal and posterior direction as the elbow is gradually flexed, resulting in reduction. Muscular relaxation is necessary for adequate reduction, and the quality of the reduction often provides a clue to postreduction stability. A palpable reduction ‘clunk’ is a favourable sign of joint stability (Fig. 24.2).10
After determining that the elbow reduction is stable in 30° of flexion, post-reduction AP and lateral radiographs should be performed to document concentric reduction in two planes. In difficult cases, fluoroscopy may be of significant assistance. The radiographs should be assessed for joint widening, irregularity or malalignment. Persistent instability or joint widening may indicate posterolateral rotatory instability or the interposition of soft tissue or osteochondral fragments (Fig. 24.3).
Treatment and rehabilitation
A stable elbow articulation following reduction of a simple dislocation will generally allow early flexion and extension, as long as valgus stress is prevented. The vast majority of simple elbow dislocations, therefore, can be treated non-operatively. Only in situations of persistent redislocation and/or elbow instability is surgery indicated. In terms of non-operative management, recommendations concerning the type and duration of immobilization tend to vary widely. Over the last several years, multiple studies have been performed to investigate the type and duration of immobilization following closed reduction of elbow dislocations as well as the role of surgical intervention following simple elbow dislocation.10–13
Non-operative treatment
The vast majority of simple elbow dislocations can be definitively treated without surgical intervention. Multiple studies over the past several years have compared surgical versus non-surgical management, the duration of immobilization and the type of immobilization used.11,12,14,15
In a publication from 1984, Josefsson et al re-examined 52 patients with a simple elbow dislocation treated with a period of immobilization at an average follow-up of 24 years after the injury. They noted that 50% of the patients had no residual signs or symptoms. However, approximately 35% of the patients had a slight or moderate loss of full extension, and this was found to be associated with early degenerative changes in the joint and/or periarticular calcification. At long-term follow-up, none of the 52 patients had suffered a redislocation. They concluded that dislocation of the elbow without an associated fracture, when treated by conservative methods, had a good prognosis in spite of the usually extensive damage to the periarticular structures.11 In another study, by Josefsson et al, 62 patients were followed for an average of 5 years following simple elbow dislocation. Thirty-four patients were treated non-operatively with closed reduction and immobilization in a plaster cast, while 28 patients were treated surgically with primary ligament repair followed by immobilization in plaster. Ligament repair was performed medially in all cases and laterally in only 17 at an average of 2 days following the injury. The authors found no significant difference in pain or range of motion between the two groups. As a result, they found no evidence to recommend primary surgical treatment of ligamentous injuries associated with simple elbow dislocations.12
In 1988, Mehlhoff et al published a series of 52 simple elbow dislocations treated with traditional closed reduction, but with varied duration of immobilization before initiating active motion. The average follow-up was 34.4 months. They noted that prolonged immobilization after the injury was strongly associated with an unsatisfactory result. Those immobilized for more than 25 days had significantly larger flexion contractures and more severe symptoms compared to patients immobilized for less than 2 weeks. As a result, they concluded that early active motion is crucial in rehabilitation of the elbow following a dislocation injury.1 Proztman et al published a series of 49 simple elbow dislocations and noted similar findings to Mehlhoff et al. Patients immobilized for less than 5 days had returned to full activity within an average of 6 weeks of the injury, with an average flexion contracture of 3°. They concluded that while the extremity is certainly more comfortable if immobilized for the first 7–10 days after injury, the price to be paid for that short-term comfort is a longer period of disability as well as an increased flexion contracture. They therefore recommended reduction followed by only 1–5 days of immobilization.13
In a study from the United States Naval Academy, Ross et al treated 21 simple elbow dislocations with closed reduction and immediate supervised active range of motion starting the day after injury. No splints or slings were used. The final range of motion averaged −4–139°, and all patients attained extension within 5° of the contralateral side. Each patient also obtained their final range of motion within an average of 19 days following reduction of the dislocation. One patient experienced a redislocation, and, at final follow-up there was only one case of recurrent instability that required surgical repair. The authors concluded that aggressive immediate motion rehabilitation allows nearly full elbow motion and an excellent functional outcome. It should be noted, however, that the United States Naval Academy has a select group of athletes as well as unique resources to deal with sports medicine injuries.14
Some authors have also recommended longer periods of immobilization following reduction of a simple elbow dislocation. Schippinger et al prospectively studied 45 patients with a simple elbow dislocation with an average follow-up of 61 months. All patients were treated by closed reduction and then randomized to a period of immobilization of less than 2 weeks, 2–3 weeks or more than 3 weeks. Although not statistically significant, they noted better pain and functional results in patients immobilized for less than 3 weeks. The authors suggested that immobilizing for 2 weeks enhances patient comfort by allowing rapid subsidence of swelling and providing pain relief, and does not adversely affect the eventual outcome.16
A recent review article by Cohen et al recommended splinting simple elbow dislocations in approximately 90° of flexion for 5–10 days following radiographically verified reduction. As the unstable elbow can redislocate even in a well-moulded splint or cast, repeat radiographs should be obtained at 3–5 days and again at 10–14 days to ensure maintenance of reduction. They then recommend initiating range-of-motion exercises with interval splinting for comfort and support. Extension is gradually increased over the subsequent 3–6 weeks. Vigorous passive motion is avoided as it can cause swelling and pain and may be associated with the development of ectopic ossification.10
Some studies have also evaluated the types of non-operative treatment available. In a recent report by DeHaan et al, a meta-analysis was performed to identify the best available treatment for simple elbow dislocations. Two randomized controlled trials and six observation comparative studies were included with a total enrolment of 342 patients. The authors noted a better range of motion, less pain, better functional scores, shorter disability and shorter treatment time after functional treatment with a sling and early range of motion compared to plaster immobilization. Of the 342 simple dislocations, there was only one redislocation (0.3%). The authors recommended assessing the elbow for instability after reduction of the dislocation by valgus and varus testing and by the lateral pivot shift test. When the elbow is considered stable, functional treatment rather than plaster immobilization is advocated.2 Maripuri et al came to similar conclusions when retrospectively reviewing 42 simple elbow dislocations treated with either plaster immobilization or a sling with early mobilization. They noted significantly better functional outcomes in the sling and early mobilization group compared to the plaster immobilization group.15
If the patient is started on active contraction of the biceps and triceps, the ‘drop sign’ will resolve over a period of several weeks in the majority of patients. In a series of 23 patients, Duckworth et al showed that residual subluxation may occur following both operative and non-operative treatment. Patients started in active elbow flexion exercises while avoiding shoulder abduction and varus stresses demonstrated resolution of the ‘drop sign’ on follow-up radiographs. At a 2-year follow-up, the arc of motion averaged 20–132° with average pronation of 78° and average supination of 64°.17
Operative treatment
Recurrent instability following simple elbow dislocations is extremely rare, and occurs in only 1–2% of cases.1,12,18 Redislocation of the elbow with passive range of motion or redislocation in plaster immobilization implies severe valgus instability with disruption of some aspect of the lateral collateral ligament complex. In these situations and when clinical examination demonstrates recurrent elbow instability in 30° of flexion surgical treatment should be considered.
Repair of the lateral ligament complex will normally restore elbow stability and it is rarely necessary to address the medial collateral ligaments. McKee et al defined the pattern of soft tissue disruption of the lateral soft tissue structures in patients requiring operative repair for a dislocation or fracture–dislocation. They concluded that repair of the lateral soft tissue structures should be an integral part of the surgical strategy for elbow dislocations requiring surgical treatment.19
Outcomes and complications
Most patients who sustain a simple elbow dislocation can be treated non-operatively and regain function with an adequate arc of motion. Lansinger et al reported good to excellent results in 75–100% of patients at long-term follow-up.20 However, because there is significant injury to the soft tissues, some patients continue to complain of persistent pain, loss of motion and instability. The most common complications following a simple elbow dislocation are stiffness, instability and heterotopic ossification.
Stiffness (see also Ch. 28)
Elbow stiffness is thought to occur due to thickening and fibrosis of the anterior joint capsule. It has been reported that most patients lose the terminal 10–15° of elbow extension following a dislocation.10 Josefsson et al followed 52 patients for an average of 24 years following simple elbow dislocations and noted an average loss of elbow extension of 12°. Some of these patients, however, were unaware of the reduction in their range of extension. The authors also noted that patients who sustained a lateral dislocation had a somewhat greater loss of extension, although this difference was not statistically significant.11 Early active mobilization may be helpful in reducing this complication.
Many authors have recommended the use of dynamic elbow splints if motion is not steadily improving within 4–6 weeks of the injury. If the stiffness is severe, surgical intervention is indicated. It is generally considered that patients require an arc of motion from 30° short of full extension to 130° of flexion (100° of motion) for activities of daily living. Husband et al used a lateral approach to release post-traumatic elbow contractures in seven patients and achieved an average increase in the arc of motion of 46°.21
Instability (see also Chs 25–27)
Insufficiency of the lateral elbow ligaments can lead to subtle instability of the elbow following dislocation. This is known as valgus posterolateral rotatory instability. Without lateral stabilization there is insufficient lateral joint support to hold the ulna reduced to the humerus and the ulna sags.22 In this situation, the ulnohumeral joint does not dislocate but rather pivots, opening up laterally in supination.23 Lateral radiographs reveal posterior translation of the radial head with widening of the ulnohumeral joint space. This can be accentuated with the elbow in supination, and the deformity reduces with forearm pronation.
It is known that all simple elbow dislocations result in rupture of the medial and lateral collateral ligament complexes. Josefsson et al evaluated 31 patients with a diagnosis of a simple elbow dislocation. The authors examined all elbows under anaesthesia, followed by surgical exploration at an average of 2 days after the injury. Valgus instability was noted in 100% of the elbows, and varus instability was apparent in 26% of the elbows. Approximately 29% of the elbows were easily redislocated under general anaesthesia. Subsequent surgical exploration of the medial collateral ligament complex was performed in all 31 patients and exploration of the lateral collateral ligament complex was performed in 18 patients. The authors noted the medial collateral ligament was totally ruptured or avulsed in all 31 cases, and all 18 laterally explored elbows also demonstrated complete rupture or avulsion of the lateral collateral ligament complex. In addition, the degree of muscular damage was correlated with the tendency to redislocate under anaesthesia.24
Evaluation of both the medial and lateral ligaments is best done under fluoroscopic guidance.
If a patient has clinical and/or radiographic evidence of lateral elbow instability after a simple elbow dislocation, they should avoid forearm supination for a period of several weeks to allow adequate healing of the lateral collateral ligament complex. Either a hinged elbow orthosis or a cast brace that keeps the forearm in pronation can be used. Reconstruction of the lateral collateral ligament complex is indicated in patients with symptomatic instability of the elbow.25
Heterotopic ossification
In a retrospective review of 62 simple elbow dislocations, Josefsson et al noted heterotopic ossification in 76% of patients at long-term follow-up. The most common sites of periarticular calcification were anterior, medial and/or lateral to the elbow joint. The authors also noted a strong correlation between the presence of the heterotopic ossification and the loss of extension of approximately 10°. However, this was only noted in patients with lesions medially and/or laterally.12
Heterotopic ossification is usually evident on radiographs within 4–6 weeks of injury (Fig. 24.4). It is often associated with closed head injury, delayed surgical intervention and aggressive passive joint manipulation after dislocation.10 In high risk patients, prophylaxis with a non-steroidal antiinflammatory medication, bisphosphonate or low-dose radiation should be considered. If the heterotopic ossification remains symptomatic, operative resection can be discussed. Most surgeons allow the process to mature before considering operative resection. This often occurs between 3 and 4 months following injury. Recurrence, if it occurs, is usually minor following surgical excision.
1 Mehlhoff TL, Noble PC, Bennett JB, et al. Simple dislocation of the elbow in the adult: results after closed treatment. J Bone Joint Surg Am. 1988;70:244-249.
2 DeHaan J, Schep NW, Tuinebreijer WE, et al. Simple elbow dislocations: a systematic review of the literature. Arch Orthop Trauma Surg. 2010;130:241-249.
3 Josefsson PO, Nilsson BE. Incidence of elbow dislocation. Acta Orthop Scand. 1986;57:537-538.
4 Durig M, Muller W, Ruedi TP, et al. The operative treatment of elbow dislocation in the adult. J Bone Joint Surg Am. 1979;61:239-244.
5 Dunning CE, Zarzour ZD, Patterson SD, et al. Ligamentous stabilizers against posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 2001;83:1823-1828.
6 Wadstrom J, Kinast C, Pfeiffer K. Anatomical variations of the semilunar notch in elbow dislocations. Arch Orthop Trauma Surg. 1986;105:313-315.
7 Slowik GM, Fitzimmons M, Rayhack JM. Closed elbow dislocation and brachial artery damage. J Orthop Trauma. 1993;7:558-561.
8 Lim D, Hodkinson SL, Brown RF. Median nerve palsy after posterolateral elbow dislocation. J Bone Joint Surg Br. 1994;76:987-988.
9 Morrey BF, editor. The elbow and its disorders, 2nd ed, Philadelphia, PA: WB Saunders, 1993.
10 Cohen MS, Hastings HII. Acute elbow dislocation: evaluation and management. J Am Acad Orthop Surg. 1998;6:15-23.
11 Josefsson PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am. 1984;66:927-930.
12 Josefsson PO, Gentz CF, Johnell O, et al. Surgical versus nonsurgical treatment of ligamentous injuries following dislocations of the elbow joint. Clin Orthop. 1987;214:165-169.
13 Protzman RR. Dislocation of the elbow joint. J Bone Joint Surg Am. 1978;60:539-541.
14 Ross G, McDevitt ER, Chronister R, et al. Treatment of simple elbow dislocation using an immediate motion protocol. Am J Sports Med. 1999;27:308-311.
15 Maripuri SN, Debnath UK, Rao P, et al. Simple elbow dislocation among adults: a comparative study of two different methods of treatment. Injury. 2007;38:1254-1258.
16 Schippinger G, Seibert FJ, Steinbock J, et al. Management of simple elbow dislocations. Langenbeck’s. Arch Surg. 1999;384:294-297.
17 Duckworth AD, Kulijdian A, McKee MD, et al. Residual subluxation of the elbow after dislocation or fracture–dislocation: treatment with active elbow exercises and avoidance of varus stress. J Shoulder Elbow Surg. 2008;17:276-280.
18 Josefsson PO, Gentz CF, Johnell O, et al. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint: a prospective randomized study. J Bone Joint Surg Am. 1987;69:605-608.
19 McKee MD, Schemitsch EH, Sala MJ, et al. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg. 2003;12:391-396.
20 Lansinger O, Karlsson J, Korner L, et al. Dislocation of the elbow joint. Arch Orthop Trauma Surg. 1984;102:183-186.
21 Husband JB, Hastings HII. The lateral approach for operative release of post-traumatic contracture of the elbow. J Bone Joint Surg Am. 1990;72:1353-1358.
22 Cohen MS, Hastings HII. Rotatory instability of the elbow: the role of the lateral stabilizers. J Bone Joint Surg Am. 1997;79:225-233.
23 O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73:440-446.
24 Josefsson PO, Johnell O, Wendeberg B. Ligamentous injuries in dislocations of the elbow joint. Clin Orthop. 1987;221:221-225.
25 Mehta JA, Bain GI. Posterolateral rotatory instability of the elbow. J Am Acad Orthop Surg. 2004;12:405-415.