Acquired Biliary Tract Disease
Cholelithiasis and Choledocholithiasis
Overview: Although in the past cholelithiasis was believed to be rare in children without hemolytic anemia, it is being diagnosed more frequently as a result of increased utilization of sonography. In fact, the sonographic finding of gallstones has been reported in fetuses, although most of these gallstones resolve spontaneously.1
Etiology: Development of gallstones in infants may be related to immature physiologic regulation of bile salt secretion. Chronic cholestasis likely plays a role in the pathophysiology of cholelithiasis. Although gallstones in infants often are discovered incidentally, many predisposing conditions have been described (Box 89-1). Gallstones in infants resolve spontaneously less often than in fetuses. Further, stones in infants are rarely complicated by biliary tract perforation and peritonitis.2
Although most of the stones seen in older children are idiopathic, a number of underlying states have been associated with gallstones (Box 89-2). Prominent among these states are sickle cell disease and intestinal problems that interfere with normal enterohepatic circulation.3 Patients with sickle cell disease and other hemolytic anemias have an increased incidence of gallstones with advancing age. Gallstones also have been reported after surgery and antibiotic therapy.4
Clinical Presentation: Cholelithiasis usually is asymptomatic in infants and young children, with an increased incidence of symptoms in older children. When symptoms occur in older children and adolescents, they are similar to those seen in adults and include bloating, nausea, vomiting, and postprandial right upper quadrant colicky pain radiating to the shoulder. In younger children the presentation may be nonspecific (such as irritability), because young children may not be able to verbalize or relate their discomfort to the right upper quadrant or to a recent meal.5
Choledocholithiasis results from migration of stones from the gallbladder into the common duct. Stones are more likely to be symptomatic when they pass into the cystic duct or the common bile duct. The most common complication of gallstones in children is pancreatitis,5 although the most common cause of pancreatitis is idiopathic or posttraumatic.6
Imaging: Although radiolucent cholesterol stones are the most common type overall, they are rare in children, and thus the majority of pediatric gallstones are visible radiographically. Even so, sonography remains the primary imaging modality for the evaluation of cholelithiasis (Fig. 89-1). Three main sonographic criteria are used to diagnose gallstones: (1) echogenic focus, (2) acoustic shadowing, and (3) gravitational dependence. Most stones move with change in patient position, which should be a routine maneuver during hepatobiliary sonography (Fig. 89-2). Four general sonographic patterns of cholelithiasis are described. The first pattern includes the simple echogenic, shadowing, mobile stone, which may be single or multiple. The second pattern of cholelithiasis describes collections of very tiny, sandlike stones, termed milk of calcium, which may mimic gallbladder sludge; acoustic shadowing may be seen only in the aggregate (see Fig. 89-2).7 Occasionally, if bile within the gallbladder is of high density, the stones may seem to float on the surface, giving an apparent fluid-fluid level. The last sonographic pattern of cholelithiasis relates to stones within a contracted gallbladder, in which case the stones produce an echogenic double arc known as the wall echo shadow (WES) complex. This pattern may be seen in patients with a chronically contracted gallbladder or those who have not fasted sufficiently (Fig. 89-3). Careful scrutiny must be used so as not to confuse the WES complex with emphysematous cholecystitis (air in the gallbladder wall), which is far more common in adults than in children.8

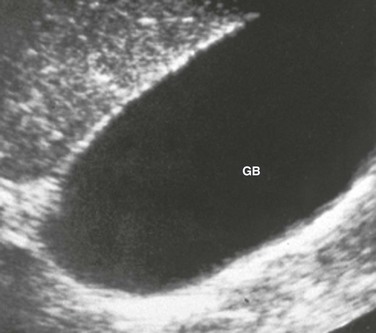
Figure 89-1 Cholelithiasis in a 17-year-old girl with abdominal pain.
A transverse sonogram of the gallbladder shows cholelithiasis (arrow) with associated posterior acoustic shadowing (S).
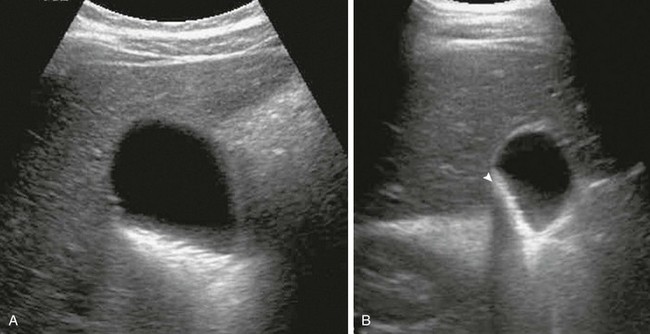
Figure 89-2 Cholelithiasis in a 16-year-old girl with right upper quadrant pain.
Transverse sonograms in the supine (A) and decubitus (B) positions reveal echogenic layering of tiny stones. Note the change in stones with change in patient position, as well as diffuse shadowing of the stone aggregate (arrowhead in B).
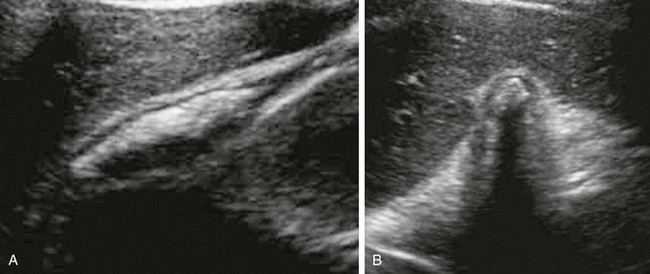
Figure 89-3 Cholelithiasis in a 16-year-old girl with abdominal pain.
Longitudinal (A) and transverse (B) sonograms performed without fasting show the anterior gallbladder wall and multiple echogenic stones with posterior acoustic shadowing (wall-echo-shadow triad).
Sonography is less successful at revealing choledocholithiasis than it is at detecting cholelithiasis because of interference from gas in adjacent bowel. Therefore dilated extrahepatic bile ducts (Fig. 89-4) may be the only sonographic sign of a more distal obstructing stone. Computed tomography (CT) scans9 might be obtained in children with biliary stones if other abdominal processes initially are clinically suspected. CT is inferior to sonography with regard to revealing the actual stone, but it readily demonstrates biliary dilation.6 If no stone is seen on sonography yet evidence exists of biliary ductal dilation, magnetic resonance cholangiopancreatography (MRCP) may be helpful. With MRCP, stones are seen as low signal intensity filling defects within the gallbladder and the biliary tree (Figs. 89-5 and 89-6).10
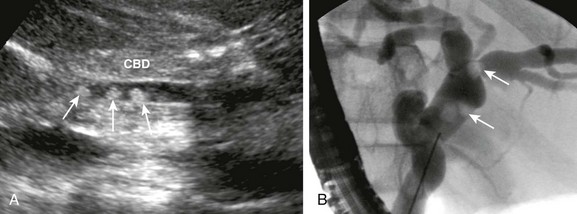
Figure 89-4 Choledocholithiasis in a 15-year-old girl with sickle cell disease and abdominal pain.
A, Sonogram of the common bile duct (CBD) reveals three stones (arrows). B, Subsequent endoscopic retrograde cholangiopancreatography shows dilated bile ducts and intraluminal filling defects (arrows).

Figure 89-5 Choledocholithiasis in a 17-year-old boy with Duchenne muscular dystrophy and jaundice.
Three-dimensional reformatted T2-weighted sequences from a magnetic resonance cholangiopancreatogram show a filling defect consistent with a stone (arrow) in the distal common bile duct. A small stone was removed at subsequent endoscopic retrograde cholangiopancreatography.
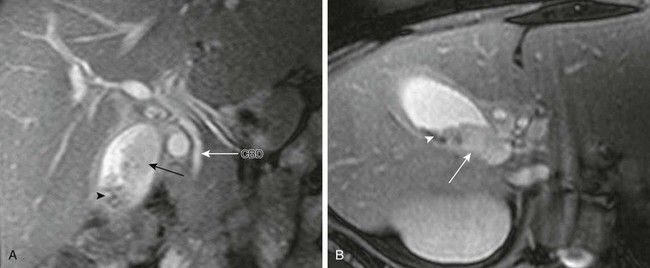
Figure 89-6 Cholelithiasis in a 12-year-old girl with abdominal pain.
Coronal (A) and axial T2-weighted (B) magnetic resonance images reveal low signal intensity gallstones (arrowheads) and isointense sludge (arrows) within the gallbladder lumen. Note the normal common bile duct (CBD) (long white arrow in A).
Biliary Sludge
Overview: The clinical significance of biliary sludge, which is particulate matter within the bile produced by cholestasis, is debated. Although most biliary sludge is a transient finding, particularly if it is associated with a transient predisposing condition, it may evolve into gallstones.12
Etiology: Sludge is formed predominantly of calcium bilirubinate particles and, depending on the underlying process, cholesterol crystals. Predisposing conditions that share the common pathway of biliary stasis include biliary outflow obstruction, intravenous hyperalimentation, hemolysis, and prolonged fasting.13
Clinical Presentation: Biliary sludge usually is asymptomatic; however, it may cause symptoms, particularly if it is associated with microlithiasis or if “bile balls” migrate into the biliary ducts. When this migration happens, symptoms occur that are similar to those seen in patients with cholelithiasis.12
Imaging: On sonography, sludge is echogenic without acoustic shadowing; it typically layers in the dependent portion of the gallbladder or other part of the biliary tree (such as a choledochal cyst) and demonstrates a fluid-sludge level (Fig. 89-7). Occasionally sludge coalesces within the gallbladder lumen, forming a tumefactive “sludge ball” that, when fixed, may mimic a polyp or mass.8 Differential considerations include uncommon conditions such as hemobilia, biliary mucus, and parasitic infection.
Treatment and Follow-up: Because biliary sludge generally is asymptomatic and resolves spontaneously with resolution of the underlying condition, it does not require separate treatment. However, follow-up in patients in whom the underlying condition does not remit is important to assess for resolution or evolution, particularly if the patient becomes symptomatic.12
Acute Cholecystitis
Overview: Acute cholecystitis is uncommon in infants and children compared with adults. However, the mortality rate is at least 30% because of concomitant disease and the potential for rapid progression, with gallbladder gangrene occurring in more than 50% of cases and perforation in more than 10% of cases.14
Etiology: Cholecystitis develops in a small percentage of children with cholelithiasis, and acute acalculous cholecystitis represents 50% to 70% of all cases of cholecystitis in children.15 In most cases, the pathophysiology of acute cholecystitis involves obstruction of the cystic duct, which leads to gallbladder distention, followed successively by edema, ischemia, mural necrosis, and, in severe cases, perforation. The pathophysiology of acalculous cholecystitis is thought to involve biliary stasis, dehydration, gallbladder ischemia, and elevated ampullary pressures as contributing factors.14 In neonates with acute cholecystitis, the diagnosis may not be suspected, leading to a high mortality rate.
Clinical Presentation: Making a diagnosis in cases of acalculous cholecystitis can be difficult. The condition is most dangerous when it occurs during a serious illness, and the development of symptoms and laboratory abnormalities (such as fever and leukocytosis) initially may be masked by the underlying condition. Patients who may experience acalculous cholecystitis include those with septicemia, postoperative patients, and patients who have sustained severe trauma or burns. Systemic infection may be more common in pediatric patients. Symptoms include jaundice, nausea, vomiting, and tenderness to palpation.12,14–16
Imaging: Urgent imaging of possible acute cholecystitis is useful for rendering a diagnosis, determining the severity of disease, and discovering other potential causes of abdominal pain. Sonography is the initial imaging modality of choice, particularly to evaluate for gallstones and biliary obstruction.
The sonographic findings of calculous and acalculous cholecystitis are identical except for the lack of gallstones in the latter condition. Sonographic findings of cholecystitis when viewed individually are nonspecific, but when combined they may indicate a specific diagnosis. The best indicators of acute cholecystitis include cholelithiasis, a sonographic Murphy sign (tenderness when the gallbladder is compressed), and gallbladder wall edema with wall thickening greater than 3.5 mm (Fig. 89-8).14,17 Intramural edema related to acute cholecystitis is usually striated, with multiple interrupted bands of hypoechogenicity. This appearance also has been associated with gangrenous cholecystitis. The interrupted layers of intramural edema seen with acute cholecystitis should not be confused with homogeneous gallbladder wall thickening, a common nonspecific finding seen in a variety of disorders such as ascites, hypoalbuminemia, congestive heart failure, hepatitis, portal hypertension, and gallbladder wall varices. Other sonographic findings of acute cholecystitis include gallbladder distention, pericholecystic fluid (especially with perforation), adjacent rim of hypoechogenicity or hypervascularity in the liver, biliary sludge, and, rarely, dirty shadowing as a result of air-producing infection (found most often in adults with diabetes). CT is not the modality of choice in most pediatric patients with cholecystitis, but if it is performed for other reasons, it shows similar findings (Fig. 89-9).

Figure 89-8 Acute cholecystitis in a 15-year-old girl with a history of cholelithiasis.
A transverse sonogram through the gallbladder reveals a markedly thickened and edematous gallbladder wall with echogenic material in the lumen. The patient had a history of chronic, recurrent abdominal pain.
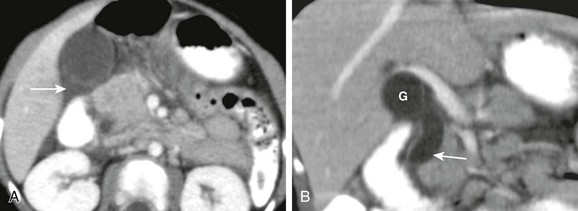
Figure 89-9 Cholecystitis and ascending cholangitis in a 25-month-old boy with subsequent confirmed passage of a gallstone.
A, Axial image from a contrast-enhanced computed tomography scan of the abdomen demonstrates pericholecystic edema (arrow) on the axial image. B, A coronal reformatted image demonstrates a distended gallbladder (G) and dilation of the common bile duct (arrow).
Hepatobiliary scintigraphy with technetium-99m–labeled iminodiacetic acid derivative is highly sensitive for the diagnosis of acute cholecystitis in adults and children. Normally, the gallbladder is opacified with a radiopharmaceutical agent in the first 30 minutes of the study or in the first hour with slow injection of intravenous morphine (which increases pressure in the sphincter of Oddi). However, with acute cholecystitis, gallbladder opacification does not occur. Occasionally a rim of increased activity is seen in the liver surrounding the gallbladder (the rim sign), and peritoneal activity may be seen with perforation (Fig. 89-10).18
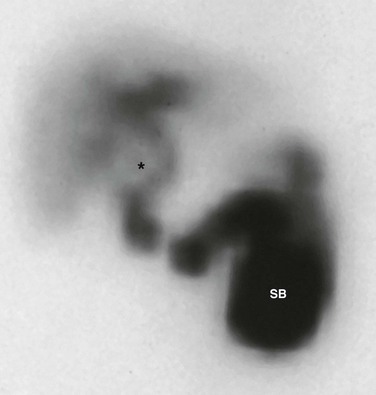
Figure 89-10 Acute cholecystitis in a 15-year-old girl with a history of cholelithiasis (same patient as in Fig. 89-8).
A 4-hour image from a biliary patency scan shows hepatic uptake and excretion of technetium-99m–labeled iminodiacetic acid into the biliary tree and small bowel (SB) without gallbladder (asterisk) opacification. A halo of increased activity known as the rim sign surrounds the gallbladder fossa indicating hyperemia.
Treatment and Follow-up: Treatment for acute acalculous cholecystitis may differ depending on the patient’s clinical status and underlying conditions. Children may be treated medically and observed prior to surgery.16,19 Percutaneous cholecystostomy is increasingly a lifesaving, minimally invasive alternative. Gallbladder perforation is a surgical emergency that occurs in 3% to 15% of patients with acute cholecystitis.20
Cholangitis
Overview: Cholangitis, or ascending cholangitis, refers to biliary duct obstruction with associated biliary infection. Primary sclerosing cholangitis (PSC) is a noninfectious idiopathic obliterative inflammatory fibrosis of the biliary tree.
Etiology: Causes of ascending cholangitis are numerous and range from neoplasms (benign and malignant) to infection (suppurative, nonsuppurative, and human immunodeficiency virus) to autoimmune or chemotherapy-induced disorders. Appropriate therapy is directed toward relief of the underlying cause of obstruction, whether congenital or acquired.
The features of PSC suggest an autoimmune mechanism, but the pathophysiology of tissue damage has not been definitively determined. Associated disorders include inflammatory bowel disease, in particular ulcerative colitis (47%), idiopathic causes (24%), Langerhans cell histiocytosis (15%), and other immune system disorders (10%).21 PSC also has been associated with cystic fibrosis.
Clinical Presentation: Boys are affected more often than girls and typically present in the second decade of life. Presentation is with jaundice, abdominal pain, and hepatomegaly. Alkaline phosphatase levels may be within normal limits. As many as 81% of patients may have underlying irritable bowel disease, possibly subclinical.22
Imaging: With use of sonography, nonspecific dilation of the biliary system, hyperechoic portal triads, portal casts, thickened gallbladder wall, and cholelithiasis may be identified in persons with PSC. CT findings include focal dilation of the biliary tree and contrast enhancement of the bile duct walls caused by inflammatory changes. Magnetic resonance imaging may reveal peripheral wedge-shaped areas of high T2 signal in association with dilated bile ducts. T1 and T2 shortening along the periportal triads as a result of inflammation also may be detected. Key findings on cholangiopancreatography include multifocal stricture of the biliary tree with alternating areas of dilation, forming a classic “string of beads” appearance. Additional findings include the pruned-tree pattern (dilation limited to central ducts), cobblestone appearance (coarse mural irregularities), and pseudodiverticula (Fig. 89-11). MRCP has been found to be 84% sensitive and accurate in the diagnosis of PSC.23
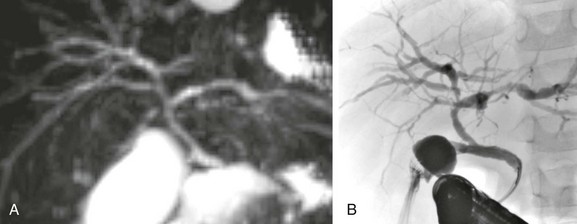
Figure 89-11 Sclerosing cholangitis in an adolescent boy with ulcerative colitis.
A, Magnetic resonance cholangiopancreatography demonstrates irregularity, narrowing, and ductal beading throughout the biliary system. B, Endoscopic retrograde cholangiopancreatography in another patient demonstrates areas of abnormal biliary ductal dilation and strictures throughout the biliary duct system consistent with sclerosing cholangitis. (A, Courtesy Dr. Marta Hernanz-Schulman, MD, Nashville, TN.)
Although cholangitis occasionally is segmental, the entire biliary tract usually is involved and intrahepatic biliary duct involvement is seen in 100% of cases, whereas the extrahepatic ducts are involved in 60% of cases.24 The gallbladder is rarely involved.
Treatment and Follow-up: Complications of sclerosing cholangitis include portal hypertension, biliary cirrhosis, secondary cholangitis, and cholangiocarcinoma. Treatment is aimed at palliation and may include medical therapy (such as ursodeoxycholic acid to promote bile flow), interventional dilation of strictures, and drainage of infected obstructed ducts. The median reported time for liver transplantation is approximately 12.7 years from initial diagnosis.22,25
Hydrops of the Gallbladder
Etiology: Gallbladder hydrops is thought to be related to transient cholestasis and obstruction of the biliary tree and usually is associated with preceding infectious disorders elsewhere in the body (Box 89-3), most notably mucocutaneous lymph node syndrome (Kawasaki disease) and parenteral hyperalimentation.
Clinical Presentation: Hydrops of the gallbladder is more frequent in boys and usually presents in children ages 17 months to 7 years. Presentation may include jaundice, abdominal pain, right upper quadrant tenderness, vomiting, or a palpable mass.26
Imaging: Sonography is the modality of choice in patients suspected of gallbladder hydrops. The findings consist of gallbladder dilation without gallbladder wall thickening. The gallbladder may resemble a balloon in which normal contours are lost (Fig. 89-12). A normal gallbladder length is 1.5 to 3 cm in infants (<1 year old) and 3 to 7 cm in older children.27 Sludge is seen in some cases, and the biliary tree is otherwise normal. Serial sonographic studies may demonstrate resolution.28
Albuquerque, PA, Morales Ramos, DA, Faingold, R. Magnetic resonance imaging of the liver and biliary tree in children. Curr Probl Diagn Radiol. 2009;38(3):126–134.
Anupindi, SA. Pancreatic and biliary anomalies: imaging in 2008. Pediatr Radiol. 2008;38(suppl 2):S267–S271.
Lowe, LH. Hepatobiliary disease in children. Semin Roentgenol. 2008;43(1):39–49.
References
1. Suma, V, Marini, A, Bucci, N, et al. Fetal gallstones: sonographic and clinical observations. Ultrasound Obstet Gynecol. 12(6), 1998. [439-434].
2. Gubernick, JA, Rosenberg, HK, Llaslan, H, et al. US approach to jaundice in infants and children. Radiographics. 2000;20(1):173–195.
3. Darge, K, Anupindi, S. Pancreatitis and the role of US, MRCP and ERCP. Pediatr Radiol. 2009;39(suppl 2):S153–S157.
4. Bogue, CO, Murphy, AJ, Gerstle, JT, et al. Risk factors, complications, and outcomes of gallstones in children: a single-center review. J Pediatr Gastroenterol Nutr. 2010;50(3):303–308.
5. Reif, S, Sloven, DG, Lebenthal, E. Gallstones in children. Characterization by age, etiology, and outcome. Am J Dis Child. 1991;145(1):105–108.
6. Shanbhogue, AK, Fasih, N, Surabhi, VR, et al. A clinical and radiologic review of uncommon types and causes of pancreatitis. Radiographics. 2009;29(4):1003–1026.
7. Wu, SS, Casas, AT, Abraham, SK, et al. Milk of calcium cholelithiasis in children. J Pediatr Surg. 2001;36(4):644–647.
8. Rosenthal, SJ, Cox, GG, Wetzel, LH, et al. Pitfalls and differential diagnosis in biliary sonography. Radiographics. 1990;10(2):285–311.
9. Emery, KH. Cross-sectional imaging of pediatric biliary disorders. Pediatr Radiol. 2010;40(4):438–441.
10. Anupindi, SA, Victoria, T. Magnetic resonance cholangiopancreatography: techniques and applications. Magn Reson Imaging Clin North Am. 2008;16(3):453–466.
11. Chan, S, Currie, J, Malik, AI, et al. Paediatric cholecystectomy: shifting goalposts in the laparoscopic era. Surg Endosc. 2008;22(5):1392–1395.
12. Jungst, C, Kullak-Ublick, GA, Jungst, D. Gallstone disease: microlithiasis and sludge. Best Pract Res Clin Gastroenterol. 2006;20(6):1053–1062.
13. Mitchell, CL, Vasanawala, SS. An approach to pediatric liver MRI. AJR Am J Roentgenol. 2011;196(5):W519–W526.
14. Barie, PS, Fischer, E. Acute acalculous cholecystitis. J Am Coll Surg. 1995;180(2):232–244.
15. Tsakayannis, DE, Kozakewich, HP, Lillehei, CW. Acalculous cholecystitis in children. J Pediatr Surg. 1996;31(1):127–130. [discussion 130-131].
16. Imamoglu, M, Sarihan, H, Sari, A, et al. Acute acalculous cholecystitis in children: diagnosis and treatment. J Pediatr Surg. 2002;37(1):36–39.
17. Deitch, EA, Engel, JM. Acute acalculous cholecystitis. Ultrasonic diagnosis. Am J Surg. 1981;142(2):290–292.
18. Mariat, G, Mahul, P, Prév, tN, et al. Contribution of ultrasonography and cholescintigraphy to the diagnosis of acute acalculous cholecystitis in intensive care unit patients. Intensive Care Med. 2000;26(11):1658–1663.
19. Glenn, F, Becker, CG. Acute acalculous cholecystitis. An increasing entity. Ann Surg. 1982;195(2):131–136.
20. Granlund, A, Karlson, BM, Elvin, A, et al. Ultrasound-guided percutaneous cholecystostomy in high-risk surgical patients. Langenbecks Arch Surg. 2001;386(3):212–217.
21. Sisto, A, Feldman, P, Garel, L, et al. Primary sclerosing cholangitis in children: study of five cases and review of the literature. Pediatrics. 1987;80(6):918–923.
22. Feldstein, AE, Perrault, J, El-Youssif, M, et al. Primary sclerosing cholangitis in children: a long-term follow-up study. Hepatology. 2003;38(1):210–217.
23. Chavhan, GB, Roberts, E, Moineddin, R, et al. Primary sclerosing cholangitis in children: utility of magnetic resonance cholangiopancreatography. Pediatr Radiol. 2008;38(8):868–873.
24. Debray, D, Pariente, D, Urvoas, E, et al. Sclerosing cholangitis in children. J Pediatr. 1994;124(1):49–56.
25. Ibrahim, SH, Lindor, KD. Current management of primary sclerosing cholangitis in pediatric patients. Paediatr Drugs. 2011;13(2):87–95.
26. Egritas, O, Nacar, N, Hanioglu, S, et al. Early but prolonged gallbladder hydrops in a 7-month-old girl with Kawasaki syndrome: report of a case. Surg Today. 2007;37(2):162–164.
27. Rozel, C, Garel, L, Rypens, F, et al. Imaging of biliary disorders in children. Pediatr Radiol. 2011;41(2):208–220.
28. Neu, J, Arvin, A, Ariagno, RL. Hydrops of the gallbladder. Am J Dis Child. 1980;134(9):891–893.
29. Suddleson, EA, Reid, B, Woolley, MM, et al. Hydrops of the gallbladder associated with Kawasaki syndrome. J Pediatr Surg. 1987;22(10):956–959.