Above-Knee and Below-Knee Amputation
Surgical Principles
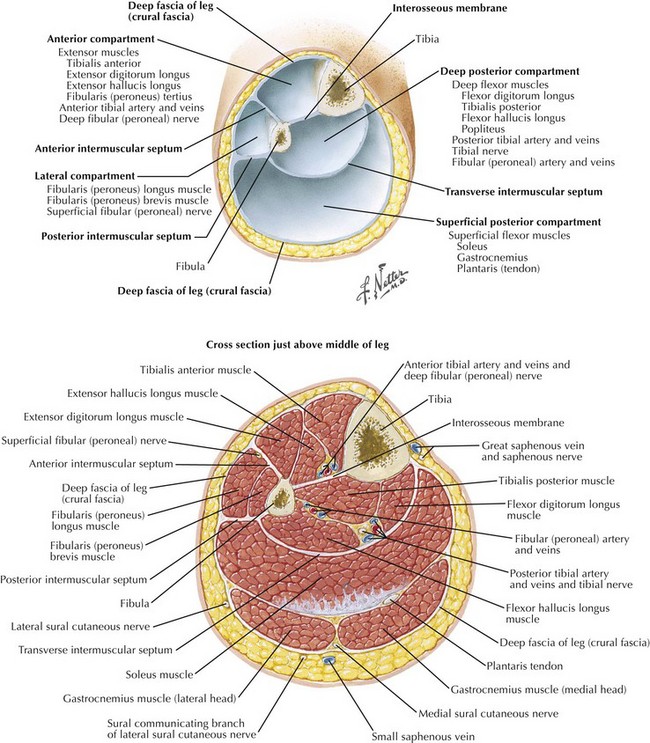
Use of immediate postoperative prosthesis (IPOP) typically is surgeon and institution specific. IPOP allows for early weight bearing and ambulation and is well suited for younger, motivated patients. The goal of operation is to provide a healed wound with a stump that can fit into a prosthetic limb. For BKA, the long posterior myocutaneous flap is typically used, although circular and fish-mouth incisions may be necessary with wounds in or on the calf. Newer prosthetic techniques allow for mediolateral or anteroposterior flaps with good functional outcome. The importance of identifying the fascial layers for closure and meticulous handling of the tissues should be emphasized (Fig. 39-1).
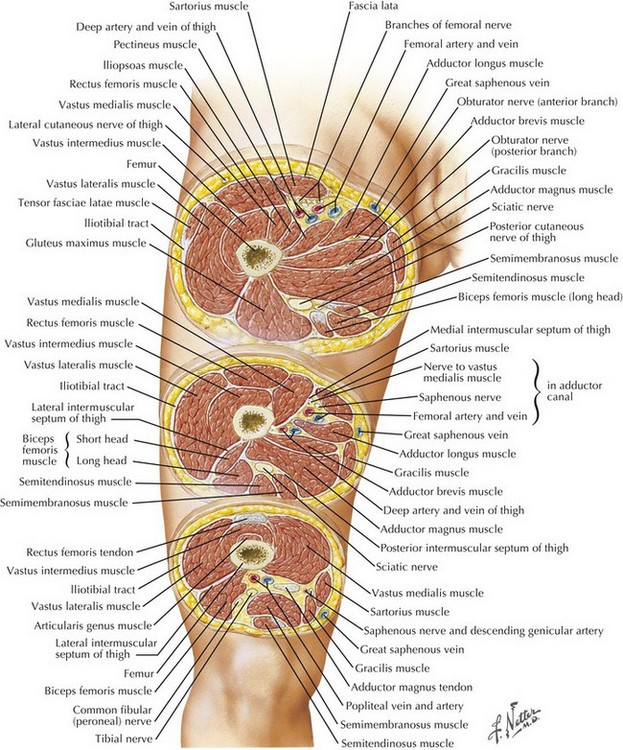
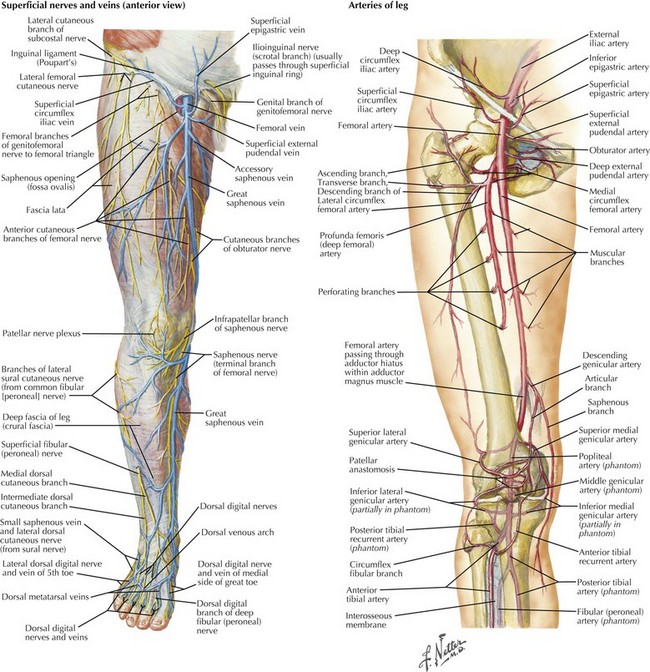
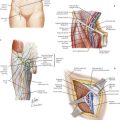
The length of the stump depends on preoperative functional status with expected postoperative potential for prosthetic fitting, but usually the tibial transection is made about 10 cm beyond the tibial tuberosity. For AKA, it is preferable to leave the residual femur as long as possible, except in nonambulatory patients with severe peripheral vascular disease who undergo AKA for palliation of pain or nonhealing ulcers and may benefit from a shorter stump to maximize healing potential. Understanding the bony landmarks, arterial supply, nerves, and compartments of the lower extremity is essential to perform an appropriate procedure (Figs. 39-2 and 39-3).
Below-Knee Amputation
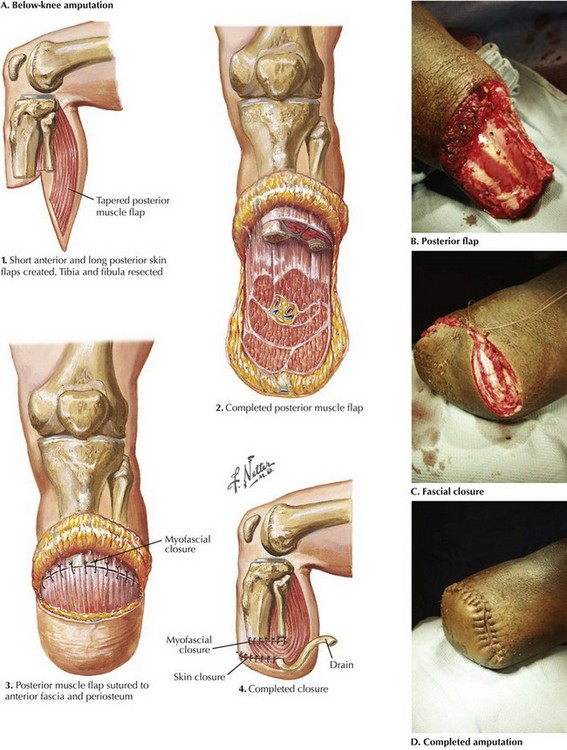
The myocutaneous skin flap can be measured or created freehand. For a typical posterior flap in below-knee amputation (BKA), the anterior skin incision is made approximately 10 cm below in the tibial tuberosity to the level of the fascia (Fig. 39-4, A).
The tibia is then transected at approximately the level of the skin incision by using a power saw (Fig. 39-4, B). The anterior tibia is beveled 60 degrees. The fibula is then transected 1 to 2 cm proximal to the tibia. This technique permits exposure of the posterior tibial and peroneal neurovascular bundles, which are individually ligated.
The posterior flap in BKA is fashioned with an amputation knife or cautery. Strict hemostasis is achieved; placement of a drain is optional. Closure is performed with absorbable fascial sutures. Special care is taken with the skin closure, using staples or nonabsorbable vertical mattress sutures (Fig. 39-4, C and D). A well-padded sterile dressing is applied. IPOP is an option in younger, highly motivated patients. Other BKA patients may benefit from a rapidly removable cast or knee immobilizer to minimize contracture.
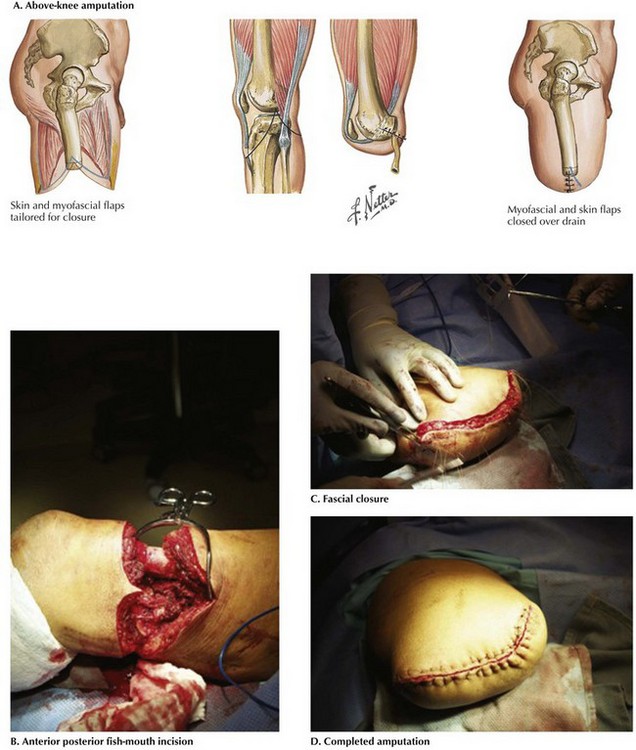
Above-Knee Amputation
The most common closure in above-knee amputation (AKA) is an anteroposterior fish-mouth incision, but as in BKA, this can be modified to obtain adequate tissue coverage (Fig. 39-5, A). A short fish-mouth incision minimizes the length of incision in AKA. The incision is carried down to the level of the fascia, which is transected. The quadriceps muscles are transected with Bovie cautery. Medial division of the sartorius muscle allows entry into the popliteal fossa, where the superficial femoral artery and vein are ligated and transected. The sciatic nerve is deep to these vessels and should be ligated and divided separately. Laterally, the iliotibial band and intermuscular septum are divided, along with the large lateral muscles.
The femur is dissected clear of surrounding tissues. The periosteum is raised to the appropriate level (Fig. 39-5, B). The femur is transected with a power saw. The bone should be transected generously proximal to the skin incision, allowing for skin retraction during healing and avoiding tension on the distal incision by the remaining femur. The posterior flap is then fashioned with an amputation knife or cautery. The sciatic nerve is ligated as far proximal as possible, then allowed to retract with transection.
Strict hemostasis is achieved with cautery and silk ligatures in the AKA patient. The fascia is approximated with absorbable sutures; the skin is closed with staples or nonabsorbable suture (Fig. 39-5, C and D). A padded sterile dressing is applied with a final application of an impervious dressing.
Eidt, JF, Kalapatapu, VR. Lower extremity amputation: techniques and results. In Cronenwett J, Johnston KW, eds.: Rutherford’s vascular surgery, 7th ed, Philadelphia: Saunders, 2010.
Goodney, PP, Holman, K, Henke, PK, et al. Regional intensity of vascular care and lower extremity amputation rates. J Vasc Surg. 2013.
Robinson, KP. Amputations in vascular patients. In: Bell PRF, ed. Surgical management of vascular disease. Philadelphia: Saunders, 1992.