CHAPTER 90 Ablative Surgery for Spasticity
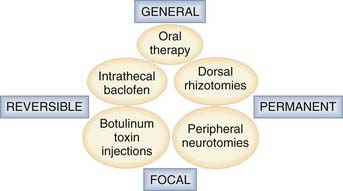
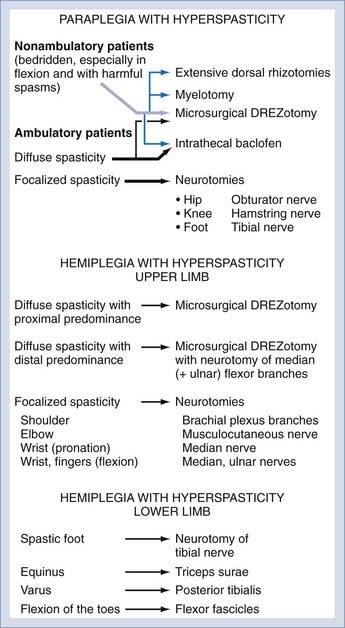
Management of spasticity includes not only intrathecal baclofen therapy and botulinum toxin injections but also destructive surgery directed at peripheral nerves, dorsal roots, the dorsal root entry zone (DREZ), and the spinal cord. Methods of surgical management are classified according to whether their impact is general or focal and whether the effects are temporary or permanent (Fig. 90-1).
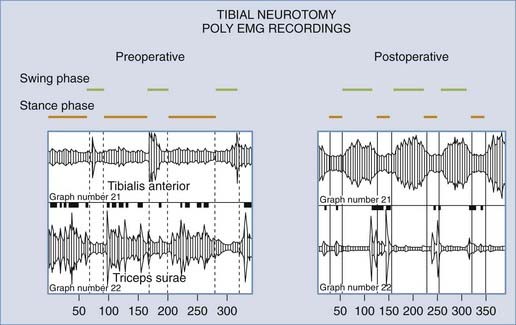
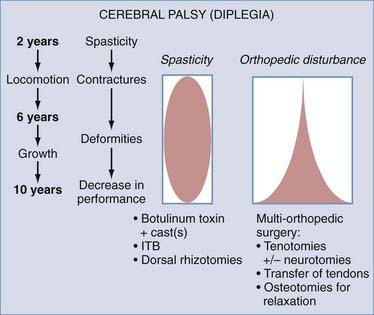
Neurodestructive procedures must be performed so that excessive tone is reduced without suppressing useful muscular tone or impairing any residual motor/sensory functions. In patients who retain some masked voluntary motility, the aim is to re-equilibrate the balance between paretic agonist and spastic antagonist muscles so that treatment results in improvement in (or the reappearance of) voluntary motor function (Fig. 90-2). In patients with poor residual function preoperatively, the aim is to halt the evolution of orthopedic deformities and improve comfort.
Our team has treated more than 1000 patients with spasticity over the past 20 years. We believe that teams dealing with spasticity should have all of the technical modalities at hand.1 Intrathecal baclofen therapy, which is discussed in detail in another chapter of this book, is indicated primarily for paraplegic or tetraplegic adult patients with diffuse spasticity, especially of spinal origin, although it can also be used to treat spasticity related to cerebral palsy in older children. Ablative operations are indicated for focal spasticity of the limbs when treatment with botulinum toxin injections proves insufficient. Peripheral neurotomy is justified when harmful spasticity affects one or a few muscular groups. A preliminary test consisting of an anesthetic block may help in the decision-making process by mimicking the effect of the neurotomy. When harmful spasticity affects an entire limb or in the setting of hemiplegia or paraplegia, surgery directed at the dorsal roots (dorsal rhizotomy) or the DREZ (microsurgical DREZotomy) may be the solution. Complementary orthopedic operations are frequently needed in patients with associated irreducible contractures, tendon retractions, joint deformities, or any combination of these problems.
Selective Peripheral Neurotomy
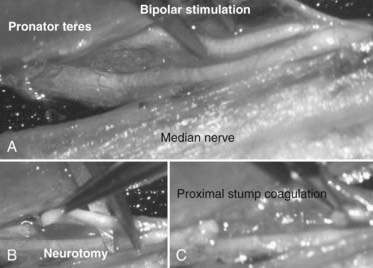
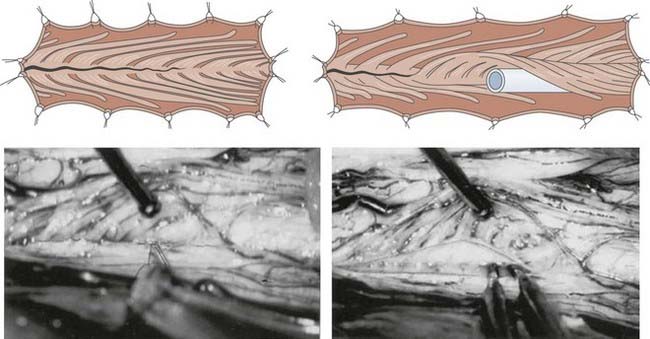
Peripheral neurotomy was introduced for the treatment of a spastic foot by Stoffel.2 Later, peripheral neurotomy was made more selective by using microsurgery and mapping via intraoperative electrical stimulation to better identify the function of individual nerve fascicles (Fig. 90-3).3,4 Neurotomy consists of partial sectioning of one or several of the motor branches (or fascicles) corresponding to the muscle or muscles in which spasticity is considered excessive and works by interrupting the segmental reflex arc in both its afferent and efferent limbs. Neurotomy must not include sensory nerve fibers because even partial sectioning of them can result in deafferentation pain. Either motor branches must be clearly isolated from the nerve trunk, or the fascicles must be dissected and identified within the nerve trunk several centimeters proximal to the formation of an identifiable branch. On an empirical basis it is agreed that neurotomy must include sectioning of approximately 50% to 80% of all the branches to a targeted muscle for it to be effective.
Surgical Techniques
Surgery on the Lower Limb*
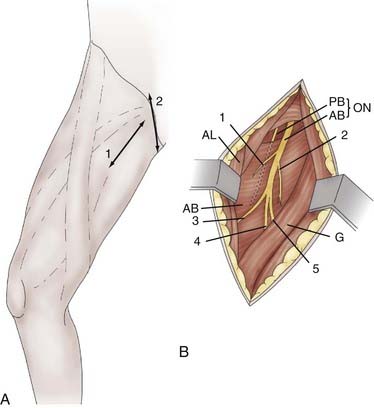
Obturator Neurotomy for the Hip
Obturator neurotomy eliminates spasticity of the adductor muscles. It is often proposed for diplegic children with cerebral palsy when crossing or “scissoring” of the lower limbs hampers their walking. It can also be performed on paraplegic children to facilitate perineal washing, toilet, and self-catheterization. The incision can be made along the body of the adductor longus at the proximal portion of the thigh or transverse in the hip flexion fold, centered on the prominence of the adductor longus tendon. In addition to its more aesthetic appearance, the latter incision facilitates adductor longus tenotomy when necessary (Fig. 90-4A). The dissection is conducted lateral to the adductor longus muscle body to rapidly locate the anterior branch of the obturator nerve. The posterior branch is situated more deeply and should be spared to preserve the hip-stabilizing muscles (Fig. 90-4B).
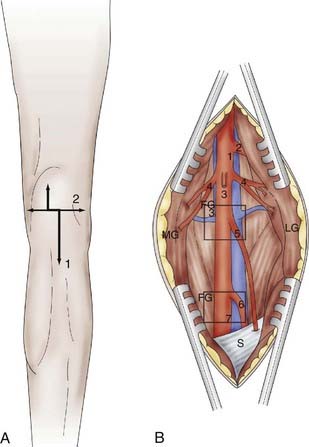
Hamstring Neurotomy for the Knee
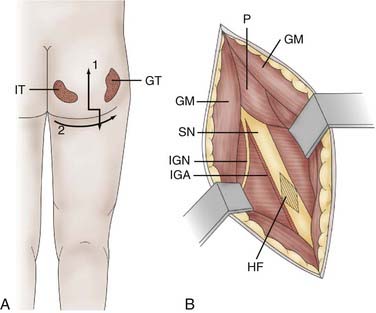
Hamstring neurotomy is indicated for children with spastic diplegia to counter the accentuation of flexion deformity of the knees observed with growth. A transverse incision is made in the gluteal fold, centered on the groove between the ischium and greater trochanter (Fig. 90-5A). After crossing the fibers of the gluteus maximus, the sciatic nerve is identified in the depth of the incision. Branches to the hamstring muscles are isolated at the border of the nerve, primarily based on motor evoked responses of the semitendinosus muscle, which is often the major muscle responsible for spasticity (Fig. 90-5B).
Tibial Neurotomy for the Foot
Tibial neurotomy is indicated for the treatment of varus spastic footdrop with or without claw toes. It consists of exposing all motor branches of the tibial nerve at the popliteal fossa (i.e., nerves to the gastrocnemius and soleus, tibialis posterior, popliteus, flexor hallucis longus, and flexor digitorum longus). In a majority of patients, the soleus is almost completely responsible for the pathogenesis of spastic footdrop, so the gastrocnemius may be spared.8 The incision can be made vertical on either side of the popliteal fold and extended inferiorly or transversely in the popliteal fossa to yield a more aesthetic result. In addition, the latter incision allows high tenotomy of the gastrocnemius fascial insertion to be performed at the end of the procedure if necessary (Fig. 90-6A).
The first nerve encountered is the sensory medial cutaneous nerve of the leg, which is located immediately anterior to the saphenous vein. It must be spared. More deeply, the tibial nerve trunk, from which the nerves to the gastrocnemius emerge, is easily identifiable. The superior soleus nerve is situated in the midline, just posterior to the tibial nerve. An effective soleus neurotomy is marked by the immediate intraoperative disappearance of ankle clonus. By retracting the tibial nerve trunk medially with a traction adhesive tape, the other branches can then be identified by electrical stimulation as they emerge from the lateral edge of the tibial nerve trunk. The most lateral branch is the popliteal nerve, followed by the tibialis posterior nerve and finally by the inferior soleus nerve and flexor digitorum longus nerves. Some fascicles, often larger, can give a toe flexion response via the intrinsic toe flexors (Fig. 90-6B). However, neurotomy of these branches is not recommended if they cannot be clearly individualized because they may be mixed with sensory fascicles.
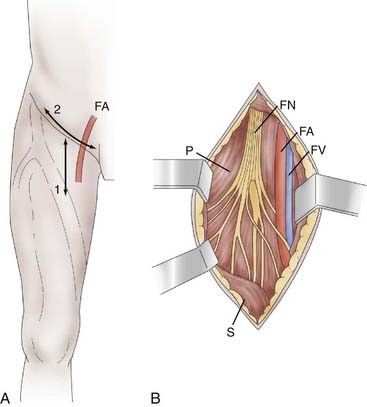
Femoral Neurotomy for the Quadriceps
Femoral neurotomy is indicated to treat excessive spasticity of the quadriceps muscle. This muscle is often spastic, which can interfere with gait by limiting knee flexion during the swing phase. Given its “strategic” importance in maintaining upright posture, a motor block is an essential part of the preoperative evaluation. The neurotomy involves the motor branch to the rectus femoris and vastus intermedius muscles. A horizontal incision is made in the hip flexion fold (Fig. 90-7A). The dissection passes medial to the sartorius muscle body and exposes the motor branches of the femoral nerve, first the nerve to the rectus femoris and then, more deeply, the nerve to the vastus intermedius (Fig. 90-7B). Electrical stimulation is essential given the large number of sensory fascicles of this nerve that must be spared.
Surgery on the Upper Limb
Pectoralis Major and Teres Major Neurotomy for the Shoulder
Neurotomy of collateral branches of the brachial plexus innervating the pectoralis major or the teres major is indicated for spasticity of the shoulder with internal rotation and adduction.9 For the pectoralis major, the skin incision is made at the innermost part of the deltopectoral sulcus and curves along the clavicular axis. The clavipectoralis fascia is then opened and the upper border of the pectoralis major muscle reflected downward. Close to the thoracoacromialis artery, the ansa of the pectoralis muscle is identified with the aid of a nerve stimulator. For the teres major, the skin incision follows the inner border of the teres major from the lower border of the posterior head of the deltoid muscle to the lower portion of the scapula. The lower border of the long portion of the brachii triceps constitutes the upper limit of the approach. The dissection is carried deep between the teres minor and major muscles. In the vicinity of the subscapular artery, the nerve ending on the teres major is identified. The nerve is surrounded by thick fat when approaching the anterior facet of the muscle body.
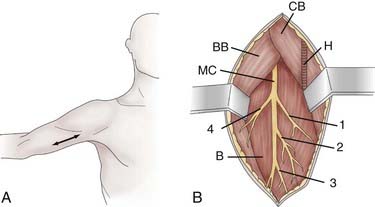
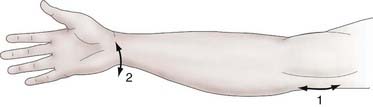
Musculocutaneous Neurotomy for the Elbow
Neurotomy of the musculocutaneous nerve is indicated for spasticity of the elbow with flexion mediated by the biceps brachii and brachialis muscles. The skin incision is performed longitudinally, from the inferior edge of the pectoralis major medial to the biceps brachii, and is extended 5 cm (Fig. 90-8A). The superficial fascia is opened between the biceps laterally and the coracobrachialis medially. The brachial artery and median nerve exit medially. The dissection proceeds in the space where the musculocutaneous nerve lies anterior to the brachialis muscle (Fig. 90-8B). Opening the epineurium allows the fascicles of the nerve to be dissected; the motor fascicles are distinguished from the sensory ones with a nerve stimulator.
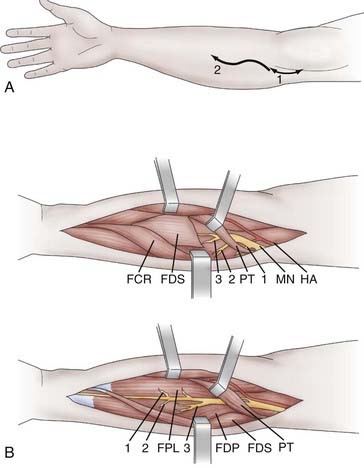
Median Neurotomy for the Wrist and Fingers
Neurotomy of the median nerve is indicated for spasticity of the forearm with pronation mediated by the pronator teres and quadratus muscle, for spasticity of the wrist with flexion mediated by the flexor carpi radialis and palmaris longus muscles, and for spasticity of the fingers with flexion attributable to the flexor digitorum superficialis (flexion of the proximal interphalangeal and metacarpophalangeal joints) and the flexor digitorum profundus muscle (flexion of the distal interphalangeal joints). Swan neck deformation of the fingers mediated by the lumbrical and interosseous muscles can be limited by neurotomy of the median and ulnar nerves. With regard to the thumb, neurotomy of the median nerve is indicated for spasticity with flexion and adduction/flexion (thumb-in-palm deformity) attributable to the flexor pollicis longus. The skin incision begins 2 to 3 cm above the flexion line of the elbow, medial to the biceps brachii tendon, passes through the elbow, and curves toward the junction of the upper and middle thirds of the anterior aspect of the forearm (the convexity of the curve turns laterally) (Fig. 90-9A).10,11 Thereafter, the median nerve is searched for medial to the brachial artery and identified at the elbow, deeply under the lacertus fibrosus, which is cut. Sharp dissection is used to separate the branches of the median nerve. The pronator teres belly with its two heads is retracted medially and distally so that its muscular branches can be inspected. This muscle is next retracted up and laterally while the flexor carpi radialis is pulled down and medially. The muscular branches to the flexor carpi radialis and flexor digitorum superficialis can then be seen. Finally, the latter is retracted medially to uncover the branches to the flexor digitorum profundus, flexor pollicis longus, and pronator quadratus. These latter muscular branches may be individualized as separate branches or may remain together in the distal trunk of the anterior interosseous nerve. Sometimes it may be useful to divide the fibrous arch of the flexor digitorum superficialis muscle to make the dissection easier (Fig. 90-9B).
Ulnar Neurotomy for the Wrist and Fingers
Neurotomy of the ulnar nerve is also indicated for spasticity of the wrist with flexion and ulnar deviation, both mediated by the flexor carpi ulnaris; for spasticity of the fingers with flexion mediated by the flexor digitorum profundus muscle, which is partly innervated by the ulnar nerve; and for spasticity of the thumb with adduction/flexion attributable to the adductor pollicis. Ulnar neurotomy can also be performed in conjunction with median neurotomy for swan neck deformation of the fingers. A separate arched skin incision is made to expose the ulnar nerve at the medial part of the elbow (Fig. 90-10), where it enters between the two heads of the flexor carpi ulnaris. There, the motor branches to this latter muscle are identified. Distally, the branches to the medial half of the flexor digitorum profundus are identified.
Surgery on the Spinal Roots, Dorsal Root Entry Zone, and Spinal Cord
History
In accordance with Sherrington’s experimental data, Foerster in 1908 performed the first dorsal rhizotomies from L1-S2 (excluding L4, the root of the quadriceps) for lower limb spasticity in cerebral palsy patients. From his experience with 159 patients, Foerster suggested the following12:
In 1945, Munro suggested sectioning the ventral roots from the last thoracic to the first sacral segments to treat irreducible spasticity with severe spasms.13 This type of procedure was recommended for spasticity associated with spontaneous hyperactivity of motor neurons, as observed after anoxia. In fact, sectioning the dorsal roots is ineffective in such cases, whereas ventral root sectioning abolishes the spasms.
In 1951, Bischof described longitudinal myelotomy,14 the aim of which is to interrupt the spinal reflex arc between the ventral and dorsal horns with a vertical coronal incision performed laterally from one side of the spinal cord to the other, from the L1-S1 segments, in paraplegic patients. The technique was then modified to avoid complete interruption of the corticospinal fibers. Via a T9-L1 laminectomy, a posterior longitudinal sagittal incision is made before performing a cruciform myelotomy by making a transverse incision on either side with a stylet that has a right-angle extremity. The purpose of this surgically performed lesion is to interrupt the spinal reflex arc between the ventral and dorsal horns without sectioning the fibers connecting the pyramidal tract to the motor neurons of the ventral horn. Longitudinal myelotomy was used widely for patients with triple flexion and severe sphincter disturbances.
To reduce the harmful effects of dorsal rhizotomy on postural tone in ambulatory patients with cerebral palsy, Gros and pupils introduced topographic selection of rootlets by electrical stimulation to preserve the innervation of muscles responsible for useful tone (the quadriceps and abdominal and gluteal muscles in particular).3,15 This technique was termed selective posterior rhizotomy. Apart from effects on the lower limbs, Gros also observed a decrease in spasticity of the upper limbs and improvement in speech and swallowing in his cerebral palsy patients. This is termed an indirect effect.
In 1977, Fraioli and Guidetti proposed partial dorsal rhizotomy, which consisted of incising the dorsalmost part of each rootlet a few millimeters before its entry into the dorsolateral sulcus in an attempt to spare sensation.16 In 1976, Fasano and collaborators developed functional dorsal rhizotomy, a technique based on stimulation of the posterior rootlets with corresponding EMG recordings.17 Exaggeration of the duration or extent of the motor evoked response indicated the particular roots that must be surgically sectioned. In 1972, Sindou and associates observed that the technique of selective microsurgical destruction of the ventrolateral part of the DREZ, which was developed for treating pain,18,19 led to marked hypotonia in the muscles corresponding to the operated medullary segments.20 Subsequently, the technique was applied to severe spasticity in either the upper limb of hemiplegic patients or the lower limb of paraplegic patients.
Because microsurgical DREZotomy performed for pain achieved a potent hypotonic effect, the procedure was applied not only to hyperspastic states in paraplegic patients21 but also to severe cases of hemiplegic upper limbs.22 This potent effect is presumably due not only to interruption of the (tonigenic) dorsal afferent fibers but also to lesioning of the dorsal horn gray matter, which contains a quantity of interneurons that convey “tonigenic” input to motor neurons of the ventral horn.
Surgical Techniques
Dorsal Rhizotomy
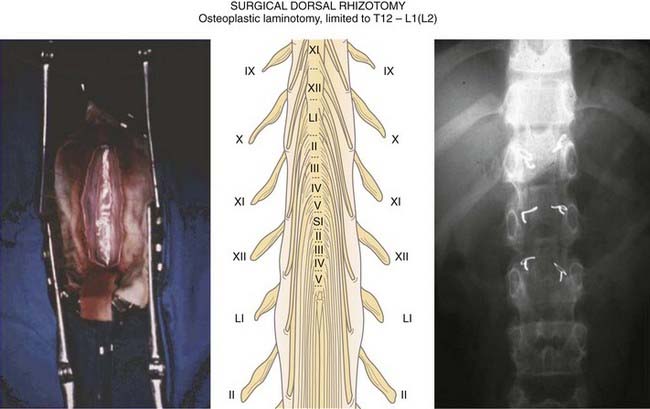
The surgical approach for dorsal rhizotomy varies significantly from one team to another. The most classic technique—described first by Fasano and coworkers17 and then by Peacock and Arens23 and Abbott and colleagues24—is as follows: a one-piece laminotomy is performed from L1-S1 with a high-speed saw, which allows repositioning at the end of the procedure. Bipolar electrical stimulation of the sensory roots is carried out with the assistance of multichannel EMG recordings (in addition to palpation of the leg muscles for evidence of contraction). Roots that when stimulated cause either muscle activity outside their myotome or activity that persists after cessation of the stimulus are deemed abnormal and are separated into their rootlets. The rootlets are in turn stimulated and the same criteria used to judge their normality. Abnormally responsive rootlets are candidates to be cut.
To limit the extent of this approach, we prefer a limited osteoplastic laminotomy from T11-L1, which will be replaced and fixed at the end of the procedure (Fig. 90-11).1 The ventral (and corresponding dorsal) L1, L2, and L3 roots are identified by their muscular responses to electrical stimulation, which is performed intradurally just before they enter their dural sheaths. The dorsal lumbosacral rootlets are recognized at their entrance into the dorsolateral sulcus at the conus medullaris. The landmark between the S1 and S2 medullary segments is located approximately 30 mm from the exit of the tiny coccygeal root from the conus. The dorsal rootlets of S1, L5, and L4 can be identified by the motor responses evoked by stimulation, the sensory roots for the bladder (S2-3) by monitoring vesical pressure, and those for the anal sphincter (S3-4) by rectomanometry (or simply by using a finger introduced into the anal canal or by EMG recordings). Surface spinal cord somatosensory evoked potentials recorded from the tibial (L5-S1) and pudendal nerves (S1-3) may also be helpful. For surgery to be effective, approximately 60% of the dorsal rootlets must be cut, the amount depending on the level and function of the roots involved. In most cases, L4, which predominantly provides innervation to the quadriceps femoris, must be preserved.
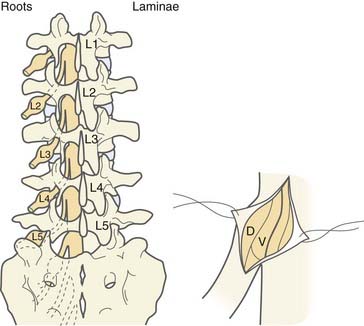
In 2001, to further reduce the invasiveness of the approach, we designed a “staged interlaminar approach” in which the level or levels to be operated on are selected on the basis of the preoperative chart (Fig. 90-12). At surgery, the lumbosacral spine is approached posteriorly in the midline so that the preselected interlaminar spaces can be reached. After resecting the ligamentum flavum, the chosen interlaminar space or spaces are enlarged by resecting the lower half of the superior and the upper half of the inferior laminae. The dura is opened in the midline for a distance of 2 cm. The L2 and L3 roots can be reached through an L1-2 opening, L4 and L5 through L3-4, and S1 and S2 via an L5-S1 opening. Generally, the dorsal rootlets (five on average) are easily identified with the microscope because they are grouped posterior to the ventral root and separated from it by a fibrous septum. Evoked motor responses are tested via the ventral and then dorsal root (rootlets). The threshold for obtaining motor responses by stimulation of the dorsal root (rootlets) is approximately three times greater than the threshold when corresponding ventral root (rootlets) are used (1 to 2 mA at 2 Hz for the latter). After identification of the dorsal rootlets, the appropriate number of them are divided, between a third and two thirds of the overall dorsal rootlets, according to the preoperative chart. The dural incision is sutured in watertight fashion and the dural suture line is covered with fat harvested from the subcutaneous layer.
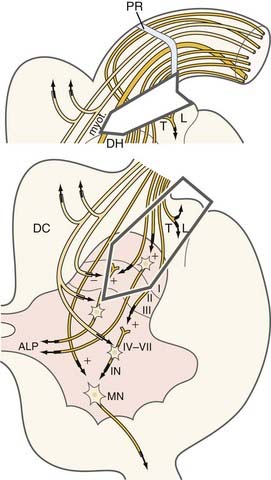
Lesioning at the Dorsal Root Entry Zone
The aim of microsurgical DREZotomy is to preferentially interrupt both the small-caliber (nociceptive) and large-caliber (myotatic) tonigenic fibers of the dorsal roots, respectively situated laterally and in the middle of the entry zone. The surgical lesion must partially if not totally preserve the medially positioned large-caliber fibers that project to the dorsal horn of the cord. The surgical target includes most of the dorsal horn, where the fibers and neurons that activate the segmental circuitry of the spinal cord are situated (Fig. 90-13). The technique is detailed in Figures 90-14 and 90-15. Briefly, the procedure consists of 3-mm-deep microsurgical incisions—at the level of the dorsolateral sulcus—with a 35-degree angle at the cervical level and a 45-degree angle at the lumbosacral level. Bipolar coagulation is performed ventrolaterally at the entrance of the rootlets into the dorsolateral sulcus and inside the gray matter of the dorsal horn along all the spinal cord segments selected for surgery.
Patient Selection
Because the features and consequences of spasticity differ from one patient to another, it is important that the objective or objectives of treatment be defined for every patient: improvement in function, prevention of deformities, or alleviation of discomfort and pain. These issues must be explained to the patient, relatives, and caregivers within the frame of a multidisciplinary team. Guidelines for surgical intervention in spasticity have been detailed elsewhere.25–27
Treating Spasticity in Adults
Spasticity should not be treated just because it is present; it should be treated because it is harmful to the patient. Patients may be able to use spastic limbs for functional activities. An extensor pattern in the lower limb or limbs may aid in standing transfers. In this scenario, “successful” spasticity management, if measured by reduction in tone and improved range of motion, might reduce rather than enhance function. Hence, the goal of spasticity management must be improved function and prevention or reversal of fixed deformities. Differentiating dynamic from fixed deformities is of prime importance before deciding on any surgical treatment, whether neurosurgical or orthopedic, or both. Dynamic range-of-motion measures are a useful starting point, supplemented with instrumented measures of spasticity and its effects on function, such as motion analysis. Guidelines for treating spasticity are shown in Fig. 90-16.
Treating Spasticity in Children
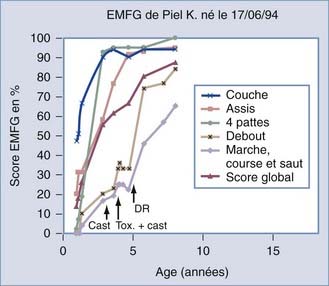
The first step in the evaluation process is to observe the child clinically to understand the child’s function and disability. The second step is to measure range of motion to detect contractures that will not respond to neurosurgical treatment. The third step is to quantify the spasticity by using the Tardieu or the Ashworth scales. The final step is to grade the child on the Gross Motor Function Measure and to observe the evolution of gross motor function with time (Fig. 90-17).
Several effective neurosurgical treatments for spasticity can be used in children with cerebral palsy (Fig. 90-18). For diffuse spasticity of the lower limbs, dorsal rhizotomy or intrathecal baclofen administration may be considered; dorsal rhizotomy is proposed when definitive action targeted to certain muscle groups is preferred. For focal spasticity, botulinum toxin injection permits delaying surgery until the child is old enough to undergo selective neurotomy.
Spasticity in the Lower Limb
Spasticity should be assessed every 6 or 12 months with the Gross Motor Function Measure so that future motor function can be predicted. Surgery may be delayed if the curve demonstrates increasing function or may be indicated if the curve plateaus or decreases (see Fig. 90-17)
Conclusion
Because of its complexity, neurosurgical management of spasticity requires a multidisciplinary approach.25–27 Because the characteristics and functional consequences of spasticity differ from patient to patient, the general rule is to tailor individual treatments. The goals are to decrease “harmful spasticity,” respect “useful spasticity,” preserve residual motor/sensory functions, reveal masked capabilities, and improve functional ability.
Abbott A, Forem SL, Johann M. Selective posterior rhizotomy for the treatment of spasticity. Childs Nerv Syst. 1989;5:337-346.
Bischof W. Die longitudinal Myelotomie. Zentrabl Neurochir. 1951;11:79-88.
Brunelli G, Brunelli F. Selective microsurgical denervation in spastic paralysis. Ann Chir Main. 1983;2:277-280.
Decq P, Cuny E, Filipetti P, et al. Role of soleus muscle in spastic equinus foot. Lancet. 1998;11(352):118.
Decq P, Filipetti P, Feve A, et al. Peripheral selective neurotomies of the brachial plexus branches for the spastic shoulder. Anatomical study and clinical results in 5 patients. J Neurosurg. 1997;86:648-653.
Decq P, Mertens P. Société de Neurochirurgie de la Langue Française. La Neurochirurgie de la Spasticité. Neurochirurgie. 2003;49:135-416.
Fasano VA, Barolat-Romana G, Ivaldi A, et al. La radicotomie postérieure fonctionnelle dans le traitement de la spasticité cérébrale. Neurochirurgie. 1976;22:23-34.
Foerster O. On the indications and results of the excision of posterior spinal nerve roots in men. Surg Gynecol Obstet. 1913;16:463-474.
Fraioli B, Guidetti B. Posterior partial rootlet section in the treatment of spasticity. J Neurosurg. 1977;46:618-626.
Gros C. Spasticity—Clinical classification and surgical treatment. In: Krayenbühl H, editor. Advances and Technical Standards in Neurosurgery, Vol 6. Wien, New York: Springer; 1979:55-97.
Maarrawi J, Mertens P, Luaute J, et al. Long-term functional results of selective peripheral neurotomy for the treatment of spastic upper limb: prospective study in 31 patients. J Neurosurg. 2006;104:215-225.
Mertens P, Sindou M. Surgical management of spasticity. In: Barnes MP, Johnson GR, editors. Clinical Management of Spasticity. Cambridge: Cambridge University Press; 2001:239-265.
Mertens P, Sindou M. Selective peripheral neurotomies for the treatment of spasticity. In: Sindou M, Abbott R, Keravel Y, editors. Neurosurgery for Spasticity. A Multidisciplinary Approach. Wien, New York: Springer-Verlag; 1991:119-132.
Munro D. The rehabilitation of patients totally paralysed below waist: anterior rhizotomy for spastic paraplegia. N Engl J Med. 1945;233:456-461.
Peacock WJ, Arens LJ. Selective posterior rhizotomy for the relief of spasticity in cerebral palsy. S Afr Med J. 1982;62:119-124.
Privat JM, Benezech J, Frerebeau P, et al. Sectorial posterior rhizotomy, a new technique of surgical treatment for spasticity. Acta Neurochir (Wien). 1976;35:181-195.
Sindou M. Neurosurgical management of disabling spasticity. In: Spetzler RF, editor. Operative Techniques in Neurosurgery, Vol 7. Philadelphia: Saunders; 2004:95-174.
Sindou M, Abbott A, Keravel Y, editors. Neurosurgery for Spasticity: A Multidisciplinary Approach. Vienna, New York: Springer Verlag, 1991.
Sindou M, Fischer G, Goutelle A, et al. La radicellotomie postérieure sélective. Premiers résultats dans la chirurgie de la douleur. Neurochirurgie. 1974;20:391-408.
Sindou M, Fischer C, Goutelle A, et al. La radicellotomie postérieure sélective dans le traitement des spasticités. Rev Neurol. 1974;30:201-215.
Sindou M, Jeanmonod D. Microsurgical DREZotomy for the treatment of spasticity and pain in the lower limbs. Neurosurgery. 1989;24:655-670.
Sindou M, Mertens P. Decision-making for neurological treatment of disabling spasticity in adults. Oper Tech Neurosurg, 7. 2004:113-118.
Sindou M, Mertens P. Selective neurotomy of the tibial nerve for the treatment of the spastic foot. Neurosurgery. 1988;23:738-744.
Sindou M, Mifsud JJ, Boisson D, et al. Selective posterior rhizotomy in the dorsal root entry zone for treatment of hyperspasticity and pain in the hemiplegic upper limb. Neurosurgery. 1986;18:587-595.
Sindou M, Quoex C, Baleydier C. Fiber organization at the posterior spinal cord-rootlet junction in man. J Comp Neurol. 1974;153:14-26.
Sindou M, Simon F, Mertens P, et al. Selective peripheral neurotomy (SPN) for spasticity in childhood. Childs Nerv Syst. 2007;23:957-970.
Stoffel A. The treatment of spastic contractures. Am J Orthop Surg. 1912;10:611-644.
1 Sindou M. Neurosurgical management of disabling spasticity. In: Spetzler RF, editor. Operative Techniques in Neurosurgery, Vol 7. Philadelphia: Saunders; 2004:95-174.
2 Stoffel A. The treatment of spastic contractures. Am J Orthop Surg. 1912;10:611-644.
3 Gros C. Spasticity—Clinical classification and surgical treatment. In: Krayenbühl H, editor. Advances and Technical Standards in Neurosurgery, Vol 6. Wien, New York: Springer; 1979:55-97.
4 Sindou M, Abbott A, Keravel Y, editors. Neurosurgery for Spasticity: A Multidisciplinary Approach. Vienna, New York: Springer Verlag, 1991.
5 Sindou M, Mertens P. Selective neurotomy of the tibial nerve for the treatment of the spastic foot. Neurosurgery. 1988;23:738-744.
6 Mertens P, Sindou M. Selective peripheral neurotomies for the treatment of spasticity. In: Sindou M, Abbott R, Keravel Y, editors. Neurosurgery for Spasticity. A Multidisciplinary Approach. Wien, New York: Springer-Verlag; 1991:119-132.
7 Sindou M, Simon F, Mertens P, et al. Selective peripheral neurotomy (SPN) for spasticity in childhood. Childs Nerv Syst. 2007;23:957-970.
8 Decq P, Cuny E, Filipetti P, et al. Role of soleus muscle in spastic equinus foot. Lancet. 1998;11(352):118.
9 Decq P, Filipetti P, Feve A, et al. Peripheral selective neurotomies of the brachial plexus branches for the spastic shoulder. Anatomical study and clinical results in 5 patients. J Neurosurg. 1997;86:648-653.
10 Brunelli G, Brunelli F. Selective microsurgical denervation in spastic paralysis. Ann Chir Main. 1983;2:277-280.
11 Maarrawi J, Mertens P, Luaute J, et al. Long-term functional results of selective peripheral neurotomy for the treatment of spastic upper limb: prospective study in 31 patients. J Neurosurg. 2006;104:215-225.
12 Foerster O. On the indications and results of the excision of posterior spinal nerve roots in men. Surg Gynecol Obstet. 1913;16:463-474.
13 Munro D. The rehabilitation of patients totally paralysed below waist: anterior rhizotomy for spastic paraplegia. N Engl J Med. 1945;233:456-461.
14 Bischof W. Die longitudinal Myelotomie. Zentrabl Neurochir. 1951;11:79-88.
15 Privat JM, Benezech J, Frerebeau P, et al. Sectorial posterior rhizotomy, a new technique of surgical treatment for spasticity. Acta Neurochir (Wien). 1976;35:181-195.
16 Fraioli B, Guidetti B. Posterior partial rootlet section in the treatment of spasticity. J Neurosurg. 1977;46:618-626.
17 Fasano VA, Barolat-Romana G, Ivaldi A, et al. La radicotomie postérieure fonctionnelle dans le traitement de la spasticité cérébrale. Neurochirurgie. 1976;22:23-34.
18 Sindou M, Quoex C, Baleydier C. Fiber organization at the posterior spinal cord–rootlet junction in man. J Comp Neurol. 1974;153:14-26.
19 Sindou M, Fischer G, Goutelle A, et al. La radicellotomie postérieure sélective. Premiers résultats dans la chirurgie de la douleur. Neurochirurgie. 1974;20:391-408.
20 Sindou M, Fischer C, Goutelle A, Schott B, Mansuy L. La radicellotomie postérieure sélective dans le traitement des spasticités. Rev Neurol. 1974;30:201-215.
21 Sindou M, Jeanmonod D. Microsurgical DREZotomy for the treatment of spasticity on pain in the lower limbs. Neurosurgery. 1989;24:655-670.
22 Sindou M, Mifsud JJ, Boisson D, Goutelle A. Selective posterior rhizotomy in the dorsal root entry zone for treatment of hyperspasticity and pain in the hemiplegic upper limb. Neurosurgery. 1986;18:587-595.
23 Peacock WJ, Arens LJ. Selective posterior rhizotomy for the relief of spasticity in cerebral palsy. S Afr Med J. 1982;62:119-124.
24 Abbott A, Forem SL, Johann M. Selective posterior rhizotomy for the treatment of spasticity. Childs Nerv Syst. 1989;5:337-346.
25 Sindou M, Mertens P. Decision-making for neurological treatment of disabling spasticity in adults. Oper Tech Neurosurg. 2004;7:113-118.
26 Mertens P, Sindou M. Surgical management of spasticity. In: Barnes MP, Johnson GR, editors. Clinical Management of Spasticity. Cambridge: Cambridge University Press; 2001:239-265.
27 Decq P, Mertens P. Société de Neurochirurgie de la Langue Française. La Neurochirurgie de la Spasticité. Neurochirurgie. 2003;49:135-416.