Anterior abdominal wall105
11.2 Inguinal canal, scrotum, testis, inguinal hernias109
11.3 Arrangement of the gut tube in the abdominal cavity113
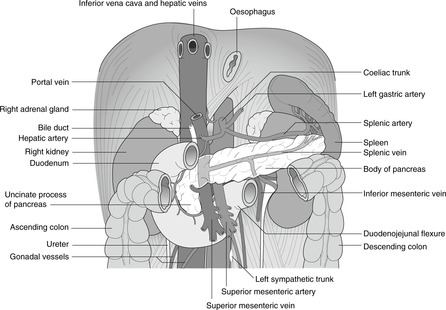
11.4 Great vessels of the abdomen, sympathetic chain116
11.5 Foregut and associated structures: pancreas, spleen, liver, gall bladder118
11.6 Midgut and hindgut126
11.7 Portal venous system: venous drainage of the gut tube and associated organs129
11.8 Nerve supply of the gut tube, gut pain131
11.9 Posterior abdominal wall, diaphragm and associated structures132
11.10 Kidneys, ureters, adrenals134
11.11 Pelvis136
11.12 Perineum145
11.13 Autonomic nervous system in the abdomen and pelvis: a review151
11.14 Summary of surface markings and vertebral levels152
Introduction
The abdominal or peritoneal cavity is separated from the thorax by the diaphragm, and from the perineum below by the pelvic diaphragm or levator ani muscle. It is supported by the vertebral column, rib cage, and the bony pelvis formed by the two hip bones and the sacrum. Upper abdominal organs (e.g. liver, stomach, spleen, kidneys) are to some extent protected by the rib cage, while others low down (e.g. bladder, uterus, prostate) are protected by the bony pelvis. It follows from this that organs most closely related to bone may be damaged by injuries to these bones: for example fractures of the left tenth rib may damage the spleen.
Abdominal walls
The abdominal walls between rib cage and bony pelvis are formed by muscles and fascia. Details of the posterior abdominal wall are of no great clinical importance, and they are considered only briefly in section 11.9. The anterior abdominal wall, on the other hand, being so often inspected, palpated and incised, needs a section of its own.
11.1. Anterior abdominal wall
The anterior abdominal wall is divided into nine regions or four quadrants. The regions are in the midline from top to bottom, epigastrium, umbilical and hypogastrium, and the lateral regions are, from top to bottom, hypochondrial, lumbar and iliac fossa or inguinal. The quadrants are right upper, right lower, left upper and left lower. Muscles of the abdominal wall are external oblique, internal oblique, transversus abdominis and rectus abdominis. The blood supply and innervation of the anterior abdominal wall are relevant to trauma, disease and surgery.
You should:
• list the nine regions and four quadrants and the principal organs and structures that lie deep to them and which can be palpated in those regions
• describe the muscular components of the anterior abdominal wall
• describe the blood supply and innervation of the anterior abdominal wall.
Surface anatomy and regions
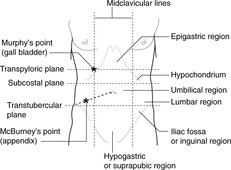
The nine descriptive regions of the anterior abdominal wall (Fig. 11.1) are demarcated by two vertical and two horizontal planes. The vertical planes are the right and left midclavicular lines, and the horizontal planes the transpyloric (by most people, although some prefer the subcostal) and transtubercular planes.
• Transpyloric plane: vertebral level L1. This intersects the rib cage at the tip of the ninth costal cartilage. It is about halfway between the suprasternal notch and the pubic symphysis, or about halfway between the xiphoid process and the umbilicus, and it marks the position or level of several internal structures (e.g. pylorus, gall bladder, renal hila, origin of superior mesenteric artery).
• Subcostal plane: vertebral level L2/3. This is the plane marking the lowest point of the rib cage. In an ill, bedridden patient it can be difficult to find, particularly if the patient is obese.
• Transtubercular plane: vertebral level L3. The tubercles of the iliac crests are palpable some distance behind the anterior superior iliac spines (ASIS). In practice, the ASIS is easier to feel than the tubercles and the plane of the ASIS may be substituted for the transtubercular plane. In any case, these lines are only rough guides.
Superficial and deep fascia
Between the skin and the muscles of the abdominal wall is the superficial (Camper’s) fascia: thin in a lean person, and thick in a fat person. The deep (Scarpas’s) fascia is a tough membrane on the external aspect of the muscles.
Clinical examination
In the midline, from top to bottom
• Epigastrium. Stomach tumours may be palpable here, and pain from foregut structures (as far as the duodenal papilla) is usually referred to this area. The pulsating aorta is palpable slightly to the left of the midline.
• Umbilical region. Pain from midgut structures (duodenal papilla to splenic flexure of the colon) is usually referred to this area. The pulsating aorta is palpable above the umbilicus.
• Hypogastrium or suprapubic region. Enlarged pelvic organs may be palpable here (uterus, bladder) and pain from hindgut structures (descending colon to anal canal) is usually referred to this area.
Right and left, from top to bottom
• Hypochondriac region. On the right, the liver and the gall bladder may be palpable. The tip of the right ninth costal cartilage, the usual surface marking of the fundus of the gall bladder, is Murphy’s point. On the left an enlarged spleen (at least three times normal size) may be palpable.
• Lumbar region. The lower poles of the kidneys may be palpated here, and the descending colon may be palpable on the left.
• Iliac fossa or inguinal region. The usual surface marking of the base of the appendix is McBurney’s point: one-third of the way along a line from the right anterior superior iliac spine to the umbilicus. Tenderness in the right iliac fossa may signify disease of the appendix, and a hard mass here may be cancer of the caecum or ascending colon. The descending colon may be palpable on the left, and a mass in the left iliac fossa may signify a tumour of the sigmoid colon or bulky faeces.
Quadrants
Quadrants are also commonly used for description:
• right upper quadrant (gall bladder, liver)
• left upper quadrant (enlarged spleen)
• right lower quadrant (appendix, caecum)
• left lower quadrant (sigmoid colon).
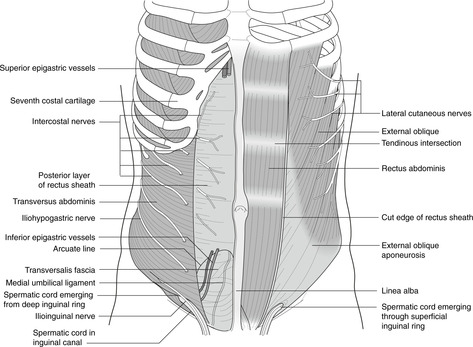
Muscles of anterior abdominal wall (Fig. 11.2)
• Rectus abdominis muscle which lies on either side of the midline.
• The sheet muscles: three anterolateral muscle sheets: external oblique, internal oblique and transversus abdominis muscles.
Rectus abdominis muscle
This runs from rib cage and sternum to the pubic bones. On contraction, it compresses the abdominal contents and is a flexor of the spinal column. Transverse tendinous intersections are (in a lean person) visible and palpable above the umbilicus. They are of little significance except that when cut they bleed profusely.
• Linea semilunaris. This is the lateral margin of the rectus abdominis. It meets the rib cage at or near the ninth costal cartilage (vertebral level L1, transpyloric plane). It can be made more obvious (to either hand or eye) by asking the supine patient to raise the head, causing rectus abdominis to contract.
• Linea alba. This is in the midline between the rectus muscles and is usually palpable as a slight depression. Weaknesses in the linea alba may result in midline herniation of abdominal contents, often at the umbilicus.
Sheet muscles: external and internal obliques, transversus abdominis
The sheet muscles are attached to lumbar fascia posteriorly (don’t bother with details), to the ribs and costal cartilages superiorly, to the hip bones inferiorly and the inguinal ligament (from ASIS to pubic tubercles) inferiorly. Medially, muscle fibres give way to broad, flat tendons (aponeuroses) which form the rectus sheath around the rectus abdominis muscle. Fibres of these muscles run in different directions, reinforcing each other, and inferiorly they form the inguinal canal through which the spermatic cord in the male, and the round ligament of the uterus in the female, pass from abdomen to scrotum or labia majora respectively. The inguinal canal is an important area (see section 11.2, below).
• External oblique muscle. From the lower eight ribs, fibres pass downwards and medially to the linea alba, pubic region and inguinal ligament, and inferiorly to the anterior superior iliac spine and iliac crest. The aponeurosis of external oblique contributes to the anterior wall of the rectus sheath. Along a line from the anterior superior iliac spine to the pubic tubercle, the aponeurosis is thickened to form the inguinal ligament, where the deep fascia of the thigh is attached to the external oblique aponeurosis.
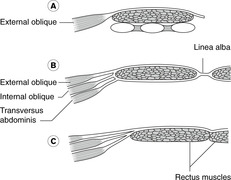
• Internal oblique muscle. From the lateral part of the inguinal ligament, the iliac crest and the lumbar fascia, these fibres pass upwards and medially to the costal margin and the linea alba. The aponeurosis of internal oblique splits to contribute to both anterior and posterior walls of the rectus sheath (Fig. 11.3). The lowest fibres, arising from the inguinal ligament, arch down to attach medially with similar fibres of transversus abdominis to the pubic tubercle as the conjoint tendon (see section 11.2).
• Transversus abdominis muscle. From the six lowest ribs, lumbar fascia, iliac crest and the lateral part of the inguinal ligament, fibres run across to the linea alba contributing to the rectus sheath (Fig. 11.3). As with internal oblique, the lowest fibres arch down to attach to the pubic tubercle as the conjoint tendon.
• Transversalis fascia. This layer of connective tissue separates the muscles of the anterior abdominal wall from the parietal peritoneum.
Rectus sheath
The usual pattern is shown in Fig. 11.3, although there is considerable variation. Inferiorly, since the aponeuroses of all three sheet muscles pass anterior to rectus abdominis, the only tissue separating rectus abdominis from the parietal peritoneum is transversalis fascia. Above this on the posterior aspect of rectus abdominis is the arcuate line – the free lower extremity of that part of the rectus sheath that passes posterior to rectus abdominis.
Action of the muscles as a whole
The sheet muscles and rectus abdominis are active in trunk movements: flexion, lateral flexion and twisting. They compress the abdominal contents during defecation and provide support and stability during lifting. Asymmetrical spasm of these muscles during youth and adolescence has been implicated in cases of scoliosis (twisted spine).
Nerve supply of anterior abdominal wall (Fig. 11.2)
This is from segmental nerves T7–L1. Intercostal nerves leave the costal grooves where the ribs turn superiorly, and continue into the abdominal wall. T12 segmental nerve is the subcostal nerve. L1 segmental nerve divides into two: the more cranial is the iliohypogastric, which principally supplies the abdominal wall, the more caudal the ilioinguinal, which is diverted to the anterior scrotum or labia majora, and the medial thigh.
Segmental nerves T7–12 travel in the abdominal wall between transversus abdominis and internal oblique, sending branches through these muscles to more superficial structures (e.g. skin) and internally to the peritoneum. The iliohypogastric and ilioinguinal nerves (L1) posteriorly are found between transversus and internal oblique, but in the region of the anterior superior iliac spine they penetrate internal oblique and run between internal and external obliques. This apparently trivial detail is relevant to inguinal anatomy and to incisions near McBurney’s point, for example for appendicectomy (see later).
• Sensory fibres in the nerves supply abdominal skin, wall and peritoneum (as well as thoracic skin and pleura). Cell bodies of sensory fibres are in the dorsal root ganglion of the appropriate nerve. See dermatome map (Fig. 6.6, p. 36). Note that the dermatome over the xiphoid process is (usually) T8, over the umbilicus T10, and over the pubic symphysis T12/L1.
• Motor fibres in the nerves supply the sheet muscles and the rectus abdominis. The cell bodies of the motor neurons are in the ventral horn of grey matter of the appropriate segment of the spinal cord.
Blood supply and lymph drainage of anterior abdominal wall
Arteries
• Intercostal arteries, part of the intercostal neurovascular bundles, approach from the lateral aspect.
• Epigastric arteries. Posterior to rectus abdominis muscle are:
– superior epigastric artery: a continuation of the internal thoracic artery from the subclavian
– inferior epigastric artery: a branch of the external iliac/femoral.
These freely anastomose and this may become a bypass channel for an aortic blockage (e.g. coarctation, see Fig. 10.25, p. 88).
• Branches of segmental lumbar arteries supply the posterior abdominal wall.
Veins
Intercostal veins drain to the azygos system. Lumbar (segmental) veins drain to the veins of the posterior abdominal wall and the azygos system (details not necessary), and the superior and inferior epigastric veins drain to subclavian and femoral veins respectively. Anastomoses between these venous channels may provide a bypass for a blockage of the inferior vena cava.
Lymph
The lymph drainage of the anterior abdominal wall is roughly in quadrants: superiorly to right and left axillary nodes, and inferiorly to right and left inguinal nodes.
Abdominal incisions
• Median incisions. The linea alba is a nerveless and comparatively bloodless plane.
• Paramedian incisions. Nerves enter rectus abdominis muscles from the lateral aspect, so in paramedian incisions, the anterior layer of the rectus sheath is incised and the rectus abdominis muscle displaced laterally so as not to tear the nerves. It is better to avoid incisions through the tendinous intersections, if possible: they bleed profusely.
• Incisions through the sheet muscles, e.g. a gridiron incision near McBurney’s point for appendicectomy. Muscle fibres need only be separated to give sufficient access, but it is worth noting that the L1 nerves (ilioinguinal and iliohypogastric) are in the vicinity of an incision over McBurney’s point, and that damage to the iliohypogastric nerve might weaken the muscles of the anterior abdominal wall in the inguinal region, increasing the possibility of a subsequent inguinal hernia.
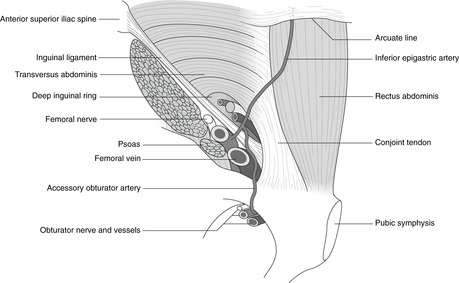
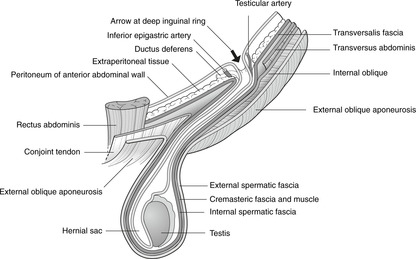
11.2. Inguinal canal, scrotum, testis, inguinal hernias (Figs 11.4, 11.5)
The inguinal canal is a weak spot in the anterior abdominal wall. In the male it transmits structures to and from the testis; in the female it is much smaller. The internal aspect of the canal is the deep inguinal ring; the external aspect is the superficial ring. In embryonic life the testis migrates from the abdomen to the scrotum. It is covered in the scrotum by three layers of fascia, and most intimately, by the tunica vaginalis, the cavity of which is a part of the peritoneal cavity that becomes detached during development. The abdominal origin of the testis is reflected in its vascular supply, and also its lymph drainage to para-aortic nodes, unlike that of scrotal skin to inguinal nodes.
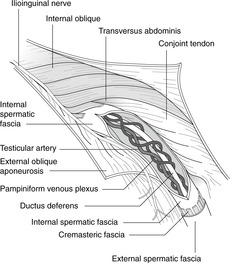
The inguinal canal
Imagine the developing testis inside the abdomen trying to make its way out. It must first penetrate the transversalis fascia: the defect in this layer so caused is the:
Deep (internal) inguinal ring
This is roughly circular and its surface marking is about 2cm above the femoral pulse at the inguinal ligament, the pulse being roughly halfway between the anterior superior iliac spine and the pubic tubercle. The deep ring is immediately lateral to the inferior epigastric artery passing up on the posterior surface of the rectus abdominis muscle.
Emerging from the deep inguinal ring, the testis makes its way downwards and medially, roughly parallel to and slightly above the inguinal ligament, through (in order) transversus abdominis and internal oblique to arrive at a defect in external oblique, the:
Superficial (external) inguinal ring
This is a triangular defect in external oblique, the base of which is medial to the pubic tubercle, and the apex of which points up and laterally so that most of the superficial ring is more-or-less directly above the pubic tubercle.
Inguinal canal – the pathway between the two rings (Figs 11.4, 11.5)
• The floor of the canal is formed by the inguinal ligament.
• The anterior wall is formed by external oblique aponeurosis throughout, reinforced laterally (over the deep ring) by internal oblique.
• The posterior wall is formed by transversalis fascia throughout, reinforced medially (deep to the superficial ring) by the conjoint tendon (united internal oblique and transversus abdominis) attached to the pubic tubercle.
• The roof of the canal is made up of the fibres of internal oblique arching over the contents of the inguinal canal to form the conjoint tendon.
In coughing, straining and lifting, the muscles of the anterior abdominal wall contract and the diaphragm is fixed so that abdominal contents (e.g. bowel) might be forced through the potential weak spot of the inguinal region. This is minimised by the way in which the muscles move when contracting which results in the arching fibres of internal oblique being pulled inferiorly to cover the anterior aspect of the deep inguinal ring, thereby reinforcing it and reducing the size of the potential weakness.
Spermatic cord
As the testis ‘pushes’ its way through the inguinal canal towards the scrotum, it drags with it the ductus deferens, arteries, veins and nerves passing to the testis. These structures constitute the spermatic cord, which acquires coverings that to some extent reflect the layers of the abdominal wall through which they have passed. From inside out these are:
• the internal spermatic fascia
• the cremasteric fascia and cremaster muscle
• the external spermatic fascia.
The spermatic cord also includes:
• the testicular artery, on each side a direct branch of the aorta
• the pampiniform plexus of veins which form the testicular vein draining on the right to the inferior vena cava and on the left to the renal vein
• testicular lymphatics passing to para-aortic nodes (the lymph drainage of the testis thus reflecting its arterial supply)
• the genital branch of the genitofemoral nerve (L1, 2) which supplies cremaster muscle with involuntary motor fibres – cremaster muscle retracts the testis
• sympathetic nerve fibres
• blood vessels serving the ductus deferens.
Ilioinguinal nerve L1
This supplies anterior scrotal and penile skin. It enters the inguinal canal not through the deep inguinal ring, but from the lateral aspect. In the region of the anterior superior iliac spine it lies between internal and external obliques, and so, as it runs down parallel to the inguinal ligament it is joined in the inguinal canal by the structures which have entered through the deep inguinal ring. The ilioinguinal nerve passes through the superficial inguinal ring on the surface of the spermatic cord.
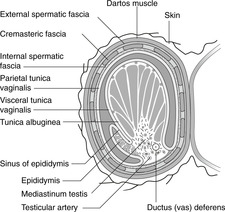
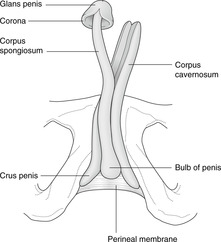
Scrotum (Fig. 11.6)
The scrotum is equivalent to the labia majora in the female. It is a body wall structure, so:
• its arterial supply is from body wall arteries (pudendal, femoral)
• its venous drainage is to body wall veins (pudendal, great saphenous)
• its lymph drainage is mainly to inguinal lymph nodes (very important)
• its cutaneous sensory nerve supply is from ilioinguinal (L1), genital branch of genitofemoral (L1, 2) and scrotal branches of the pudendal (S2, 3, 4) nerves.
Scrotal skin is thin and contains smooth muscle fibres – dartos, supplied by sympathetic fibres, which contract in the cold to cause wrinkling.
Testis (Fig. 11.6)
In the scrotum, each testis is invaginated into its serous membrane, the tunica vaginalis, much as the lung is invaginated into the pleura. The serous cavity around the testis was in fetal life continuous with the peritoneal cavity through the processus vaginalis (the tunica vaginalis and peritoneum being exactly equivalent), but as the muscles of the anterior abdominal wall are formed and become stronger, the processus becomes separated from the main peritoneal cavity. Attached to the lateral surface of the testis is the epididymis, into which the seminiferous tubules of the testis converge and eventually unite to form at its lower, and narrower end, the ductus (vas) deferens. The recess between the epididymis and the testis is the sinus of the epididymis. The covering of the testis, between it and the visceral layer of tunica vaginalis, is the tunica albuginea.
Unlike the scrotum, the testis is an organ of the posterior abdominal wall, like the kidney, and therefore:
• testicular arteries come directly from the aorta
• testicular veins drain to the IVC on the right and the renal vein on the left
• and, most importantly, lymphatic drainage is to nodes around the abdominal aorta, para-aortic nodes, and not to inguinal nodes like scrotal skin.
Testicular descent
The testis develops high on the posterior wall of the embryonic coelom and subsequently descends through the inguinal canal so that at or soon after birth it should be in the scrotum. Its descent may be arrested at any stage. It may take a wrong turn after it has come through the inguinal canal: such ectopic testes are fairly easy to place in the scrotum since the spermatic cord is long enough. More difficult to deal with is the testis, which has not travelled far enough to have a sufficiently long spermatic cord for the testis to be placed in the scrotum. Testes which are allowed to remain ectopic are inclined to malignant change.
Retractile testes
The testis may be retracted into the abdomen, out of harm’s way (presumably) – this is cremaster in action. The cremaster reflex may be elicited by gentle stimulation of the skin of the scrotum or anterior thigh, and plunging into cold water may cause retraction, although it is not usual for a man to retract his testes at will. It is of clinical significance in the young boy: a testis which has retracted in shock (as it were) because the hand palpating the scrotum is cold may be mistaken for an undescended testis.
Testicular malignancy and lymph drainage
If you suspect a testicular malignancy and find the inguinal nodes are enlarged, it is reasonable to assume that the malignancy has already spread from the testis to invade neighbouring scrotal skin, whence it has spread further to the inguinal nodes. Testicular malignancy is potentially lethal and it is as well for men to examine their testes as women do their breasts.
Testicular torsion
The testis may twist upon the spermatic cord resulting in occlusion of the blood supply. This is painful and is an emergency: the cord needs to be untwisted before the testis dies.
Vasectomy
This is ligation and removal of a short length of the ductus (vas) deferens, usually for the purposes of birth control.
Swellings arising in the testis
• Hydrocele. There may be a build-up of serous straw-coloured fluid between the layers of the tunica vaginalis (compare with pleural effusion). This is usually innocent: it simply needs to be drained by needle aspiration.
• Varicocele. Varicose veins of the pampiniform plexus and testicular veins may arise, more commonly (inexplicably, despite several theories) on the left than the right.
• Spermatocele. This is a fluid-filled cyst of the epididymis containing spermatozoa. It is uncommon.
Inguinal hernias (Fig. 11.7)
A hernia is a condition in which internal structures are forced out through a weakness in the wall. In the inguinal region, abdominal contents (e.g. intestines, fat) may pass through the inguinal canal – a potential weak spot in the anterior abdominal wall. Since the canal is larger in the male than the female, inguinal hernias are commoner in the male.
Types of inguinal hernia
• Indirect inguinal hernia. Abdominal contents pass through the deep inguinal ring and into the canal. They may be so large that they continue through the superficial ring, above and medial to the pubic tubercle, and present as a scrotal swelling. The neck (internal opening) of the hernia in this case would be through the deep inguinal ring, lateral to the inferior epigastric artery.
• Direct inguinal hernia. Abdominal contents bulge through the anterior abdominal wall between the deep inguinal ring and the midline, usually owing to a weak conjoint tendon. In this case, the neck of the hernia would be medial to the inferior epigastric artery.
It is not usually possible to distinguish these two hernias on clinical examination alone, except that a large scrotal hernia is more likely to be an indirect hernia.
• Congenital inguinal hernia. The potential space between the two layers of the tunica vaginalis may remain in continuity after birth with the peritoneal cavity. This is a congenital inguinal hernia: coils of intestine may surround the testis in the scrotum.
Is it an inguinal hernia or a scrotal swelling?
It may be difficult to distinguish between a scrotal swelling of testicular origin and a large inguinal hernia extending into the scrotum. If it is possible to ‘get above’ the swelling, it is not an inguinal hernia but something confined to the scrotum, for example a hydrocele.
Inguinal region in the female
Everything in the inguinal region of the female is much the same as in the male, except that it is all smaller and, as noted, inguinal hernias are less common in the female (but see Ch. 13; Femoral hernia, p. 210). The structure in the female which passes through the inguinal canal is the round ligament of the uterus, an insignificant structure derived from the gubernaculum (see an Embryology text for details). The labia majora of the female share the same blood supply (femoral, pudendal), nerve supply (genitofemoral, pudendal) and lymph drainage (mainly to inguinal nodes) as the scrotum in the male.
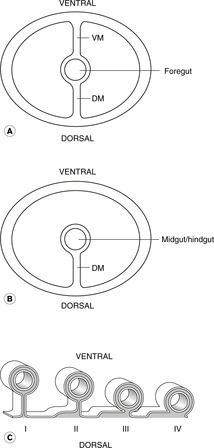
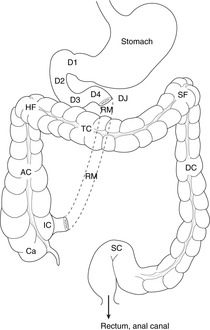
11.3. Arrangement of the gut tube in the abdominal cavity
The intestines and associated organs were originally connected to the posterior abdominal wall by an elongated hilum, the dorsal mesentery. Subsequent changes in the disposition of abdominal viscera result in a complex arrangement of mesenteries and omenta. The transverse colon divides the abdominal cavity into supracolic and infracolic compartments. The areas on either side of the ascending and descending colons are the paracolic gutters. Other important areas of the peritoneal cavity are the lesser sac, the hepatorenal pouch and the subphrenic spaces.
Some embryological considerations
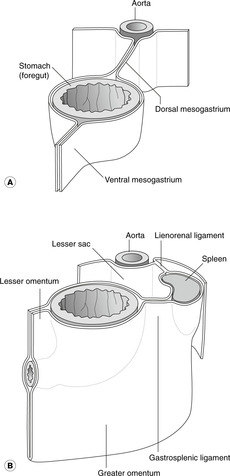
Think of the gut tube and associated organs as pushing their way into the peritoneal cavity from behind, much as the lung pushes its way into the pleural cavity. The ‘hilum’ of the gut tube, where the parietal and visceral peritoneal layers meet, is elongated into a structure which connects the entire length of the gut tube to the dorsal body wall, and through it pass blood vessels, nerves, and lymphatics. This is the dorsal mesentery (Fig. 11.8).
In the embryo, the gut tube enters the abdomen from the thorax passing behind a mass of mesoderm called the septum transversum, which subsequently becomes part of the diaphragm, liver and the connections between them and the ventral body wall. The upper part of the abdominal gut tube is attached not only to the dorsal body wall by the dorsal mesentery, but also to the ventral body wall by these derivatives of the septum transversum, which form the ventral mesentery (Fig. 11.8). This part of the gut tube is foregut and it extends distally as far as what will be the mid-portion of the duodenum. The remainder of the gut tube, midgut and hindgut, is connected to the dorsal body wall only by the dorsal mesentery, known simply as the mesentery: there is no ventral mesentery here.
This simple layout of the gut tube in the peritoneal cavity is subsequently complicated by two factors. First, the tube elongates spectacularly and coils on itself within the abdomen; and secondly some parts of the gut tube then adhere to the dorsal body wall, thus losing their mesentery and becoming apparently retroperitoneal, an adjective meaning that the dorsal mesentery has been lost (Fig. 11.8). Clinically, this means that those parts of the alimentary canal that remain mesenteric are more mobile and may twist or herniate into other areas, while those that are retroperitoneal are more or less fixed. The final layout is shown in Figure 11.9.
In the peritoneal cavity…
Strictly speaking there is nothing in the peritoneal cavity except a thin layer of peritoneal fluid. Yet, you will hear: ‘the stomach is in the peritoneal cavity’ as you hear ‘the lungs are in the pleural cavities’ and ‘the heart is in the pericardial cavity’. The function of the peritoneal cavity is, like the pleural and pericardial cavities, to permit movement of the gut tube (postural, peristalsis, etc.) independent of movement of the body wall.
Names – caution!
Abdominal cavity = peritoneal cavity. That part of the peritoneal or abdominal cavity that is within the pelvis is sometimes called the pelvic cavity, although it should more properly be the pelvic part of the peritoneal cavity.
Mesenteric = omental = epiploic = ligamentous (not to be confused with other uses of ligament). Which of these terms is used in any given situation is merely traditional.
Parts of the peritoneal cavity
• Supracolic compartment: superior to the transverse colon. This is usually taken to include the oesophagus, stomach, most of the duodenum, liver and biliary system.
• Infracolic compartment: inferior to the transverse colon. This includes the jejunum, ileum, caecum, ascending, descending and sigmoid colon, and rectum.
• Paracolic gutters: lateral to ascending and descending colons.
• Paravertebral gutters: between ascending and descending colons and the vertebral column.
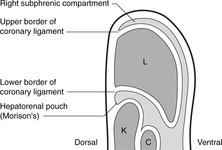
• Hepatorenal (Morison’s) pouch: the superior end of the right paracolic gutter between liver and kidney.
• Subphrenic (subdiaphragmatic) and subhepatic spaces (Fig. 11.10). The liver and diaphragm developmentally are different parts of the same thing (septum transversum) and they remain attached to each other at the so-called bare area of the liver. The recesses of the peritoneal cavity partially separate the two structures. Naming of these is not consistent, but the system given here is as good as any:
– Posterior subphrenic space: posterior to the liver, between it and the posterior diaphragm. It is continuous with Morison’s pouch.
– Anterior subphrenic space: anteriorly between the liver and the diaphragm.
The anatomy of the liver, mainly a right-sided organ, means that these spaces are on the right side of the body.
• Lesser sac. Developmental changes mean that that part of the peritoneal cavity to the right of the (originally midline) stomach becomes at first behind the stomach (as the ventral surface of the stomach is displaced to the right), and then almost completely isolated from the rest of the peritoneal cavity as a result of the duodenum becoming adherent to the dorsal body wall. This is the lesser sac of the peritoneal cavity, behind the stomach, and the small communication between it and the rest of the peritoneal cavity is the epiploic foramen of Winslow (see later). The rest of the peritoneal cavity, with its supracolic and infracolic compartments, is the greater sac.
Pouches and disease
These pouches and sacs may be the sites of collection of inflammatory fluid which, particularly around the diaphragm, may go undiagnosed unless they are deliberately excluded – that is to say unless you think about the possibility of their involvement, you will miss them. This is particularly true of the areas between liver and diaphragm, and Morison’s pouch which, in a patient lying supine in bed, is the most dependent part of the peritoneal cavity. Fluid may collect here unless appropriate physiotherapy and regular postural changes are instituted.
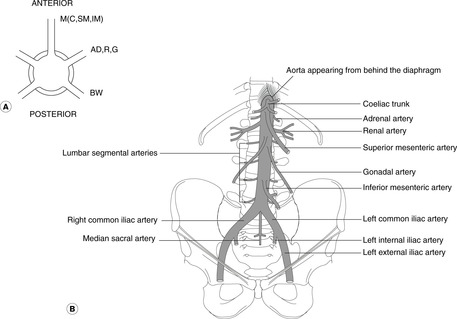
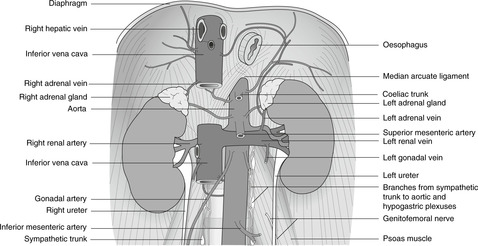
11.4. Great vessels of the abdomen, sympathetic chain
The aorta and inferior vena cava are on the posterior abdominal wall. Aortic branches serve the body wall (lumbar arteries), kidneys (renal arteries), gonads (ovarian and testicular arteries), and the gut tube (coeliac, superior mesenteric, inferior mesenteric arteries). The aorta divides into the common iliac arteries that supply pelvic organs and the lower limbs. The inferior vena cava is formed by the union of the common iliac veins and passes up on the right of the aorta to the liver where it is joined by hepatic veins, before penetrating the diaphragm and opening into the right atrium of the heart.
Aorta
The aorta enters the upper abdomen slightly to the left of the midline behind the diaphragm at vertebral level T12. It passes down to about vertebral level L3/4 where it divides (surface marking: just below and to the left of the umbilicus in a recumbent patient) into the common iliac arteries. It is easily palpated in the upper abdomen between the umbilicus and the rib cage.
Branches of the aorta (Fig. 11.11)
• Lumbar segmental arteries. There are paired, body wall branches, equivalent to the intercostals in the thorax. They are of no significance except that they give branches that pass into the vertebral canal to supply the spinal cord. Damage to the larger ones, for example in abdominal aortic surgery, may lead to spinal cord lesions.
• Renals, adrenals, gonadals. These are paired arteries, anomalous arrangements of which are common. The renals arise at about vertebral level L1 and you should study radiographs of them. The origin of the gonadals is more variable, but is usually about vertebral level L2/3.
• Mesenteric. These single, unpaired branches arise ventrally. There are three:
– Coeliac. Vertebral level T12. Supplies abdominal foregut (up to duodenal papilla) and structures which develop in foregut mesenteries: stomach, liver, spleen, most of the pancreas, duodenum as far as the papilla, greater omentum, lesser omentum.
– Superior mesenteric. Vertebral level T12/L1 (that is, immediately below the coeliac). Supplies midgut: distal duodenum, uncinate process of pancreas, jejunum, ileum, caecum, appendix, ascending colon, transverse colon, associated mesenteric structures.
– Inferior mesenteric. Vertebral level L3 (but more variable). Supplies hindgut: descending colon, sigmoid colon, rectum and upper part of anal canal.
• The common iliac arteries pass down and laterally towards the lower limbs. At the pelvic brim they divide to give external and internal iliac arteries.
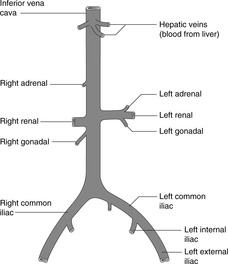
Inferior vena cava (Fig. 11.12)
The inferior vena cava is slightly to the right of the midline. It is formed from the two common iliac veins and passes upwards through the liver and diaphragm (at vertebral level T8) to enter the thorax. Its main tributaries are the renal, gonadal, adrenal and hepatic veins. Venous anatomy is in general much more variable than arterial anatomy, and anomalies are frequently encountered. A study of its complex embryology, though certainly not essential, will help to explain why. Suffice it here to say that the inferior vena cava may begin on the left and cross over the aorta to the right, or there may even be bilateral cavas up as far as the renal veins.
 |
| Fig. 11.12 |
Segmental veins drain eventually to the azygos system and the superior vena cava; they have nothing to do with the inferior vena cava.
Sympathetic chain
• The right sympathetic chain passes down from the thorax and comes to lie posterolateral to the inferior vena cava.
• The left sympathetic chain comes to be posterolateral to the aorta. Below the aortic bifurcation the chains continue over the pelvic brim in front of the sacrum and they unite to form the ganglion impar (unpaired). See section 11.13 (p. 151).
11.5. Foregut and associated structures: pancreas, spleen, liver, gall bladder
Oesophagus
The oesophagus enters the abdomen behind the diaphragm at vertebral level T10 slightly to the left of the midline surrounded by fibres from the right diaphragmatic crus forming a sphincter mechanism: the cardio-oesophageal sphincter. See section 11.9 (p. 132).
Hiatus hernia
This arises when part of the stomach pushes its way up into the thorax through the oesophageal opening in the diaphragm. The two types, rolling and sliding, are dealt with in clinical texts. Hiatus hernias may give rise to epigastric discomfort. This is not the same as a congenital diaphragmatic hernia, in which there is a defect in one or both sides of the diaphragm.
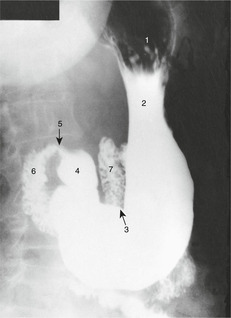
Stomach (Figs 11.13, 11.14)
The size and position of the stomach vary depending upon body shape, degree of distension, and posture. The five areas of the stomach (do not worry about the precise boundaries) are:
• cardia (around the oesophageal opening)
• fundus (above the level of the oesophageal opening)
• body (central portion)
• antrum (lower part)
• pylorus (the most distal part), the thickened sphincter mechanism controlling passage of stomach contents to the duodenum. The pylorus normally lies at about vertebral level L1, the transpyloric plane.
 |
| Fig. 11.13 |
The left border is the greater curvature and the right the lesser curvature.
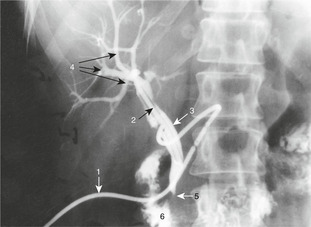
Radiology of the stomach (Fig. 11.14)
The alimentary canal can be demonstrated radiographically with the use of radio-opaque barium compounds. A barium swallow demonstrates the mouth, pharynx and oesophagus. In a barium meal the stomach and small intestines are displayed after an appropriate time interval.
Lesser omentum and lesser sac (Fig. 11.15)
As explained earlier, the original ventral border of the stomach is attached to the ventral body wall by the ventral mesogastrium. This border becomes the lesser curvature, and the ventral mesogastrium (mesogastrium = mesentery of the stomach) becomes, from stomach ventrally, lesser omentum, liver and falciform (sickle-shaped) ligament. The lesser omentum moves during development so that by the time of birth it lies in a more-or-less coronal plane, and behind it and the stomach is the lesser sac of the peritoneal cavity, which opens into Morison’s pouch of the greater sac through the epiploic foramen of Winslow.
Greater omentum, gastrosplenic ligament and splenorenal (lienorenal) ligament (Fig. 11.15)
Between spleen and stomach the mesentery is known by two names. Above, it is the gastrosplenic ligament. Below, it grows down to form a double layer of omental (mesenteric) tissue partly covering the intestines – the greater omentum. This is, amongst other things, a fat store and may become very large – regrettably so in some middle-aged people (including the author). The greater omentum is, with the stomach and lesser omentum, part of the anterior wall of the lesser sac, and, again in development, it becomes adherent to the mesentery of the transverse colon – the transverse mesocolon – so that the transverse colon is attached to the under surface of the greater omentum.
Duodenum (Fig. 11.16)
This is like three and a half sides of an approximate rectangle, inside which is the head of the pancreas. There are four parts.
• First part. This passes backwards and horizontally, becoming retroperitoneal (i.e. loses its mesentery). It passes anterior to the common bile duct and the gastroduodenal artery. Posterior duodenal ulcers may erode this, causing haemorrhage.
• Third part. This is retroperitoneal and passes horizontally to the left at about vertebral level L2/3, crossing the midline in front of the abdominal aorta below the origin of the superior mesenteric artery. Disease of either duodenum or aorta can result in an aortoduodenal fistula presenting as bleeding into the intestine.
• Fourth part. This, also retroperitoneal, turns upwards on the left side of the midline and at about vertebral level L1 turns to the left and once again becomes mesenteric as the jejunum: this is the duodenojejunal flexure (‘d–j flexure’) or junction. It is anchored (some say) by a few smooth muscle fibres in the so-called ligament of Treitz, which passes down from the diaphragm to the duodenojejunal junction.
 |
| Fig. 11.16 |
Pancreas (Fig. 11.16)
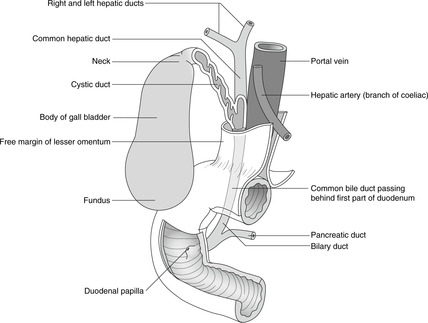
Duct system (Figs 11.16, 11.17)
The exocrine acini secrete into a duct system that begins in the tail and proceeds to the right. As it enters the head it turns inferiorly to join the common bile duct and enters the duodenum at the papilla. There may be an accessory pancreatic duct opening above the main duct.
 |
| Fig. 11.17 |
Blood supply
This is from branches of the coeliac and superior mesenteric arteries (see later).
Pancreatic disease
• Pancreatic pain is often felt in the back as well as generally in the abdomen anteriorly.
• Inflammation of the pancreas (pancreatitis) may result in a collection of inflammatory fluid in the lesser sac – a pancreatic pseudocyst.
• Cancer of the head of the pancreas may result in blockage of the common bile duct as it approaches the duodenal papilla.
• The pancreas develops from two outgrowths of foregut which, after some rotation around the gut tube, fuse. Congenital anomalies include a condition in which pancreatic tissue forms a ring around the duodenum – annular pancreas. This may cause duodenal obstruction.
Spleen (Fig. 11.16)
This is situated at the back (not the side) on the left, related to ribs 9, 10 and 11. It extends between vertebral levels T12–L2 under the left dome of the diaphragm. It is anterior to the left costodiaphragmatic recess of the pleural cavity. It does not normally extend any further anteriorly than the midaxillary line and is therefore not normally palpable. It is about the size of a clenched fist and, having developed in the dorsal mesogastrium, is attached to the dorsal body wall by the splenorenal ligament and to the stomach by the gastrosplenic ligament. At its hilum (vertebral level L1, transpyloric plane) it is in contact with the tail of the pancreas, which extends into the splenorenal ligament, through which the splenic vessels pass between the posterior abdominal wall and the spleen.
Splenic injury and disease
The spleen is in danger from trauma to the left lower rib cage, particularly ribs 9, 10 and 11. A ruptured spleen may cause fatal haemorrhage since, as part of the haematological policing system of the body, it has a profuse blood supply. It may become enlarged in haematological conditions or liver disease. As it enlarges it becomes palpable at the left subcostal margin, but you should note that by the time it does so it is already about three times larger than normal. It may enlarge further diagonally down towards the right iliac fossa. Such a huge spleen may be found in haematological diseases (e.g. sickle cell anaemia, leukaemia), and, lacking a palpable border in the place where it might be expected because it is so large, it may escape detection.
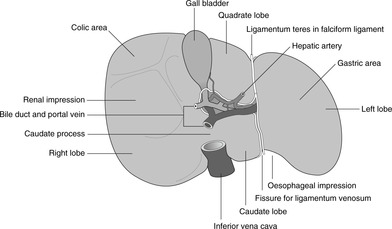
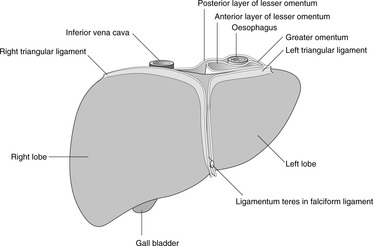
Liver and biliary system (Fig. 11.18, Fig. 11.19, Fig. 11.20 and Fig. 11.21)
Position and surface anatomy
The liver occupies the right and central upper abdomen, roughly from the fourth intercostal space (nipple in a lean male) to the costal margin. A very rough approximation is to draw a triangle whose angles are the two nipples and the tenth costochondral junction. Posteriorly, it is somewhat smaller: to map its surface projection, join the two inferior angles of the scapulas to the midpoint of the right eleventh rib.
 |
| Fig. 11.18 |
 |
| Fig. 11.21 |
Diaphragmatic and peritoneal attachments of the liver, bare area
The liver and most of the diaphragm develop from the septum transversum, and part of the liver remains in direct contact with the diaphragm with no intervening peritoneum: this is the bare area. The margins of the bare area, where the hepatic visceral peritoneum is reflected on to the under surface of the diaphragm, are known as the coronary ligament, and the right and left extremities of this are the right and left triangular ligaments.
Posteriorly, the liver is supported mainly by the inferior vena cava and the hepatic veins. Anteriorly (Fig. 11.18) it is connected to the anterior abdominal wall by the falciform ligament which has a free lower border extending from the internal aspect of the umbilicus to the inferior surface of the liver. This border contains the ligamentum teres – the obliterated umbilical vein that in fetal life conveyed oxygenated blood from the placenta to the fetus.
Parts of the liver
There are four anatomical lobes: right, left, quadrate and caudate. Their boundaries are not demarcated on the anterosuperior surface of the liver, but are clearer on the inferior, or visceral, surface (Fig. 11.19). This surface displays an H-shaped group of fissures. The crossbar of the H is the porta hepatis, the area anterior to it the quadrate lobe and posterior to it the caudate lobe.
• The left-sided limb of the H is a deep fissure receiving:
– the falciform ligament (with the ligamentum teres in its free edge), and
– part of the lesser omentum from the stomach, attached deep in this fissure to the obliterated ligamentum venosum (a continuation in the fetus of the umbilical vein).
• The right limb of the H is made up of two fossas, anteriorly for the gall bladder and posteriorly for the inferior vena cava.
• The quadrate lobe lies between the falciform ligament and the fossa for the gall bladder.
Physiologically and functionally, these anatomical lobes are of no significance. Functionally, the liver is divided into lobes and segments similar to the bronchopulmonary segments of the lung, each with its own branches of the hepatic artery and portal vein, and each with its own tributaries of the hepatic vein and the biliary tree. Knowledge of these is useful for surgeons but is not required for undergraduates.
Inferior vena cava and the liver
The inferior vena cava passes through the bare area of the liver and the diaphragm (vertebral level T8) to enter the thorax and the right atrium of the heart. In this region the right adrenal gland is posterior to the IVC and intimately related to the bare area of the liver.
Biliary tree and gall bladder (Fig. 11.17)
The biliary tree conveys the exocrine products of the liver (bile) to the duodenum. The gall bladder is a blind diverticulum of the biliary tree for the purposes of bile storage. The right and left hepatic ducts unite to form the common hepatic duct. The cystic duct from the gall bladder joins this to form the common bile duct. There is some variation in the layout of this duct system: the important thing is that the common bile duct passes down in the free edge of the lesser omentum, then posterior to the duodenum and into the substance of the head of the pancreas. It turns to the right and unites with the pancreatic duct. There is then a small widening, the ampulla of Vater, before the sphincter mechanism (sphincter of Oddi), which protrudes slightly into the left side of the second part of the duodenum as the duodenal papilla.
Biliary obstruction, obstructive jaundice (Fig. 11.20)
This arises when the normal passage of bile into the duodenum is blocked, either partially or wholly. It may arise within the liver (intrahepatic) or outside it (extrahepatic). Extrahepatic causes include gallstones, which find their way into the common bile duct and then block it, or cancer of the head of the pancreas, compressing the common bile duct from the outside as it passes through the head of the pancreas. In these cases with severe or complete blockage of the biliary tree, bile pigments will not reach the duodenum so the faeces will be lighter coloured than normal; biliary enzymes will not reach the intestines so that fat will be poorly digested and the faeces will be fatty (steatorrhoea) and float in the toilet bowl; bile pigments, instead of being in the intestines, will be absorbed into the bloodstream, so the patient appears yellow, and bile pigments are excreted in the urine, so the urine is dark. The combination of pale stools and dark urine means obstructive jaundice. Associated with episodes of excruciating pain, it probably means gallstones in the duct; associated with lassitude and weight loss it probably means cancer of the head of the pancreas.
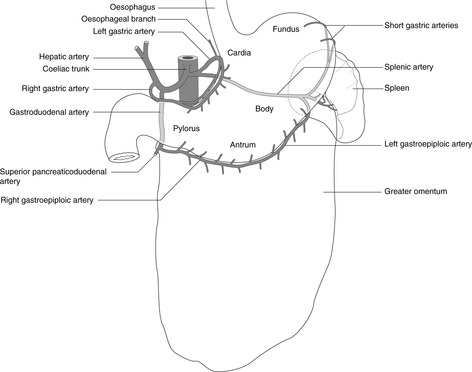
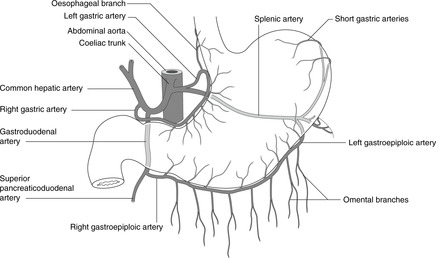
Blood supply of foregut derivatives: oesophagus, stomach, proximal duodenum, liver, gall bladder, pancreas, spleen – coeliac artery (Fig. 11.21)
The coeliac artery arises from the aorta at vertebral level T12, and supplies all the abdominal foregut and derivatives. There are three branches: splenic, hepatic, left gastric.
• Splenic: passes in the posterior wall of the lesser sac through or along the top of the pancreas (giving branches to it) and through the lienorenal ligament to the spleen. Near the spleen it gives short gastric arteries that pass in the gastrosplenic ligament to the fundus of the stomach, and the left gastroepiploic, which supplies the greater omentum and the greater curvature of the stomach.
• Common hepatic (usually simply hepatic): passes to the liver in the free edge of the lesser omentum. It gives:
– right gastric: lesser curvature
– gastroduodenal: passes inferiorly, behind the first part of the duodenum, and divides into the right gastroepiploic (for the greater curvature) and the superior pancreaticoduodenal which runs between the head of the pancreas and the duodenum, supplying them both
– cystic: to the gall bladder
– right and left hepatic arteries (terminal branches).
• Left gastric: lesser curvature and terminal oesophagus.
Note that the duodenum distal to the duodenal papilla is a midgut derivative. It is therefore supplied by branches of the superior mesenteric artery, in particular the inferior pancreaticoduodenal, which runs in the groove between pancreas and duodenum, anastomosing with the superior pancreaticoduodenal.
Boundaries of the epiploic foramen (of Winslow)
• Anterior – structures in the free edge of the lesser omentum: portal vein (behind), common hepatic artery (front left), common bile duct (front right).
• Superior – caudate lobe of liver.
• Posterior – inferior vena cava.
• Inferior – duodenum (first part).
Bleeding from the liver, Pringle’s manoeuvre
All blood passing to the liver enters through either the hepatic artery (freshly oxygenated, from the aorta) or the portal vein (from the intestinal bed). Both these vessels pass in the free edge of the lesser omentum. Bleeding from the liver, therefore, can be stemmed by compressing the free edge of the lesser omentum (Pringle’s manoeuvre). Should bleeding continue, it is likely that the inferior vena cava has been damaged.
Lymph drainage of foregut: stomach, liver, spleen, pancreas, duodenum, Virchow’s node
Lymph from foregut structures drains to coeliac nodes, although in reaching them other structures may be involved. The lymph drainage of the stomach is particularly important because of stomach cancer and, as elsewhere, it mirrors the arterial supply:
• lymph from the greater omentum passes to splenic and pancreatic nodes before reaching coeliac nodes
• as well as draining to the coeliac nodes, lymph from the lesser curvature may pass retrogradely to the liver, leading to hepatic involvement – this is not uncommon.
From the coeliac nodes, lymph passes to the cisterna chyli, the thoracic duct and its termination in the formation of the left brachiocephalic vein. In some cases of upper abdominal malignant disease, particularly stomach cancer, involvement of left supraclavicular nodes may occur, presumably because of their proximity to the termination of the main thoracic duct. This, when present, is known as Virchow’s node.
11.6. Midgut and hindgut
Midgut and hindgut extend from the second part of the duodenum to the anal canal. They receive blood from the superior and inferior mesenteric arteries, and venous blood drains to the portal system. Lymph drains to mesenteric nodes, thence to preaortic nodes and the cisterna chyli.
You should:
• describe the disposition of the jejunum and ileum
• describe the disposition and surface anatomy of the caecum, ascending colon, transverse colon, descending colon and sigmoid colon
• describe the blood supply of midgut and hindgut and the importance of the marginal artery.
Midgut
The midgut extends from the duodenal papilla to (roughly) the distal end of the transverse colon (splenic flexure), and hindgut extends from there to the pectinate (dentate) line of the anal canal. For the third and fourth parts of the duodenum, see above.
Small bowel: jejunum and ileum
At the duodenojejunal flexure, the gut tube once again becomes mesenteric and the first (about) two-fifths of the mesenteric small bowel is the jejunum, the remainder the ileum. Anatomically they may be differentiated by the pattern of arteries in the mesentery, and the jejunal walls are somewhat thicker, but neither of these matters to anyone except surgeons. The mesentery of the jejunum and ileum is known simply as ‘the mesentery’. Originally in the midline, it has shifted during development so that it runs from above left to bottom right. Branches of the superior mesenteric vessels pass in it.
Inside the jejunum, the mucosa forms prominent folds: the plicae circulares.
Meckel’s diverticulum
Within about 1m or so of the distal end of the ileum is the site of the embryonic vitellointestinal duct attachment, and a remnant of this duct may persist: Meckel’s diverticulum. It is clinically important in that it may contain ectopic gastric mucosa, which secretes acid and causes bleeding from the intestinal mucosa. It should be included in the differential diagnosis of anyone with otherwise unexplained blood loss, especially children.
Peyer’s patches
These are aggregations of lymphoid tissue in the wall of the small intestine. In certain conditions (e.g. lymphomas) these may enlarge and cause intestinal obstruction.
Carcinoid tumour
Tumours of the small intestine are rare, but occasionally the neuroendocrine cells scattered throughout the epithelium undergo neoplastic change resulting in overproduction of pressor (causing blood pressure to increase) amines. This may present as episodes of increased bowel movements, diarrhoea and hypertension and other cardiovascular effects.
Large bowel
Caecum and appendix
The ileocaecal junction is marked by a valve. The surface marking of the caecum and base of the appendix is McBurney’s point. The appendix is of variable length and position: it usually lies retrocaecally but may extend down into the pelvis and give rise, when inflamed, to pelvic pain. See ‘Appendicitis and pain’ (section 11.8, p. 131).
Palpating the caecum
A hard mass in the right iliac fossa is strongly suggestive of caecal disease (e.g. cancer).
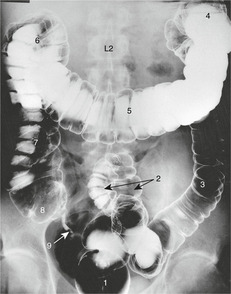
Colon
There are four parts:
• ascending
• transverse
• descending
• sigmoid.
The colon is distinguished by the concentration of longitudinal muscle in its wall into three broad bands, the taenia coli. They converge at the appendix. They are responsible for powerful peristaltic movements that convey the increasingly solid faeces towards the anus. They are responsible for another characteristic feature of the colon – it is as if they are shorter than the colon itself, so the colon is ‘gathered’ to form sacculations or haustrations.
The ascending, transverse and descending colons form three sides of a rectangle, the two angles being the hepatic and splenic flexures. The ascending and transverse (or most of it) are midgut derivatives, so are supplied by the superior mesenteric artery. The descending colon is a hindgut derivative and is supplied by the inferior mesenteric artery. Ascending and descending colons are retroperitoneal and so are not usually mobile, but the transverse colon has a mesentery – the transverse mesocolon – that may be sufficiently extensive for the transverse colon to loop down for some distance. The descending colon is often palpable on the left side of the abdomen, particularly if it contains faecal matter.
The sigmoid colon has a mesentery (the sigmoid mesocolon) and meets the rectum in front of the body of S3, as the gut tube loses its mesentery and once again becomes retroperitoneal. This junction is known as the rectosigmoid junction; recto-coming first because clinically it is usually considered from the bottom up, as when viewed through a sigmoidoscope or at a barium enema radiographic examination.
Rectum
The rectum and anal canal are considered with other pelvic and perineal structures (see section 11.12).
Diverticular disease
Repeated straining at stool, such as may result from a diet lacking fibre, may cause small out-pouchings of the colonic lumen through weak spots in the muscular coat of the colon. These diverticula may be apparent on barium examination of the colon (diverticulosis) and may become inflamed (diverticulitis) with episodes of abdominal pain.
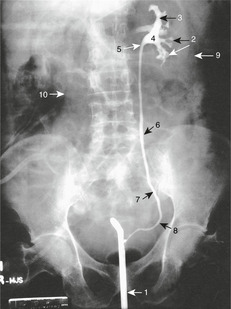
Radiology of the large bowel (Fig. 11.22)
The colon and rectum may be demonstrated radiologically by a barium enema: barium is injected through the anal canal and pumped up to, usually, the caecum.
Blood supply of midgut and hindgut (Fig. 11.23)
The midgut artery is the superior mesenteric (origin: vertebral level T12/L1). The hindgut artery is the inferior mesenteric (origin: about vertebral level L3).
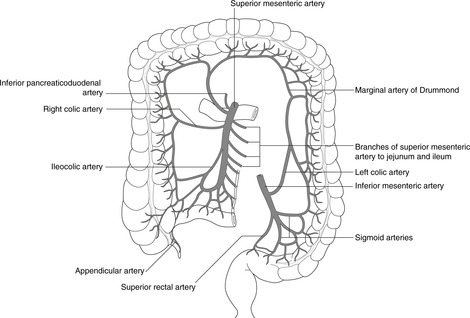 |
| Fig. 11.23 |
Superior mesenteric artery: main branches
• Inferior pancreaticoduodenal: as name suggests.
• Right colic: ascending colon.
• Jejunal and ileal: as names suggest. Since coils of ileum hang down into the pelvic cavity, on an arteriogram it appears as if branches of the superior mesenteric pass down into the pelvis.
• Ileocolic, appendicular: as names suggest.
• Middle colic: transverse colon.
Inferior mesenteric artery: main branches
• Left colic: descending colon.
• Sigmoid colic: sigmoid colon.
• Superior rectal or superior haemorrhoidal: rectum and upper part of anal canal.
Marginal artery
Branches to the colon from both mesenteric arteries form the marginal artery (of Drummond) – an arterial anastomosis along the mesenteric border of the colon that allows the descending colon and sigmoid colon to receive sufficient arterial blood from the superior mesenteric artery even if the inferior mesenteric artery is ligated. The converse does not hold: the inferior mesenteric artery does not supply enough blood to the marginal artery to allow the ligation of the superior mesenteric artery.
Lymph drainage of midgut and hindgut
Midgut: duodenum, small intestine, ascending and transverse colons
This is to nodes in the mesentery, and preaortic nodes around the origin of the superior mesenteric artery from the aorta. It then passes to the cisterna chyli and thoracic duct.
Hindgut: descending and sigmoid colons, rectum, upper part of anal canal
This is to nodes in the posterior abdominal wall and the sigmoid mesentery, and preaortic nodes around the origin of the inferior mesenteric artery from the aorta. It then passes to the cisterna chyli and thoracic duct.
11.7. Portal venous system: venous drainage of the gut tube and associated organs (Fig. 11.24)
All venous blood from the intestinal bed drains to the liver through the portal vein. Liver disease that impairs this may induce anastomoses between the portal and systemic venous systems.
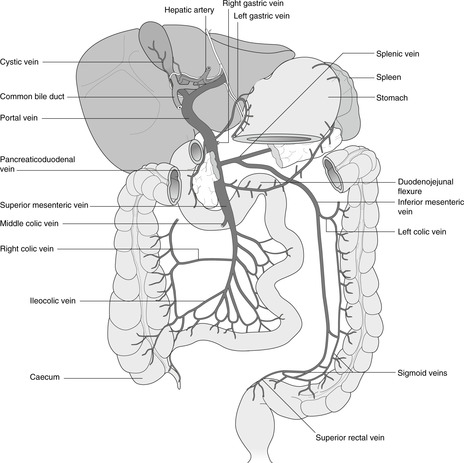 |
| Fig. 11.24 |
Portal system, portal hypertension, portosystemic anastomoses
Venous blood from the abdominal gut tube, spleen and pancreas passes in the inferior and superior mesenteric veins and the splenic vein, which unite to form the hepatic portal vein (usually known simply as the portal vein) behind the neck of the pancreas. The portal vein then passes in the free edge of the lesser omentum to the liver, dividing into right and left branches before branching to reach all parts of the liver. By this means, all nutrients absorbed through the intestinal mucosa pass first to the liver.
Blood which enters the liver, whether by portal vein or hepatic artery, passes through the hepatic sinusoids to the central veins. These unite to form (usually) three hepatic veins opening directly into the inferior vena cava as it passes through the liver on its way to the right atrium of the heart. In liver disease in which blood flow through the sinusoids is either impaired or blocked (e.g. certain forms of cirrhosis) this leads to a build-up of back pressure in the portal vein and its tributaries – portal hypertension – which can cause engorgement of the intestinal venous bed and enlargement of the liver and/or spleen (hepato/spleno/megaly). In extreme cases this may lead to blood ‘searching’ for alternative channels to pass from portal vein to inferior vena cava. These anastomoses between portal veins and systemic veins (portosystemic anastomoses) include:
• Connections between veins in and around the falciform ligament, including a recanalised ligamentum teres (umbilical vein), and the veins of the anterior abdominal wall. These can result in enlarged veins of the abdominal wall radiating from the umbilicus: caput Medusae (from Greek mythology).
• Other anastomoses of the posterior abdominal wall and bare area of the liver: clinically insignificant.
Occasionally, surgeons may manufacture an artificial portosystemic anastomosis to relieve severe portal hypertension. There are several options for this: one is to make a communication in the region of the epiploic foramen (of Winslow) between the portal vein and the inferior vena cava: this is a portocaval shunt or anastomosis. Of course, this means that all the material absorbed from the intestines fails to pass through the liver and much of it is toxic. It is a palliative procedure, not a curative one.
11.8. Nerve supply of the gut tube, gut pain
The intestines are innervated by the autonomic nervous system, which modulates the intrinsic neural activity of myenteric plexuses. Pain from the gut tube passes centrally in autonomic neurons and enters the spinal cord in dorsal roots of thoracic spinal nerves, so pain is referred to anterior abdominal wall skin: from foregut structures to the epigastrium, from midgut structures to the umbilical region, and from hindgut structures to the hypogastrium. In addition, upper abdominal disease can irritate the diaphragm giving rise to referred pain in the shoulder as a result of the cervical origin of the phrenic nerve.
You should:
• explain the basic arrangement of gut tube innervation
• list the sites of referred pain from stomach, ileum, caecum and colon
• explain why gall bladder disease can cause shoulder pain
• explain why the pain of appendicitis often shifts from central umbilical to right iliac fossa.
Myenteric plexuses, autonomic influences
A plexus of neurons is situated in and around the smooth muscle layers of the gut wall. These myenteric plexuses possess intrinsic neural activity which is modulated by the action of the autonomic nervous system. Revise Chapter 6.
Sympathetic
Lateral horn cells (preganglionic) of the thoracolumbar spinal cord give rise to axons that pass through the ventral root of thoracolumbar spinal nerves, to white rami communicantes, the sympathetic chain (no synapse) and the splanchnic nerves to arrive at the pre-aortic group of plexuses: coeliac, superior mesenteric, etc. Here, they synapse and postganglionic fibres pass with the arteries to their destination. For nerves to hindgut, see later.
Parasympathetic
Foregut and midgut: the vagus nerves in the abdomen. The vagus nerves enter the abdomen with the oesophagus. They form anterior and posterior trunks which pass close to the lesser curvature in the lesser omentum. Vagal branches pass to the liver and to the pyloric sphincter. Section of these (vagotomy) may be performed to reduce the secretion of gastric acid, but this operation interferes with the sphincter mechanism and disrupts gastric emptying, so a gastrojejunostomy (making a communication between stomach and jejunum) may be required. Pyloric and antral branches of the vagus are known as nerves of Latarjet, the French physician who described them. It is questionable how much vagal activity passes beyond the pyloric sphincter, and it is now accepted that the myenteric plexuses in the gut tube walls form a kind of gut brain; this has its own intrinsic activity which is capable of being modified by sympathetic and (perhaps) parasympathetic activity from elsewhere.
Hindgut: pelvic splanchnic nerves. Cell bodies (preganglionic) in grey matter of S2, 3, 4 segments give rise to axons which pass through the ventral roots of S2, 3, 4 and form the pelvic splanchnic nerves. These pass to the hypogastric plexus where they (probably) synapse, postganglionic fibres passing with branches of the inferior mesenteric artery to their destinations.
Hirschsprung’s disease
This is a rare inherited condition in which neurons of the hindgut (descending and sigmoid colon) myenteric plexuses, normally formed by neural crest cells, are absent. There is thus no intrinsic muscular activity present here and the colon remains narrow and incapable of peristalsis. It presents as intestinal blockage fairly soon after birth and the affected part of the colon must be removed.
Gut pain
• Foregut. Pain from foregut structures is referred to the epigastrium. However, when the disease or inflammation also spreads to involve body wall structures (e.g. parietal peritoneum), pain may also be perceived over the region concerned. Furthermore, gall bladder pain may also be referred to the right shoulder, presumably because of local irritation of the diaphragm as it attaches to the rib cage anteriorly, and since the sensory innervation of the diaphragm is from the phrenic nerve, C3, 4, 5 pain is referred to those dermatomes.
• Midgut and hindgut. Pain from midgut structures is referred to the umbilical region, and from hindgut structures is referred to the hypogastric (suprapubic) region. Again, when the disease or inflammation also spreads to involve body wall structures (e.g. parietal peritoneum), pain may also be perceived over the region concerned.
Appendicitis and pain
The classic picture is one of central abdominal (periumbilical) pain that after some time appears to shift to the right iliac fossa. The explanation usually given is that initially the inflammation involves only the appendix, which becomes distended, and the resulting midgut visceral sensation is referred to the umbilical region. As the disease progresses, the inflamed appendix enlarges and inflammation spreads to the parietal peritoneum of the anterior abdominal wall. This is then perceived as body wall (somatic) pain – well localised and sharp. Why does the appendix become inflamed? Is appendicitis always appendicitis? Ask a pathologist how often a removed appendix is, in fact, normal.
11.9. Posterior abdominal wall, diaphragm and associated structures
Lumbar vertebrae
Revise Chapter 5. Lumbar vertebrae:
• are bigger than thoracic vertebrae, increasing in size from L1 to L5
• lack facets for rib articulations
• possess several other processes for the attachment of muscles particularly associated with the maintenance of the upright posture (the details of these need not concern you).
Posterior abdominal wall
The posterior abdominal wall is formed by muscles and fascia on either side of the vertebral column. The lumbar fascia surrounds these muscles and extends laterally, providing attachment for the sheet muscles of the anterior abdominal wall.
• Postvertebral muscles: erector spinae (more properly sacrospinalis) muscle: the muscle mass behind the rib cage, responsible for our upright posture. You do not need to know details of their construction. They are supplied by dorsal rami of regional nerves and are covered posteriorly by latissimus dorsi muscle attaching the upper limb to the trunk (see Ch. 12).
• Psoas (major and minor). This is attached to the lumbar vertebrae and intervertebral discs and passes down and laterally, deep to the inguinal ligament, to attach to the lesser trochanter of the femur. It is the main hip flexor and is supplied by direct twigs from ventral rami of lumbar nerves 2, 3 and 4. Running on its anterior surface is the genitofemoral nerve (L1, 2). For meat eaters, psoas is better known as a fillet steak.
• Quadratus lumborum muscle: twelfth rib to posterior part of ilium (quadratus lumborum is a lateral flexor of the spinal column).
Diaphragm
The diaphragm is attached posteriorly to both sides of vertebrae T12, L1 and to the right side of L2. In the midline, fibres from both sides arch (median arcuate ligament) over the aorta as it passes down from the thorax. Passing laterally, fibres arch over psoas (medial arcuate ligament) to the transverse process of vertebra L1, and from there they arch over quadratus lumborum (lateral arcuate ligament) to the tip of the twelfth rib. Laterally and anteriorly, diaphragmatic muscle fibres are attached to the internal aspects of ribs, costal cartilages and the sternum.
Orifices
• Vertebral level T8: the inferior vena cava passes through the central tendon. This means that the IVC remains open when the diaphragm contracts and intra-abdominal pressure rises.
• Vertebral level T10: the oesophagus and vagus nerves pass through the muscular portion, and this means that when the diaphragm contracts and intra-abdominal pressure rises, the cardio-oesophageal sphincter closes.
• Vertebral level T12: aorta, cisterna chyli and tributaries of the azygos vein pass behind the diaphragm.
Nerve supply
• Motor: phrenic nerve C3, 4, 5.
• Sensory: phrenic nerve centrally and branches of local intercostal nerves peripherally.
The diaphragm may be irritated by disease of abdominal organs, leading to referred pain in the shoulder tip (because of C3, 4, 5 innervation). Typically, gall bladder disease may give referred pain in the right shoulder region.
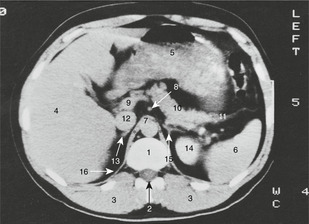
Abdominal CT and MRI scans (Fig. 11.25)
A scan is a widely used way of ‘looking into’ the abdomen to assess the anatomy and seek any abnormality. Figure 11.25 shows an example of a scan, in effect a horizontal section at vertebral level L1 (although of course scans can be taken at any level and in any plane). Now that you have covered a good deal of abdominal anatomy you will be able to understand what you see in this scan.
Nerves of the posterior abdominal wall: lumbar plexus (Fig. 11.26)
These arise form the ventral rami of T12–L5, which form the lumbar plexus.
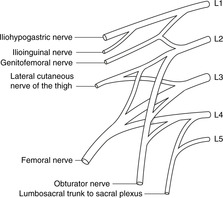 |
| Fig. 11.26 |
The nerves are, in order of importance:
1. Femoral (L2, 3, 4): knee extension, hip and knee joints, anterior thigh sensation.
2. Obturator (L2, 3, 4): hip adduction, hip and knee joints, medial thigh sensation.
3. Lateral cutaneous nerve of the thigh (L2, 3). Sensory, lateral thigh. This passes close to the anterior superior iliac spine where it may be damaged by trauma or belts that are too tight.
4. Ilioinguinal and iliohypogastric (L1): lower anterior abdominal wall.
5. Genitofemoral (L1, 2): anterior scrotum, labia, cremaster.
11.10. Kidneys, ureters, adrenals
The kidneys are retroperitoneal organs posterior to, on the right, the colon and duodenum, and on the left, the colon, spleen and stomach. Behind them are the costodiaphragmatic recesses of the pleural cavities and the lowest one or two ribs. Anomalies of the renal vessels are common. The ureters descend from the renal pelvis to the bladder, passing over the pelvic brim at the sacroiliac joint. There are three sites of ureteric narrowing at which renal stones may stick: the pelviureteric junction, crossing the pelvic brim, and traversing the bladder wall. The adrenal glands are related to the superior poles of the kidneys.
Kidneys (Fig. 11.27)
Position and relations
The kidneys are retroperitoneal. They are higher than you think. Although the right kidney (under the liver) is slightly lower than the left, the hilum of each is at about vertebral level L1 (transpyloric plane). The upper pole is approximately level with T12 vertebra and the lower pole approximately with L2 or L3. Remember, though, that the kidneys move up and down with breathing, and at body temperature the perinephric fat which surrounds them is more liquid than solid so these levels are only guides. Each kidney is surrounded by a tough capsule, which is firmly attached to the fascia over the renal vessels, best seen in a butcher’s shop. Adult human kidneys are not usually lobulated, unlike those of other species (also readily seen at the butcher’s) and also unlike fetal human kidneys, although fetal lobulation persists into childhood and, occasionally, adulthood.
• The important posterior relations of the kidney are the diaphragm and the costodiaphragmatic recess of the pleural cavity. An inexpertly performed renal biopsy, or injection into the kidney, may first enter the pleural cavity and cause a pneumothorax.
• Important anterior relations of the kidney are different on the two sides: they include ascending colon, hepatic flexure and duodenum on the right, and spleen, stomach, splenic flexure and descending colon on the left.
 |
| Fig. 11.27 |
Vessels and anomalies
Both renal arteries arise from the aorta at vertebral level L1. The left renal artery is short but that on the right is longer, passing posterior to the inferior vena cava.
The right renal vein is very short but the left receives both adrenal and gonadal veins before crossing anterior to the aorta immediately below the origin of the superior mesenteric artery.
The kidneys develop low down and ascend during fetal life. This may be arrested and thus a kidney may be lower than its normal position. As the kidneys ascend they acquire new blood vessels and accessory renal vessels are common, especially at the lower poles of the kidneys.
Renal arteries are end-arteries: that is to say their territories do not communicate significantly, so accessory renal arteries should not be tied. Accessory renal veins, however, may be tied since there are significant connections between the territories of individual veins.
Renal pelvis, ureter (Fig. 11.28)
The collecting ducts of the renal tubular system open into:
• minor calyces, which then form
• major calyces, which open into
• the renal pelvis, not to be confused with bony pelvis or pelvic part of the abdominal cavity. This is the most posterior of the structures at the renal hilum: it rapidly narrows to become
• the ureter: this descends approximately in line with the tips of the transverse processes of lumbar vertebrae (an important landmark radiologically), crossing the pelvic brim anterior to the sacroiliac joint and the bifurcation of the common iliac arteries. It then turns forwards and medially to enter the bladder at the level of the ischial spine – also important radiologically.
Renal injuries
The kidneys are at risk from penetrating injuries to the lower rib cage and from trauma (e.g. sports injuries, kicks, etc.) in the renal angle – the inferior angle between the twelfth rib and the vertebral column.
Ureteric constrictions, stones
There are three sites of narrowing where kidney stones are particularly likely to be stuck. They are:
• pelviureteric junction
• as the ureter crosses the pelvic brim
• as the ureter passes through the bladder wall.
Lymph from the kidneys and adrenals
This drains to para-aortic nodes. It is not particularly clinically important.
11.11. Pelvis
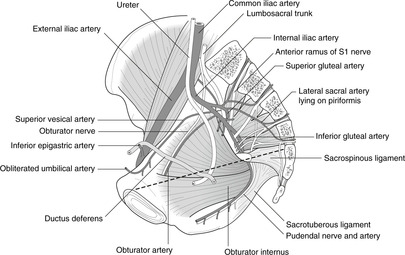
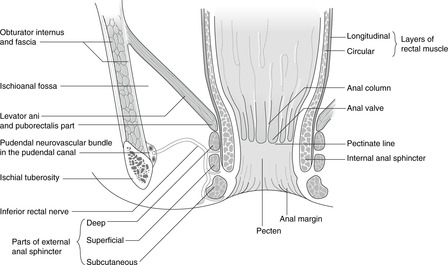
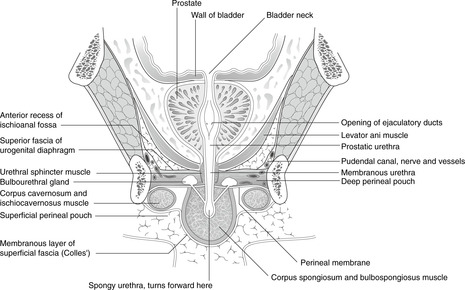
The pelvic girdle is made up of the hip bone, the sacrum and various ligaments. Immediately inside the pelvic walls are the nerves of the sacral plexus contributing to the innervation of the lower limb. Pelvic organs include the sigmoid colon, rectum, internal genital organs, bladder and prostate. The pelvis is bounded inferiorly by the pelvic diaphragm (levator ani muscle), which separates the pelvis above from the perineum below. Pelvic structures are supplied by the internal iliac artery and its branches, and innervated by branches of lumbar nerves and by pelvic extensions of the abdominal sympathetic plexuses. The pelvic diaphragm is important in the maintenance of faecal continence, and is also responsible for helping to maintain the integrity of the pelvic floor, particularly supporting the uterus.
You should:
• list the bones of the pelvic walls and describe the anatomy of the pelvic diaphragm
• describe the arrangement of the sacral plexus and its main nerves: sciatic and pudendal
• describe the anatomy of the rectum
• describe the disposition of the female internal genitalia and the factors responsible for their support
• describe the relationship between the vagina and the rectouterine pouch of Douglas
• describe the disposition of the ureters, bladder, prostate and male genital ducts in the pelvis.
• explain how pelvic disease may involve the vertebral column and spinal nerves.
General disposition
The pelvis and perineum contain organs of the reproductive system, and the caudal terminations of the alimentary and urinary systems. There are, nevertheless, separate anatomical components, as below:
• the caudal or pelvic part of the peritoneal cavity
• a muscular diaphragm (pelvic diaphragm or levator ani muscle) which:
– limits the abdominopelvic cavity inferiorly
– provides support for internal organs (e.g. uterus, bladder, rectal ampulla)
– is penetrated by the distal portions of the alimentary, urinary and reproductive systems; and
– contributes to the sphincter mechanisms for gut tube and urinary system
• the perineum: the area caudal or inferior to the pelvic diaphragm.
The perineum is concerned largely with the external genitalia, and the effluent and sphincters of the gut tube and urinary system. Perineal structures are cloacal derivatives (Latin: cloaca = sewer), and are supplied by the (internal) pudendal artery and the pudendal nerve (S2, 3, 4).
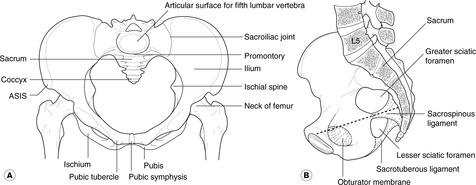
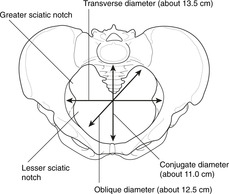
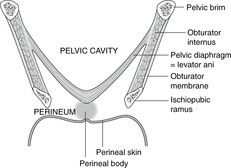
Bony pelvis, pelvic girdle (Fig. 11.29)
This is made up of the hip bones, sacrum, and ligaments and muscles associated with them.
• Hip (innominate) bone. Made up of three bones, ilium, ischium and pubis, which fuse together during adolescence.
• Sacrum. Five fused vertebrae, coccyx attached caudally.
The articulated pelvic girdle looks like a narrow bowl with, on top, two large flattened ‘handles’ or wings. The area above the wings is the greater or false pelvis (terms of little use) and the bowl is the true pelvis. The ridge forming the border between the two is the pelvic brim and marks the pelvic inlet. The inferior extent of the true pelvis is marked by the pelvic outlet, made up of the two inferior pubic rami, the ischial tuberosities, the sacrotuberous ligaments and the sacrum and coccyx. Between the inlet and outlet is the birth canal, so-called for obvious reasons.
Sexing the pelvis
Compared with the female, the male pelvis has:
• a more acute subpubic angle (in the female it is similar to that between thumb and index finger in a hand in neutral position; in the male it is similar to the angle between index and middle fingers)
• more inturned ischial spines
• a sacrum that projects more anteriorly.
It can be difficult to pronounce on the sex of an isolated pelvis, and it is a skill that is unnecessary unless you are concerned with archaeology or forensic science. You may be asked to give an opinion based on a radiograph; my tip is to look for the soft tissue shadow of the penis since this is usually a fairly reliable guide to the sex of the individual.
Surface anatomy
• The iliac crests are palpable throughout their length. You should be able without hesitation to put your fingers on the anterior superior iliac spine and identify it on radiographs and the skeleton. The posterior superior iliac spine marks the posterior end of the crest: it is always marked by a skin dimple, no matter how fat the person.
• The pubic symphysis is palpable in the midline, and the pubic tubercle is about 1.5cm lateral to it. The pubic symphysis and the pubic tubercles are used in the examination of the inguinal region.
Posteriorly, the ischial tuberosity is palpable (this is what you sit on) and the ischial spines are palpable on rectal or vaginal examination.
Ligaments and membrane
• Inguinal ligament: anterior superior iliac spine to pubic tubercle.
• Sacrotuberous ligament: sacrum to ischial tuberosity.
• Sacrospinous ligament: sacrum to ischial spine.
The last two ligaments convert two notches on the hip bones, the greater and lesser sciatic notches, into the greater and lesser sciatic foramina (Fig. 11.30).
The obturator foramen, facing anteroinferiorly, separates the superior pubic ramus above from the inferior pubic ramus and ischial ramus below. It is closed by the obturator membrane.
Walls of the pelvis
Pelvic walls consist of the bones and ligaments as above, the obturator internus muscle on the internal aspect of the obturator membrane, and piriformis muscle arising from the anterior aspect of the sacrum and passing to the gluteal region through the greater sciatic foramen.
Sacral plexus (Fig. 11.31)
The nerves forming the sacral plexus are immediately adjacent to (internally) the pelvic walls. All roots (L4–S3) unite to form the sciatic nerve which is in fact two nerves, the tibial and the common peroneal (note: a word referring to the fibula in the leg – not perineal) or common fibular nerve.
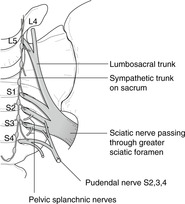 |
| Fig. 11.31 |
Other branches of the sacral plexus are:
• superior gluteal L4, 5, S1: hip abduction, weightbearing
• inferior gluteal L5, S1, 2: powerful extension
• pudendal S2, 3, 4: the perineum.
Contents of the pelvis
The pelvis contains the sigmoid colon and rectum, the termination of the ureters and the bladder and prostate, the ovaries, Fallopian tubes, uterus and upper part of the vagina, and the main nerves and arteries supplying these organs and the lower limb.
Pelvic diaphragm, perineal body (Fig. 11.32)
This is a sheet of voluntary muscle, also called levator ani or the pelvic floor, separating the pelvic part of the peritoneal cavity above from the perineum below. It is a funnel pointing inferiorly, the outer edges of which rest against the pelvic walls in a circle extending from behind the pubic symphysis, over the obturator membrane, ischial spine, sacrospinous ligament and the anterior aspect of the sacrum at about S4 (see Figs 11.29B and 11.34). It has several constituent parts, the names of which you do not need to know except for puborectalis which is described with the anal sphincters (p. 150). It is supplied by small branches from sacral nerves.
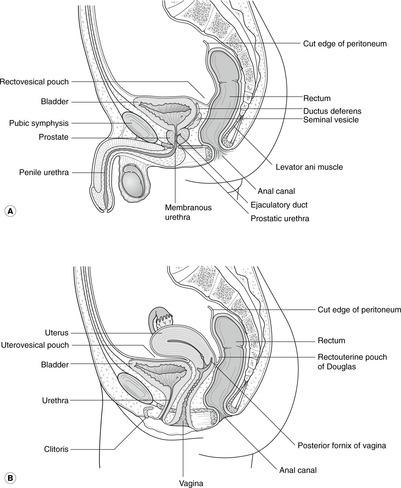 |
| Fig. 11.34 |
Besides its function as part of the urinary and anal sphincters, it is important in providing support for pelvic organs, particularly the uterus and bladder.
Blood vessels of the pelvis
Pelvic blood vessels lie inside the plane of the nerves.
Common iliac artery
From the bifurcation of the aorta, the common iliac arteries pass down and laterally. As they cross the pelvic rim, near the sacroiliac joint, they divide into:
• external iliac: this heads for the midpoint of the inguinal ligament and the lower limb
• internal iliac: this supplies all the contents of the pelvis and perineum and sends small branches to the lower limb.
Internal iliac artery and its main branches (Fig. 11.33)
• Branches which supply the body wall (not important): iliolumbar and lateral sacral.
• Visceral branches. It is not necessary to memorise these, simply know that they exist. Think of a pelvic organ and name an artery after it: uterine, superior and inferior vesical, etc. The only pelvic organ not supplied by the internal iliac artery is the gonad (artery from the aorta directly).
Course of the pudendal neurovascular bundle (Fig. 11.33)
All perineal structures receive arterial blood via the pudendal artery, and are innervated by the pudendal nerve (S2, 3, 4). The pudendal neurovascular bundle leaves the pelvis through the greater sciatic foramen, passes over the external aspect of the ischial spine, and turns medially again through the lesser sciatic foramen. Remember that the outer margin of the funnel-shaped pelvic diaphragm is attached to the internal aspect of the ischial spine and so the pudendal neurovascular bundle has, by this manoeuvre, passed from above the diaphragm to below it without having to penetrate it.
Veins
These mirror the arteries. Tributaries conveying blood from the pelvis and perineum eventually unite to form the internal iliac vein. This unites with the external iliac vein (blood from the lower limb) to form the common iliac vein, and the two common iliac veins unite to form the inferior vena cava. The gonadal veins drain directly to the inferior vena cava on the right, and to the left renal vein on the left.
Venous connections, spread of malignancy
In addition to the named veins, there are numerous connections (Batson’s veins) between pelvic veins and the internal vertebral venous plexus. They allow disease to spread readily from pelvic organs to the vertebral column and may result in, for example, cancer of the prostate causing backache and symptoms of lumbar nerve root entrapment.
Pelvic cavity in the female and male (Fig. 11.34)
In the male the pelvic part of the peritoneal cavity is limited by the side walls of the pelvis, the rectum behind and the bladder and anterior abdominal wall below and in front. It contains coils of ileum.
In the female, the pelvic cavity is partially divided into a smaller anterior portion and a larger posterior portion by a side-to-side fold of tissue projecting up from the pelvic floor. This is the broad ligament, or broad ligament of the uterus. It is formed embryologically by two ingrowths from the sides, which unite in the midline. It contains in the midline the uterus and in its superior margins the uterine or Fallopian tubes extending laterally. Underneath the Fallopian tubes, lateral to the uterus, the broad ligament contains nothing in particular except some embryological remnants of the male genital system that may occasionally become involved in disease (epoöphoron, paroöphoron). Passing from back to front in the base of the broad ligament are the ureters.
Rectouterine pouch of Douglas, uterovesical pouch
The broad ligament is angled forwards so that the posterior surface is more superior, and the anterior surface more inferior. That part of the cavity behind and above the ligament is the rectouterine pouch of Douglas which contains coils of ileum.
In front of (inferior to) the broad ligament is the uterovesical pouch. It is normally empty, that is to say its peritoneal surfaces are in contact with each other, and insignificant.
Uterus and vagina (Fig. 11.35)
These are midline structures. The uterus has three parts:
• cervix, which projects into the vagina
• body, the main bulk
• fundus, that part between and above the entry of the two Fallopian tubes.
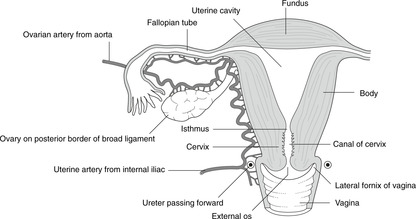 |
| Fig. 11.35 |
The vagina is angled upwards and backwards. The cervix of the uterus projects into its upper anterior wall, the recesses around the projecting cervix being the fornices: one anterior, one posterior (superior), and two lateral. An important relation of the lateral fornix is the ureter which is between the lateral fornix and the uterine artery.
The rectouterine pouch of Douglas directly overlies the superior (posterior) vaginal fornix, and abscesses in the pelvic cavity may be drained through the vagina in the female.
External os and cervical smears
This is the opening between the vagina and the cavity of the cervix. Just inside it is the site of the squamocolumnar junction. The spatula used to take a cervical smear is shaped with a long arm to be inserted in the cervical opening for columnar cells, and a short arm which remains outside it for squamous cells. One hopes not to see squamous cells near the tip of the long arm.
The external os in a woman who has not borne children is more or less circular. After the birth of the first child it becomes, and remains, slit-like.
Mechanical support
The two main factors in the support of the uterus are:
• Pelvic diaphragm which acts as a sling supporting these organs. It clasps the cervix and vagina.
• Ligaments on the upper surface of the pelvic diaphragm:
– cardinal, or lateral cervical, or Mackenrodt’s
– pubocervical
– sacrocervical.
Damage to, or stretching of, these structures or of the perineal body (trauma, repeated childbirth) may result in uterine and/or vaginal prolapse which may be so severe that the uterus is palpable or even visible at the vaginal opening.
Blood supply
• Fundus of uterus and Fallopian tubes: branches of the ovarian artery (from the aorta).
• Body and cervix of uterus, and vagina: uterine and vaginal arteries (from internal iliac artery).
Nerve supply
Sensory fibres from the uterus pass back to the central nervous system in autonomic nerves. The pathways are not clearly understood. Uterine pain is felt in the lower back and perineum.
Lymph drainage
• From lower vagina: inguinal nodes.
• From upper vagina, cervix and lower body: internal iliac nodes.
• From upper body and fundus: para-aortic nodes (by lymph channels running with the ovarian arteries).
Fallopian or uterine tubes
The Fallopian tubes are extensions of the upper lateral corners of the uterine cavity along the upper margin of the broad ligament. However, before they reach the side walls of the pelvis, they open into the peritoneal cavity on the posterior (superior) surface of the broad ligament. In the female, therefore, there is a potential route for foreign organisms to enter the peritoneal cavity from the external environment. This is not so in the male, where the peritoneal cavity is entirely sealed.
The Fallopian tube has four parts, from medial to lateral:
• interstitial or intramural: in the thickness of the uterine wall
• body: lateral to that
• ampulla: slightly wider, fertilisation normally takes place here
• fimbriated end: the opening into the peritoneal cavity. This is mobile.
Ovaries
The ovaries are attached to the posterosuperior surface of the broad ligament by the mesovarium, through which branches of the ovarian vessels pass to and from the ovary. Although on the back of the broad ligament, the ovaries are sufficiently close to the side walls of the pelvis for an inflamed ovary to irritate the tissue supplied by the obturator nerve on its way to the obturator foramen. Pain from ovarian disease, or even a heavy menstrual period, may be referred to the territory of the obturator nerve: hip and medial thigh.
Ovarian vessels
Ovarian veins show a similar pattern, the right passing directly to the inferior vena cava, and the left to the left renal vein (as with the testis).
Ovarian lymphatics, together with those from the fundus of the uterus and the Fallopian tubes, pass directly to para-aortic nodes.
Round ligaments: gubernaculum in the female
• The round ligament of the ovary is a cord-like thickening on the posterior (superior) aspect of the broad ligament between the ovary and the junction of the Fallopian tube and the uterus.
• The round ligament of the uterus is a similar thickening on the anterior (inferior) aspect of the broad ligament from the same part of the uterus to the deep inguinal ring; it passes through the inguinal canal to the subcutaneous tissue of the labia majora outside the superficial inguinal ring.
• They are two different parts of the same thing, the embryological gubernaculum, and are otherwise entirely insignificant.
Ureters, bladder (Fig. 11.36)
The urinary bladder lies between the peritoneum of the anteroinferior pelvic cavity and the pelvic diaphragm, upon which it rests.
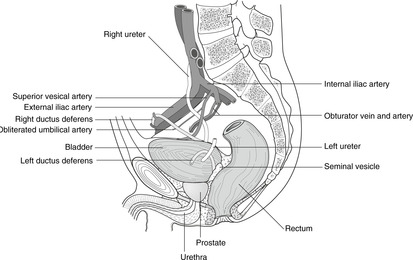 |
| Fig. 11.36 |
The ureters enter the posterior surface of the bladder near the midline. The area of bladder wall bounded by the two ureteric orifices and the single midline urethral orifice is the trigone. It is the part of the bladder that expands least as the bladder fills.
The bladder neck is the term given to the bladder as it narrows down to open into the urethra. In the male, this is surrounded by the prostate gland.
The muscle of the bladder wall is the detrusor muscle. It is involuntary (smooth) muscle.
Nerve supply
Motor supply of the bladder muscle is from the pelvic splanchnic nerves, S2, 3, 4. Sensory fibres pass in the same nerves to enter the same segments of the spinal cord, with their cell bodies in the dorsal root ganglia of S2, 3, 4. The function of sympathetic fibres to the bladder has not been fully elucidated.
Bladder pain is referred to the lower abdomen, perineum and back.
Venous blood and lymph vessels
These drain to the internal iliac veins and nodes.
Median umbilical ligament, patent urachus
Extending in the midline from the bladder to the umbilicus is the obliterated remnant of the urachus, itself the successor of the allantois. Should this fail to close before birth, a patent urachus will result in urine leaking from the umbilicus of the newborn.
Prostate gland, seminal vesicle, ductus deferens (Fig. 11.36)
These are reproductive organs, secreting fluid into the urethra to provide sustenance for the great journey that the spermatozoa must undertake.
In the male, the prostate gland surrounds the neck of the bladder and rests upon the pelvic diaphragm. The seminal vesicle is a tightly coiled gland above and behind the prostate on the posterior wall of the bladder. As the urethra passes through the prostate, it receives the ejaculatory ducts on each side, each ejaculatory duct formed by the union of the ductus (vas) deferens and the seminal vesicle.
Lobes of the prostate
These are not anatomically or functionally separate lobes, merely different areas.
• Anterior lobe: anterior to the urethra.
• Lateral lobes: lateral to the urethra. Posteriorly, there is a slight midline sulcus that separates the two lateral lobes.
• Posterior lobe: the posterior parts of both lateral lobes.
• Median lobe: the area of the gland in the midline posterior to the urethra, bounded by it and the two ejaculatory ducts.
Prostatic enlargement, palpation of the prostate, rectal examination
Enlargement of the prostate gland may be benign or due to cancer and is common in old men. It may compress the urethra, leading to difficulty in passing urine (urinary retention). This is particularly so if the median lobe is involved.
Insertion of the examiner’s finger, suitably protected, into the rectum is a routine part of a full clinical examination. Apart from any anal or rectal disease, it is usually possible to feel the prostate gland, its midline posterior sulcus, and possibly even the seminal vesicle. In a patient with urinary retention, a palpably enlarged prostate is indicative of the root of the problem: if the posterior part of the gland is enlarged, the chances are that the whole gland is also enlarged. Unfortunately, the converse does not hold: the fact that the posterior lobe is not palpably enlarged does not mean that the gland is not the cause, since the median lobe, the most likely culprit, is not palpable.
Prostatic malignancy and the vertebral column
Because of the connections between the pelvic veins and the vertebral venous plexuses, prostatic malignancy may spread to the vertebral column. It may present as a collapsed vertebra as a result of erosion of the vertebral body by secondary deposits, or by shooting pains down the legs, as a result of nerve entrapment resulting from vertebral collapse.
Blood supply and lymph drainage
Prostatic arteries arise from the internal iliac. Veins drain to the internal iliac veins and connect with the vertebral venous plexuses. Lymph vessels drain to internal iliac nodes.
The nerve supply of the prostate is not important.
Ductus (vas) deferens (Fig. 11.36)
From the testis the ductus passes through the inguinal canal. After traversing the deep inguinal ring it passes lateral to the inferior epigastric artery and turns medially and down, crossing the ureter and passing between the bladder and the medial aspect of the iliac vessels and their branches. It approaches the prostate gland from behind, above the seminal vesicle, the duct of which it joins to form the ejaculatory duct entering the posterolateral aspect of the prostate gland and the urethra.
Rectum (Fig. 11.37)
Already you can see that the human rectum is not well named: it is not straight. There are, furthermore, three lateral curvatures with corresponding mucosal folds, sometimes called the valves of Houston. These folds project into the lumen, from above down (or below up), from the left, from the right, and from the left, thus causing reciprocal bending of the rectal channel, from above down (or below up), to the right, to the left, and to the right. The mucosal folds are easily torn and so you should be careful when inserting instruments into the rectum.
Blood supply. Being a derivative of hindgut, the rectal blood supply comes from branches of the inferior mesenteric artery. Venous blood drains to the inferior mesenteric vein and the portal vein.
Nerve supply. See later.
Lymph drainage. This is to mesenteric nodes and internal iliac nodes.
Rectoanal junction
Opinions differ about where the rectum becomes the anal canal: my view is that the pelvic diaphragm is the demarcation. The anal canal is considered in section 11.12 (p. 150).
11.12. Perineum
The perineum is the area inferior to the pelvic diaphragm (levator ani muscle). All perineal structures are supplied by the pudendal artery and the pudendal nerve (S2, 3, 4). It contains the anal canal, the ischioanal (ischiorectal) fossa on either side of the anal canal, and the external genitalia. It is partly divided by the urogenital diaphragm between the ischiopubic rami, which contains muscles of the external (voluntary) urinary sphincter (sphincter urethrae). The perineal body, anterior to the anal canal, is a fibromuscular node and focal point for the activity of both pelvic and urogenital diaphragms: damage to it may result in sphincter incontinence and prolapse of pelvic organs.
You should:
• describe the anatomy of the anal canal in relation to the pelvic diaphragm, and the watersheds of the anal canal
• explain the mechanism of faecal continence
• describe the general arrangement of the perineum
• describe the anatomy of the urethra in the male and female, and the anatomy of urinary continence
• describe the anatomy of the external genitalia, and how to catheterise the urethra in male and female.
Spatial considerations in the perineum: the ischioanal (ischiorectal) fossa (Fig. 11.37)
Pudendal vessels and nerve: course and branches
Look at Figure 11.33 to remind yourself how clever the vessels are to pass from above the pelvic diaphragm to below it without having to penetrate it. Once in the perineum, the pudendal neurovascular bundle makes its way downwards and forwards on the lateral wall of the ischioanal fossa, which is formed by obturator internus muscle. It is enclosed by a fascial sheath called Alcock’s canal (pudendal canal). The nerve and artery give branches to the anal canal and eventually reach the back of the urogenital diaphragm, which they supply (perineal branches). Other branches continue to the external genitalia (dorsal nerve/artery of the penis/ clitoris).
Pudendal nerve block
By injecting local anaesthetic agents around the ischial spine, all perineal structures may be anaesthetised. This can be useful in childbirth or in any surgical procedures in the perineum. The injection point can be located by palpating the ischial spines by lateral pressure of the fingers in the vagina until the ischial spine is located. The needle would be inserted through the wall of the vagina.
Urogenital diaphragm (Fig. 11.38, Fig. 11.39 and Fig. 11.40)
This incomplete shelf of muscle runs between the inferior pubic rami and merges with the perineal body in the midline posteriorly. It is penetrated by the urethra (in both sexes) and, in the female, by the vagina. It consists of, from above down:
• a thin fascial layer with no particular name
• a sheet of voluntary muscle, the perineal muscles, which form the external urinary sphincter and are supplied by the pudendal nerve – this muscle sheet is somewhat rearranged in the female where the vagina passes through it, but you need not worry about this
• a thick fascial layer called the perineal membrane.
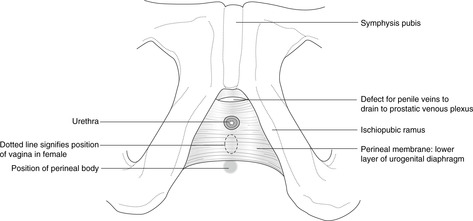 |
| Fig. 11.38 |
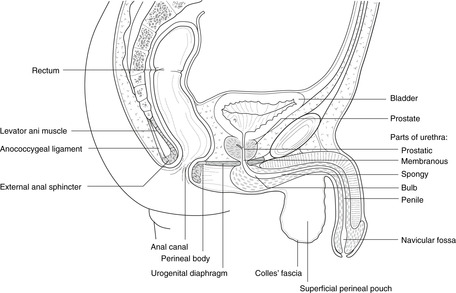 |
| Fig. 11.39 |
Female urethra
From the bladder neck the urethra passes inferiorly through the urogenital diaphragm. Since the inferior layer of the urogenital diaphragm is the perineal membrane, this is sometimes called the membranous portion of the urethra. From here the urethra continues down directly to open at the vestibule.
Male urethra (Figs 11.38, 11.39)
• Prostatic urethra. From the bladder neck the urethra enters the prostate gland. It is here quite wide and U-shaped. Below the prostate gland, it passes through the urogenital diaphragm as the:
• Membranous urethra. Immediately below the perineal membrane there is a slight dilatation, the urethral bulb, and it turns forwards to run immediately inferior to the perineal membrane as the:
• Spongy urethra. Here the urethra is surrounded by caverns of venous blood, the corpus spongiosum, or spongy erectile tissue, and smooth muscle fibres, the bulbospongiosus muscle. This forms one of the three tubes of erectile tissue that make up the penis, and it is enlarged at its tip to form the glans penis. The spongy urethra continues forwards in the penis as the:
• Penile urethra. Slightly before its termination there is another slight dilatation, the navicular fossa, in the region of which a mucosal fold projects into the urethra from what would be the superior aspect of the urethra with the penis pointing forwards.
Catheterisation of the male urethra
• First, avoid the mucosal fold near the navicular fossa by aiming the catheter down, assuming the penis is pointing forwards, held in your hand.
• Next, push the catheter gently back until you meet increased resistance. The catheter tip is now at the bulb with the right-angled bend.
• Now turn the penis inferiorly and gently ease the catheter round the corner. If you are rough you may rupture the urethra.
• The next difficult region is the membranous urethra as it penetrates the urogenital diaphragm. Remember that in an old man you are likely to be inserting the catheter because of urinary retention, and so the bladder will be very full and the poor old man will be contracting his urinary sphincter very tightly indeed. This makes it even harder to advance the catheter. After you have managed this, the rest is easy: the prostatic urethra is wide and easily distensible and the catheter will go straight into the bladder. The old man is now very relieved and may well be grateful to you for ever.
Superficial and deep perineal pouches, Colles’ fascia
• Deep perineal pouch. This is the area of the urogenital diaphragm between the upper and lower fascial components. It is a silly term, since it is full of perineal muscles.
• Superficial perineal pouch. This is the area inferior to the perineal membrane, bounded posteriorly by the perineal body. Urine may leak into this area if the urethra is ruptured. Such a urinary leak is limited by Colles’ fascia – the superficial fascia of the perineum (Figs 11.39, 11.40), and urine may spread up the superficial tissues of the anterior abdominal wall.
Surface anatomy of the perineum
The surface anatomy is usually described as if the patient were in ‘lithotomy position’: lying on the back, with the lower limbs elevated and the feet in stirrups. A line joining the two ischial tuberosities divides the perineum into two approximate triangles:
• the urogenital triangle anteriorly, roughly coexistent with the urogenital diaphragm internally
• the anal triangle posteriorly.
Female external genitalia: the vulva (Fig. 11.41)
The vulva is the name given to the female external genitalia. The vestibule signifies that area between the two labia majora. Internally, the bulbospongiosus and ischiocavernosus muscles are much as in the male, except smaller. The clitoris has erectile tissue as does the penis. Lymph drains to inguinal nodes.
Episiotomy, perineal tear
Look at Figure 11.41. In order to enlarge the mother’s vaginal orifice for the baby’s head, an incision is sometimes made posteriorly from the vagina into the soft tissues of the perineum and perineal skin. This is an episiotomy. If it is performed in the midline posteriorly from the vagina, there is a risk of damaging the perineal body, immediately deep to this region. For this reason the procedure is normally performed obliquely. A perineal tear which damages the perineal body may result from direct trauma, or uncontrolled expulsion of the fetal head during birth. It would result in functional loss of both muscular diaphragms associated with the perineal body: urinary incontinence, faecal incontinence and pelvic organ prolapse.
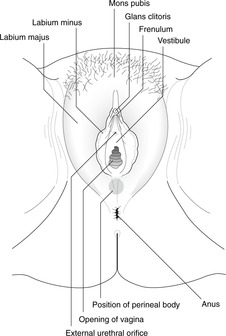 |
| Fig. 11.41 |
Male external genitalia
• Regard the penis as an enlarged clitoris and labia minora into which the urethra has been diverted.
• Regard the scrotum as the two labia majora that have been stitched together.
This is not simply bizarre fantasy, it is embryological fact. Hypospadias, the commonest penile congenital anomaly, is simply some degree of reversion to the female, or basic, form.
Penis (Fig. 11.42)
The terms ventral and dorsal are applied to the penis in the erect position, so when the penis is dependent, the dorsal surface is in front. Three tubes of erectile tissue form the penis.
• In the ventral midline is the corpus spongiosum that contains the urethra. This is attached to the under surface of the urogenital diaphragm by the bulbospongiosus muscle and is enlarged at its tip to form the glans. Bulbospongiosus is split into two in the female to form the sphincter vaginae.
• On each side, slightly dorsally, is the corpus cavernosum. Each is attached to the inferior ramus of the pubis by the ischiocavernosus muscle, and terminates just proximal to the glans.
These three chambers of venous caverns communicate with each other: this is evident clinically by the treatment of priapism, a painful condition of perpetual erection caused by venous engorgement, in which incision into one of the chambers usually solves the problem. (Priapus was a Greek fertility imp with an enormous penis. Statues of him abound).
An interesting linguistic snippet
The Latin word penis means tail: perhaps its use for the male organ developed as a euphemism so as not to offend the delicate ears of the ladies of Rome. The proper English word is ‘cock’, defined in the Compact Oxford English Dictionary (second edition, 1991, Oxford University Press) as ‘a spout or short pipe serving as a channel for passing liquids through’.
Blood supply of external genitalia
Arteries from the pudendal; veins to the prostatic venous plexus and thence to the internal iliacs.
Lymph drainage of external genitalia
• Clitoris, glans penis, penile urethra: inguinal nodes.
• Urethra inferior to the urogenital diaphragm and bulb: external iliac nodes.
• Membranous urethra and above: internal iliac nodes.
• Labia majora and scrotum: inguinal nodes.
• Ovary and testis: para-aortic nodes.
Nerve supply of external genitalia and perineal skin
• From pudendal nerve and branches:
– S4 around the anus, vulva, posterior scrotum (the anterior scrotum is part of the anterior abdominal wall and is supplied by lumbar nerves)
– S3 more laterally between the legs
– dorsal nerve of the penis or clitoris (mainly S4).
• Twigs from S5 supply a small area at the tip of the coccyx (not important).
Anal canal (see Fig. 11.37)
Opinions differ about anal anatomy, so be prepared for this. From the puborectalis sling of levator ani (see p. 138), the anal canal passes down and backwards to the anal orifice.
Mucosa of the anal canal, columns, valves, pectinate (dentate) line
• Upper part. The mucosa of the upper part of the anal canal is thrown into between 5 and 10 longitudinal mucosal folds, the anal columns. At their lower end, about halfway along the canal, these folds are joined together by mucosal ridges, called valves (not to be confused with valves of the rectum) with a small recess behind, something like a pocket. Mucous glands open into these pockets. The apparent line formed by the valves is the pectinate (dentate) line and it marks the approximate position of several boundaries or watersheds (Table 11.1).
| Above pectinate (dentate) line | Below pectinate (dentate) line | |
|---|---|---|
| Epithelium | Columnar (mucosa) | Stratified squamous (skin) |
| Arteries | Branches of inferior mesenteric, e.g. superior rectal | Branches of internal iliac, e.g. inferior rectal |
| Veins | To the portal system (inferior mesenteric) | To the systemic system (internal iliac veins) |
| Lymph | To mesenteric nodes | To internal iliac and drainage inguinal nodes |
| Nerve supply | Visceral (autonomic): pelvic splanchnic nerves (S2, 3, 4 and sympathetic). Pain is thus dull and poorly defined. | Somatic: inferior rectal from pudendal (S2, 3, 4). Pain is thus sharp and well defined. |
• Middle part. This is lined by skin and is smooth. It is sometimes known as the pecten.
• Lower part (anus). This is lined by hairy skin and is puckered by the sphincters.
Veins
You might suppose that, since the anal canal is a site of anastomoses between the portal and systemic venous systems, it would be involved in the manifestation of liver disease in a way similar to oesophageal varices. You would be wrong: it is not, and nobody knows quite why.
‘Piles’ – haemorrhoids
These are varicose veins of anal columns. As long as they are confined to the area above the pectinate line, they are relatively painless, although they may be uncomfortable, and they may rupture causing bleeding. As soon as they stray into the territory of the somatic nerve innervation below the line, they become … ouch!
Anal sphincters (Fig. 11.37)
• Internal sphincter: smooth muscle, autonomic innervation. This is simply the somewhat expanded inferior termination of the circular smooth muscle component of the wall of the gut tube.
• External sphincter: skeletal muscle, voluntary (somatic) innervation (S2, 3, 4). There are three parts. From outside (anus) in, these are:
– subcutaneous: this is the part that puckers the anal skin
– superficial: this is level with the inferior edge of the internal sphincter
– deep: this is level with the anal columns. The posterior part of the deep part is functionally related and merges with the puborectalis sling of levator ani muscles (pelvic diaphragm). This is why damage to the pelvic diaphragm, or to the perineal body, which is a part of the same mechanism, may lead to loss of sphincter control.
Sacral spinal cord and the perineum: sphincters and sex
You have read that the perineum is innervated by sacral segments 2, 3 and 4. Although the sacral nerves emerge through the sacrum, you should remember that the sacral part of the spinal cord itself from which they arise is actually level with vertebrae T11, T12 and L1. A catastrophic injury to the vertebral column in the low thoracic or upper lumbar region may therefore cause loss of S2, 3, 4 function. In two ‘s’ words, sphincters and sex, the functional implications are incontinence and, in the male, impotence. The sacral nerve roots, like all constituents of the cauda equina, are also liable to injury anywhere between their origin and their foramina of exit from the vertebral canal.
Cauda equina syndrome
Posterior herniation of a lower lumbar intervertebral disc may, if in the midline (rather than lateral), affect the nerve roots in the centre of the cauda equina. These will be those of the sacral nerves, most likely S2, 3 and 4 (See Ch. 5, p. 25; Ch. 6, p. 39). Symptoms of such compression would include sphincter disturbance and pain or numbness in the saddle area (the area of skin in contact with a saddle, were you to sit on one) supplied by these nerves. This is cauda equina syndrome and it can develop rapidly. If your patient develops sudden loss of sphincter control (either or both sphincters), detectable by, for example, assessment of anal sphincter tone, with or without saddle area numbness, it is an emergency. If dealt with quickly enough it can be reversible.
11.13. Autonomic nervous system in the abdomen and pelvis: a review
Revise Chapter 6.
Sympathetic
Preganglionic cell bodies are in the lateral column of grey matter of the thoracolumbar spinal cord. Impulses pass through ventral roots of spinal nerves and white rami communicantes to the sympathetic chain, thence without synapsing to the splanchnic nerves. They arrive at the preaortic group of plexuses, coeliac, superior mesenteric, etc., where they may synapse, postganglionic fibres being delivered to their destinations in the walls of the arteries which supply them. Preganglionic sympathetic impulses to hindgut derivatives pass down the preaortic group of plexuses in front of the aorta and, below the aortic bifurcation, continue into the pelvis as the hypogastric or pelvic plexus, also known as the presacral nerves, synapsing somewhere along the way. In this way sympathetic impulses reach the pelvic organs, postganglionic fibres passing directly to the organs concerned (e.g. bladder, internal genitalia).
The sympathetic chains continue down into the pelvis, uniting as the ganglion impar in front of the sacrum. Between T1 and about L1 or L2 the chain is connected at each segment to spinal nerves by white and grey rami communicantes. Below (and above) this thoracolumbar region, there are only grey rami. Destruction of the sympathetic chains at the lower ends of the aorta and inferior vena cava will interrupt sympathetic outflow to lower lumbar and sacral spinal nerves (for the lower limbs), but will not affect sympathetic outflow to the gut tube or pelvic viscera which parted company with the sympathetic chains higher up through the thoracic (greater, lesser, least) and lumbar splanchnic nerves to gain the preaortic and pelvic plexuses. This procedure is lumbar sympathectomy and is performed to interrupt vasoconstrictor fibres to the lower limbs in the case of peripheral vascular disease.
Parasympathetic
The parasympathetic system in the abdomen supplies only gut tube derivatives: foregut and midgut structures through the vagus, and hindgut (cloacal) structures through fibres originating from segments S2, 3 and 4. These pass into the sacral nerve roots and then, as soon as they have emerged from the sacral foramina, part company with the somatic nerves to form the pelvic splanchnic nerves. Since these are responsible for penile erection, they are also known as the nervi erigentes. You do not need to know the details.
Visceral sensation
These fibres have not been well defined for most abdominal structures, and certainly not for pelvic and perineal structures. They pass back to the spinal cord in nerves which are conveying sympathetic fibres in the opposite direction, or in nerves that convey parasympathetic fibres in the opposite direction, or possibly both. Cell bodies are in the dorsal root ganglion of whichever segment transmits the sensory fibre into the spinal cord and thus pain may be referred to the skin, or other somatic structure, supplied by that segment.
11.14. Summary of surface markings and vertebral levels (Table 11.2)
| Surface marking | Vertebral level | |
|---|---|---|
| Nipple, fourth intercostal space | Liver, upper limit | T7 |
| Xiphoid process | T9 or 10 | |
| Origin of coeliac artery | T12 | |
| Ribs 9–11 posteriorly | Spleen | |
| Origin of superior mesenteric artery | T12/L1 | |
| Tip of ninth costal cartilage, transpyloric plane | Gall bladder, pylorus, duodenojejunal flexure, hilum of kidneys, head of pancreas | L1 |
| Subcostal plane | Origin of gonadal, inferior mesenteric artery (approximate) | L2/3 |
| Umbilicus, just below and to the left | Bifurcation of aorta | L3/4 |
| Highest point of iliac crest (posteriorly) | L3/4 intervertebral disc (for lumbar puncture) | L3/4 |
| McBurney’s point, right iliac fossa | Base of appendix, caecum | L4 |
| Midinguinal point, and 2cm above | Femoral pulse, and deep inguinal ring | Not applicable |
| Pubic tubercle | Superficial inguinal ring | Not applicable |
Single best answer questions
For each numbered question, only ONE of the options lettered a–d is correct.
32. The diaphragm:
a. is penetrated by the inferior vena cava at vertebral level T10.
b. is separated from the bare area of the liver by the hepatorenal pouch.
c. receives motor fibres from the thoracic spinal cord.
d. separates the costodiaphragmatic recesses from the upper poles of the kidneys.
33. Which is NOT at about the level of the transpyloric plane:
a. cardio-oesophageal junction.
b. duodenojejunal junction.
c. hilum of the kidneys.
d. origin of superior mesenteric artery.
34. In the colon
a. the ascending colon has a mesentery.
b. the hepatic flexure is supplied by the inferior mesenteric artery.
c. the sigmoid colon is retroperitoneal.
d. the transverse mesocolon is adherent to part of the greater omentum.
35. An inept appendicectomy incision may lead to a direct inguinal hernia because which of the following nerves may be severed:
a. right genitofemoral.
b. right iliohypogastric.
c. right ilioinguinal.
d. right lateral cutaneous nerve of the thigh.
36. McBurney’s point is:
a. where the linea semilunaris meets right costal margin.
b. one third of the way from the right ASIS to the umbilicus.
c. one third of the way from the umbilicus to the right ASIS.
d. tip of the right ninth costal cartilage.
37. The principal factor in maintaining the position of the uterus is:
a. the broad ligament.
b. the levator ani muscle and ligaments on it.
c. the round ligament of the uterus.
d. the suspensory ligament of the ovary.
38. Concerning the uterus:
a. the cervix is normally retroverted on the vagina.
b. the rectouterine pouch (of Douglas) contains coils of intestine.
c. the ureter passes through the upper part of the broad ligament.
d. the uterovesical pouch is posterior to the uterus.
39. The perineum is:
a. synonymous with ischioanal (ischiorectal) fossa.
b. the lateral compartment of the leg.
c. the part of the pelvis superior to the pelvic diaphragm (levator ani).
d. the part of the trunk inferior to the pelvic diaphragm (levator ani).
40. The upper third of the anal canal:
a. is supplied by somatic pain fibres.
b. lies above the pelvic diaphragm.
c. lies inferior to the dentate (pectinate) line.
d. venous drainage is to the hepatic portal venous system.
41. In the vertebral column:
a. a herniated nucleus pulposus between L3 and L4 may compress the spinal cord.
b. compression of nerve L3 would result in symptoms in the posterior thigh.
c. ligamenta flava are attached to adjacent pedicles.
d. lumbar spinal nerves pass through the superior part of the intervertebral foramina.
42. A midline herniation of a lower lumbar intervertebral disc is most likely to damage nerves that:
a. supply anterior thigh sensation.
b. supply bladder and anal sphincters.
c. supply hip adduction.
d. supply knee extension.
Matching item questions
Questions 56–60: dermatomes and vertebral levels
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. T10
b. T12
c. L1
d. L3–4
e. L5
56. dermatome of umbilical skin
57. dermatome over pubic tubercle
58. vertebral level of oesophageal orifice in diaphragm
59. vertebral level of bifurcation of the aorta
60. vertebral level of highest point of iliac crest
Questions 61–70: lymph drainage
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. internal iliac nodes
b. inguinal nodes
c. external iliac nodes
d. para-aortic nodes
e. coeliac nodes
61. scrotal skin
62. ovary
63. rectum
64. uterine cervix
65. anal canal inferior to pectinate line
66. glans penis
67. lesser curvature of stomach
68. first part of duodenum
69. prostate
70. bladder
Questions 71–75: mesenteries
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. dorsal mesogastrium
b. transverse mesocolon
c. ventral mesogastrium
71. falciform ligament.
72. greater omentum.
73. lesser omentum.
74. structure in which middle colic vessels pass.
75. structure with obliterated umbilical vein in its free edge.
Questions 76–79: lesser sac
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. epiploic foramen (of Winslow), anterior border
b. epiploic foramen (of Winslow), inferior border
d. lesser sac, anterior wall
e. lesser sac, posterior wall
76. duodenum
77. hepatic portal vein
78. pancreas
79. inferior vena cava
Questions 80–90: abdominal arteries
Match the numbered item to the lettered response. Each lettered response may be used once, more than once, or not at all.
a. aorta, direct branch of
b. coeliac artery, or branches of
c. inferior mesenteric artery, or branches of
d. internal iliac artery, or branch of
e. superior mesenteric artery, or branches of
80. adrenal arteries
81. gonadal arteries
82. splenic artery
83. gastric arteries, right and left
84. gastroepiploic arteries, right and left
85. inferior pancreaticoduodenal artery
86. superior pancreaticoduodenal artery
87. middle colic artery
88. sigmoid colic artery
89. superior rectal (haemorrhoidal) artery
90. inferior rectal (haemorrhoidal) artery
Questions requiring short answers
91. In the inguinal canal, what forms (a) the anterior wall; (b) the posterior wall; (c) the roof; and (d) the floor?
92. Describe the testis in the scrotum. Which layer is equivalent to peritoneum? What is the cremasteric reflex? What is a hydrocele?
93. What is the significance of portosystemic anastomoses? What is a caput Medusae? Suggest surgical procedures that might achieve the same purpose. What would be the drawbacks of this?
94. What are the subphrenic spaces? How do they relate to the liver? What is the hepatorenal recess (Morison’s pouch)? What other spaces does this communicate with? Why does all this matter?
95. Describe the vagus nerves in the abdomen. What is vagotomy?
96. How is the uterus maintained in position? What is a uterine prolapse and how may it be caused?
97. What is the pouch of Douglas? How would you drain an abscess in it in (a) a female; (b) a male? Why is this relevant to inexpertly performed abortions?
98. A rugby player is kicked in the back between the left rib cage and the vertebral column. Lower ribs are fractured. There is severe internal bleeding, blood in the urine and the patient is short of breath. Explain.
99. What is the functional significance of the part of levator ani called puborectalis?
100. A 75-year-old man presents with urinary retention, back pain and shooting pains down the legs. Explain.
Self-assessment on Chapter 11: answers
True/false answers
1.
b. True.
c. False. Lymph drainage of scrotal skin is to inguinal nodes; it is drainage of testis that is to para-aortic nodes. This is important.
d. True.
e. False. It passes through the superficial ring, but not the deep.
2.
a. False. Lateral.
b. False. It passes through the superficial but not the deep. The genital branch of the genitofemoral nerve passes through both rings.
c. True.
d. False.
e. True.
3.
a. False. The superior surface of the bladder.
b. True.
c. True.
d. True.
e. True.
4.
a. True.
b. False. The splenic artery is a branch of the coeliac.
c. True.
d. False. It enlarges towards the right iliac fossa.
e. True.
5.
a. True.
b. True.
c. True.
d. False. It is derived from the ventral mesogastrium. (This is difficult and unimportant.)
e. True. It also contains the hepatic artery.
6.
a. True.
b. True.
c. True.
d. True.
e. False.
7.
a. False.
b. True.
c. False.
d. True.
e. False. Gastroepiploics supply the greater curvature.
8.
a. True.
b. False.
c. False.
d. False.
e. True.
9.
a. True.
b. True. Supplying coils of ileum.
c. False. This is from, ultimately, the coeliac.
d. True.
e. False. Anterior.
10.
a. False. Not usually, anyway.
b. False.
c. False.
d. True.
e. True.
11.
a. True.
b. True.
c. False.
d. False.
e. False.
12.
a. True.
b. False. The tail is in contact with the spleen; the uncinate process is within the loop of duodenum.
c. True.
d. True.
e. True.
13.
14.
a. True.
b. True.
c. True.
d. True.
e. False. IVC on right, renal vein on left.
15.
a. False. It receives motor fibres from C3, 4 and 5.
b. True. Intercostal nerves supply the periphery.
c. False. The IVC penetrates the diaphragm at T8, the oesophagus at T12.
d. True.
e. True.
16.
a. False. Foregut derivatives would cause epigastric pain.
b. True. Midgut visceral sensation is referred to the umbilical region.
c. True. Midgut visceral sensation is referred to the umbilical region.
d. False. Hindgut/cloacal derivatives would cause suprapubic pain.
e. False. Hindgut/cloacal derivatives would cause suprapubic pain.
17.
a. True. It is the pudendal nerve, S2, 3, 4.
b. True. It runs in Alcock’s (pudendal) canal.
c. False. It supplies the lower part of the anal canal.
d. True.
e. True.
18.
a. True.
b. True.
c. False. The pudendal artery supplies below levator ani.
d. False.
e. True. This is why cancer can spread to the spine.
19.
a. False. The renal artery supplies the kidney.
b. True.
c. False. The ovarian artery is a branch of the aorta.
d. True.
e. False. The inferior mesenteric artery supplies the rectum.
20.
a. True.
b. True. This is the pouch of Douglas.
c. True.
d. True.
e. True.
21.
a. True.
b. False. The anterior wall.
c. False.
d. False.
e. True.
22.
a. False. From inferior mesenteric.
b. False. To mesenteric nodes.
c. False. Columnar.
d. False. Visceral.
e. False. Portal.
23.
a. True.
b. True.
c. True. Contraction of this means that catheterisation is difficult at this point.
d. False. Corpus spongiosum.
e. True.
24.
a. False.
b. False. External (sphincter urethrae).
c. False. That is formed by levator ani (pelvic diaphragm).
d. False.
e. False.
25.
a. True.
b. True.
c. True.
d. False. To para-aortic nodes.
e. False. To internal iliac nodes, and elsewhere.
26.
a. False. The spleen is related to ribs 9, 10 and 11, but not 8.
b. True. The lateral cutaneous nerve of the thigh L2, 3 may be damaged.
d. True. The perineal body is an integral part of the pelvic diaphragm and associated voluntary anal and urethral sphincters.
e. True. The sacral spinal cord is at the level of these vertebrae. S2, 3, 4 segments give rise to nerve impulses for, amongst other things, penile erection.
27.
a. True.
b. True.
c. True.
d. False. This is much higher. The oesophageal hiatus in the diaphragm is at vertebral level T10, so the cardio-oesophageal junction would be about T10/T11.
e. True.
28.
a. True.
b. True.
c. True.
d. True.
e. True.
29.
a. False. It is irrelevant.
b. True.
c. False.
d. True. It appears to be related to the ischial spines on a PA radiograph.
e. True.
30.
a. False. This is anterior.
b. False. This is anterior.
c. False. This is superomedial.
d. True. This is important in renal biopsy procedures.
e. True.
Single best answers
31. c.
32. d.
33. a.
34. d.
35. b.
36. b.
37. b.
38. b.
39. d.
40. d.
41. d.
42. b.
Matching item answers
43. e.
44. g.
45. f.
46. a.
47. h.
48. a. It may also extend into the epigastrium.
49. b.
50. h.
51. e.
52. c. If hugely enlarged, the spleen may be palpable much lower and to the right, even in the right iliac fossa.
53. i.
54. b.
55. h.
56. a.
57. c.
58. a.
59. d.
60. d. The level of the iliac crests is useful as a landmark in lumbar puncture.
61. b.
62. d.
63. a.
64. a.
65. b.
66. b.
67. e.
68. e.
69. a.
70. a.
71. c.
72. a.
73. c.
74. b.
75. c. Same as 71.
76. b.
77. a.
78. e.
79. c.
80. a.
81. a.
82. b.
83. b.
84. b.
85. e.
86. b.
87. e.
88. c.
89. c.
90. d.
Short answers
92. See 11.2 (p. 111). In the scrotum the testis is covered by tunica albuginea and the two layers, visceral and parietal, of the tunica vaginalis (equivalent to peritoneum). Vessels and nerves pass between testis and scrotum through the spermatic cord, which also includes the cremaster muscle. Contraction of this muscle, such as in the cremasteric reflex elicited, for example, by cold hands, causes testicular retraction. A hydrocele is a collection of serous fluid between the visceral and parietal layers of the tunica vaginalis. A word on the embryology would be nice, but not necessary.
93. If blood can not flow through liver sinusoids (e.g. in disease) it will find bypass channels, or portosystemic anastomoses. Veins at the lower end of the oesophagus are important, as also are those resulting from reopening of channels in the falciform ligament (ligamentum teres, umbilical vein) taking blood to the anterior abdominal wall. Veins of the anterior abdominal wall radiate from the umbilicus giving the appearance of Medusa’s head. Other connections of clinical significance are in the posterior abdominal wall. Artificial bypass could be provided by connecting the portal vein to the inferior vena cava, but this would mean substances absorbed from the gut tube did not pass through the liver and were not detoxified.
94. Although the liver and diaphragm are attached to each other at the bare area, recesses of the peritoneal cavity extend between them for some distance – the anterior and posterior subphrenic spaces. The right posterior space communicates with the greater sac at the hepatorenal (Morison’s) pouch, between liver and kidney on the right, which also communicates with the lesser sac through the foramen of Winslow, and the right paracolic gutter. This matters because fluid can collect in these spaces and be the cause of disease that is difficult to diagnose.
95. The vagus nerve enters the abdomen with the oesophagus through the diaphragm at vertebral level T10. It travels down the lesser curvature in the lesser omentum. Branches pass to the stomach, antrum (nerves of Latarjet) and liver. Vagotomy (e.g. for reducing acid secretion) means that the pyloric sphincter does not function properly and a connection may have to be made between the stomach and jejunum (gastrojejunostomy). Vagotomy is now infrequently performed since the advent of suitable drugs (e.g. proton pump inhibitors) for hyperacidity and ulcer treatment.
96. The uterus is supported by levator ani (pelvic diaphragm) and ligaments on its superior surface (pubocervical, sacrocervical, cardinal). These suspend the uterus in a sling and help maintain anteversion (uterus bent forwards on vagina), along with the broad ligament. Since levator ani is anchored centrally at the perineal body, damage to this will weaken the uterine supports. This may be caused by direct trauma, or wear and tear (e.g. repeated childbirth).
97. The rectouterine pouch = pouch of Douglas. It is full of coils of small intestine and is intimately related to the posterior vaginal fornix, through which an abscess may be drained in the female. In the male, one would have to go through the anterior rectal wall. Back-street abortionists pushed implements straight up the vagina, not knowing about the angle of anteversion, with dire consequences.
98. Rugby is a very dangerous game. The player has been kicked in the renal angle, with resultant kidney damage. Internal bleeding into the pelvis and ureter explains blood in the urine. Fractured ribs cause right pneumothorax with breathing difficulties, and have ruptured the spleen to give massive internal bleeding. All this could be fatal.
99. Puborectalis maintains the angle between the rectal ampulla and anal canal. It is intimately connected with the deep part of the external (voluntary) anal sphincter and so together they are vital in the maintenance of faecal continence.
100. Prostate cancer (like any pelvic cancer) can spread by valveless veins of Batson to the internal vertebral venous plexus and lead to secondary deposits in vertebral bodies. This may cause back pain and lead to collapse of vertebrae, trapping lumbar nerve roots and giving shooting pains, and/or numbness, in the lower limb(s).