52 A Case Study Approach to the Role of Spinal Deformity Correction in the Aging Spine
KEY POINTS
Introduction
Adult degenerative deformity usually presents as a mild curve, which is rarely greater than 30 degrees unless it is superimposed on an adolescent-onset curve. Symptomatic lumbar curves tend to be larger in the idiopathic group than in the degenerative group.1 Degenerative disc disease and osteoporosis are major contributing factors in adult-onset deformity. In these adult deformities, vertebral structural changes with lateral olisthesis are typically associated with degenerative disc and facet joint arthrosis. Adult deformity may also present as a sequela after a decompression for spinal stenosis or spinal fusion for degenerative disc disease. In primary as well as secondary deformities, the degenerative process plays a central role and leads to loss of lumbar lordosis, not infrequently progressing to thoracolumbar kyphosis.
Natural History
Idiopathic Curves
Untreated adolescent idiopathic curves are known to progress after skeletal maturity 2–4. On long-term follow-up of patients with adolescent scoliosis at the University of Iowa, Weinstein et al reported that 68% of the curves progressed after maturity. Thoracic curves progressed at 1 degree per year, thoracolumbar at 0.5 degree per year. Factors associated with curve progression were Cobb angle greater than 30 degrees, apical vertebral rotation more than 30%, presence of lateral olisthesis, and a poorly seated L5 vertebra over S1 in lumbar curves 4.
Degenerative Curves
Pritchett and Bortell reported on the natural history of degenerative scoliosis in 200 patients. The number of vertebrae involved in the curve were from 3 to 6 (mean 3), with the apex commonly located between L2 and L3, and with 68% of the curves being left-sided. While degenerative spondylolisthesis was noted in half the patients, lateral listhesis was even more common (78%). They found that all the curves with the intercrestal line passing through L5 or the L4-5 interspace with vertebral rotation of 2 or more on the Nash and Moe scale progressed, as did curves greater than 30 degrees with lateral listhesis of 6 mm or more 5.
Korovessis et al. followed up 91 adults with de novo spinal deformity for a period of 3.7 years. The average curve size was 16.5 degrees (range 10° to 36°). Risk factors for progression were lateral olisthesis, a high Harrington factor (the Cobb angle divided by the number of vertebrae involved in the curve), and the disc index 6. In a similar study, Perennou et al. also reported a curve progression of 10 degrees or more in 73% of their patients over a follow-up period of 10 to 30 years, at an average of 3 degrees per year 7.
Imaging Evaluation
Radiographic studies for diagnosis and evaluation of adult scoliosis include full-length standing radiographs, bending films, hyperextension films, CT myelograms, and MRI. Assessment of bone mineral density will provide information regarding the presence and severity of osteporosis.
Standing radiographs with hips and knees in extension are necessary to evaluate the extent of the deformity and to assess sagittal and coronal balance. Supine side-bending radiographs may not be useful in degenerative scoliosis, but are useful in idiopathic scoliosis to assess curve rigidity and flexibility. Other options include traction views and fulcrum-bending views.8 Curve location, curve magnitude, number of levels involved, curve direction, and rotation should be evaluated on the radiographs. The presence of anterolisthesis, the maximum lateral olisthesis, the height of the residual disc spaces, and the presence of osteoporotic compression fractures are the radiographic factors that impact curve progression.
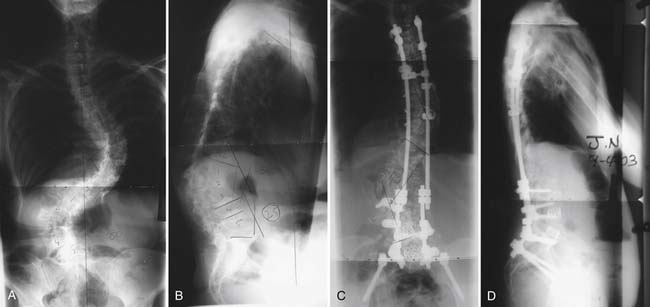
Achievement of coronal and sagittal balance is more important in adults than correction of deformity. Coronal balance is defined by the distance of the C7 plumb line from the central sacral vertical line (CSVL) on standing radiographs. Lateral trunk shift (LTS) measurement is also useful in thoracolumbar curves and is defined as the distance between the midpoint of the horizontal line drawn to the edges of the ribs at the apex of the deformity and the CSVL. (Figure 52-2)
The Role of Conservative Management
A commonly described prerequisite to surgical intervention is the lack of response to conservative care. Even though multiple nonsurgical options are advocated for adult scoliosis, there is currently a lack of evidence in the literature regarding the efficacy of these treatment options. Everett et al reviewed the literature on nonsurgical treatment options for adult scoliosis. They concluded that in the conservative treatment of adult deformity, there is level IV evidence for the role of physical therapy, bracing, and chiropractic care, while there is level III evidence for injections .9
Indications for Surgery
The second category is that of patients over the age of 50, who present mostly with degenerative curves or with idiopathic curves worsened by superimposed degenerative changes. In these patients, surgery is most likely to be indicated for progressive deformities with sagittal or coronal plane imbalance, or for refractory back or radicular pain with or without symptoms of spinal stenosis. Although compromised pulmonary function has also been suggested as an indication, Korvessis et al did not find any difference in pulmonary function in adult scoliosis patients compared with age-related changes in normal persons at an average of 23 years follow-up.6
Surgical Planning
A multitude of factors impact surgical decision-making in this patient population. Achievement of coronal and sagittal balance is the most important goal for many patients. A balanced spine orients the skull so that it is placed over the pelvis. This reduces paraspinal muscle fatigue and pain, improves patient satisfaction, improves cosmesis, and reduces the risk of complications associated with persistent decompensation in the sagittal or coronal plane. A well-balanced spine in the sagittal plane has been found to correlate with a better self-image score in adult deformity patients.10 While extensive surgery might be required to achieve an adequately decompressed and well-balanced spine, the individual surgical plan needs to be matched with the overall health, medical fitness, and expectations from surgery for every patient. Medical and social factors that are known to correlate with poor outcome are nutritional deficiency,11 chronic respiratory conditions,12 diabetes,13 smoking,14,15 coronary or cerebrovascular artery disease, and osteoporosis.16 Osteopenia is a major concern, especially if significant deformity correction is one of the goals. Segmental fixation can create a large surface area for force transmission and possibly prevent fixation failure. Medical treatment of osteoporosis with daily subcutaneous injections of parathyroid hormone for 2 to 6 weeks has been shown to enhance spinal fusion, in animal models.17,18
If an anterior and posterior fusion is planned, a same-day procedure is preferable to a staged procedure, as nutritional status has been found to take 6 to 12 weeks to return to the baseline after posterior surgery.19 Use of parenteral nutrition has been advocated if a staged procedure is planned, to improve the nutritional status before the second stage.20
The Role of Decompression Only in Adult Scoliosis Surgery
In carefully selected patients with degenerative scoliosis, performing a decompression alone without an instrumented fusion may be an option. If the patient presents with symptoms of neurogenic claudication and minimal back pain, it is possible that the patient will get relief with a trial of epidural steroids. If such patients have collapsed disc spaces without any evidence of anterolisthesis or lateral listhesis, they can be treated with decompression alone or decompression with an in situ fusion without instrumentation. Frazier et al. assessed the relationship between preoperative scoliosis and clinical outcome after a decompression only procedure for spinal stenosis in 90 patients with degenerative scoliosis. They inferred that the presence of preoperative scoliosis was associated with less improvement in back pain in these patients postoperatively; however, there was no correlation between preoperative scoliosis and satisfaction or improvement in leg pain and walking capacity after a decompression-only procedure 21.
The Role of Deformity in the Clinical Presentation
Early studies indicated that the incidence of back pain in adult scoliosis patients is about the same as in age-matched controls. Kostuik found a 60% incidence of back pain in adult patients with scoliosis, which was similar to that noted in patients without spinal deformity22. In other studies, patients with adult scoliosis were found to have more severe back pain as compared to controls, especially if the curve progressed beyond 45 degrees23. In more recent studies, Weinstein et al. have reported that chronic back pain was present in 61% of the scoliotic patients as compared to 35% of the controls24. Schwab et al. found a highly significant correlation between the severity of pain in adult scoliosis patients and the presence of lateral olisthesis and obliquity of L3 and L4 endplates on plain radiographs1. Jackson et al. had found the fractional lumbosacral curves most disabling and painful. They reported that while scoliosis greater than 40 degrees and kyphosis greater than 50 degrees correlated with pain, rotational deformity had the highest correlation with pain25. More recently, Buttermann et al. analyzed the correlation between degenerative disc findings on MRI with pain in scoliosis patients. In adult scoliosis patients, they found that the pain typically corresponded to the apex of the curve or to the lumbosacral junction. They found a higher incidence of disc degeneration and inflammatory end plate changes in adult scoliotics than asymptomatic controls. When compared with symptomatic patients with disc degeneration without a deformity, adults with scoliosis had a higher incidence of disc degeneration and inflammatory end plate changes at proximal lumbar levels (T12 – L3)26.
The role of osteoporosis in the causation of adult deformity is well known. Osteoporotic fractures may cause pain, in addition to their contribution to the deformity. Radicular pain in the lower extremities is caused by degenerative changes in adult scoliosis. Root entrapment is more common in the concavity of the curve 7,25. In 200 patients with adult scoliosis, Pritchett et al. had found a 72% incidence of neurogenic claudication and a 45% incidence of neurological symptoms in the lower limbs, most commonly paresthesias 5.
Spinal balance in sagittal and coronal plane can be adversely affected in adult scoliosis. Poor spinal balance is known to worsen the functional status in these patients, and can be quite disabling. Pain in adult scoliosis may arise from muscle fatigue due to abnormal biomechanics caused by the deformed and poorly balanced spine. Glassman et al studied the impact of spinal balance on clinical symptoms in 298 adult scoliosis patients with or without prior surgery. They reported that positive sagittal balance led to greater pain, poor function, and poor self image in patients with or without prior surgery while coronal balance of more than 4 cm correlated with greater pain and poor function. Additionally, the severity of symptoms was found to increase linearly with worsening sagittal imbalance. In terms of location, thoracic curves were better tolerated than thoracolumbar or lumbar curves; however, the magnitude of the curve had a poor correlation with functional status 27,28. In patients with adult degenerative lumbar or thoracolumbar scoliosis, Ploumis et al. reported that coronal imbalance more than 5 cm affected bodily function and moderate to severe lateral olisthesis (more than 6 mm) correlated with higher bodily pain, while sagittal balance did not show a good correlation with functional results 29. In another study, positive sagittal balance (C7 plumbline more than 6 cm) in patients with adult scoliosis has been correlated with worse Oswestry Disability Index scores (ODI), while there was no correlation found between ODI and coronal imbalance. However none of the patients in this study had coronal imbalance worse than 4 cm.30. Loss of lumbar lordosis and thoracolumbar kyphosis have also been found to have a positive correlation with self-reported pain scores in adult scoliosis patients1.
In addition to pain and spinal balance abnormalities, adult deformity can lead to significant body image and cosmesis issues. Deformity has been known to promote a negative body image, which can lead to difficulties in physical functioning and social interaction. Body image is known to be a significant issue with scoliosis patients31,32 Psychosocial studies in adult scoliosis patients have reveled difficulties in social and intimate relationships due to physical difficulties in participation, fear of injury, or self-consciousness33–35 . Attempts have been made to correlate radiographic deformity parameters with health-related quality of life (HRQL) and body image score in adult deformity patients. Except for the sagittal profile, other radiographic measures are found to correlate poorly with HRQL and body image scores in adults1,27,33. Walter Reed Visual Assessment Score (WRVAS) is a visual scale for patients’ assessment of deformity. It has been suggested that, in adults, the WRVAS is a more accurate reflection of the impact of scoliosis deformity on patient body image and HRQL than radiographic indicators. Tones et al. reported that the items of the WRVAS shared a consistent negative correlation with the Physical Functioning, Vitality, and General Health subscales of the SF-36v2, and the Physical Component Summary score in adult scoliosis patients. They also reported that older participants perceived their deformities as more severe than younger participants 26,36.
The importance of these issues from the patients’ perspective is exemplified by postoperative outcome studies in patients who have surgical correction of the deformity. Bridwell et al. had used SRS 22, ODI and SF-12 to assess outcome after surgery in 56 adult scoliosis patients at 1- and 2-year follow-up. They concluded based on these scores that surgical treatment significantly improved pain, self image, and function. They found that the greatest responsiveness to the change after surgery was demonstrated by self image domain, then the SRS total score and pain scores.37.
Surgical Techniques
Posterior Instrumentation
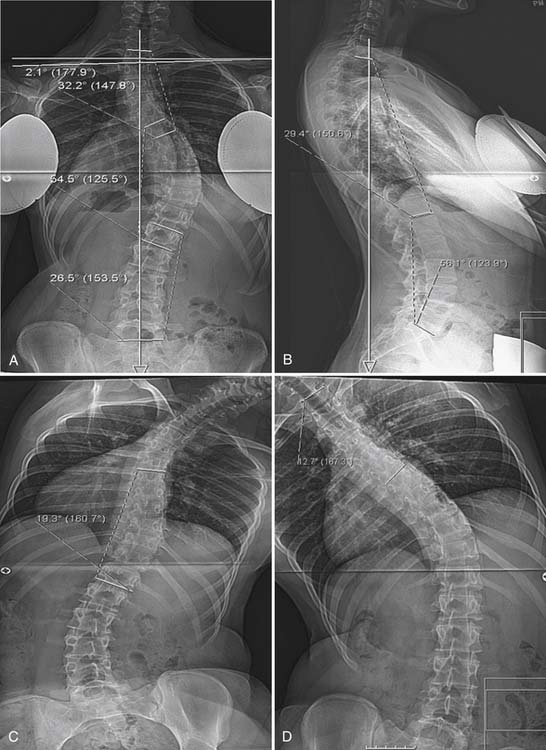
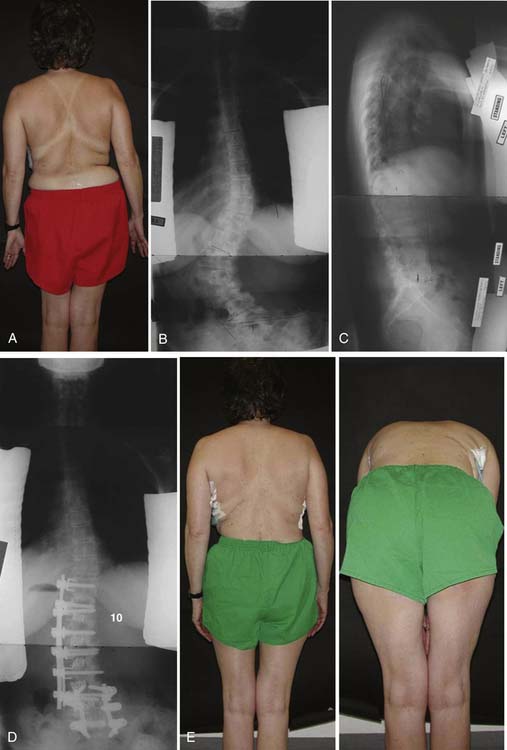
Posterior fusion and instrumentation is the most common method used in adult deformity correction. Most surgeons are familiar with the approach and comfortable with the procedure. It allows decompression of the stenotic levels and correction of deformity in all three planes. Usually, segmental instrumentation using pedicle screws and hooks or all screws is preferred, as this creates a large area of force transmission during correction of the deformity38. Traditionally sublaminar wires, hooks, and pedicle screws have been used for deformity correction and segmental fixation either individually or in different combinations. All–pedicle-screw constructs are becoming more popular for deformity correction. Although some studies have found that sublaminar wires with hooks provide similar or sometimes better coronal plane correction, 39,40 multiple studies have found that pedicle screw constructs offer better correction, better long-term durability of correction, better rotational correction, improved pulmonary function values, and lesser blood loss than hybrid constructs39,41,42. Additionally, pedicle screws provide three column fixation, have better pullout strength, 43 and improve the ability to maintain and enhance lumbar lordosis.44 Pedicle screw constructs are, however, significantly costlier 42. (Figure 52-3)
Anterior Release or Anterior-Only Surgery
Many studies have documented that anterior release is not necessary in most patients with adolescent idiopathic scoliosis even if the curves are larger than 70 degrees, especially when adequate posterior release is performed and posterior instrumentation using an all–pedicle-screw construct is utilized.45–47 However, adult scoliosis is a pathologically different entity. Due to superimposition of the degenerative process, curves are more rigid, and the presence of rotatory olisthesis at multiple levels compounds the coronal plane deformity. Additionally, the presence of thoracolumbar kyphosis may make it difficult to achieve sagittal and coronal balance with a posterior-only procedure. So, traditionally, an anterior spinal release has been proposed for the treatment of adult lumbar spinal deformities,48–51 which is to be followed by posterior instrumentation and fusion.
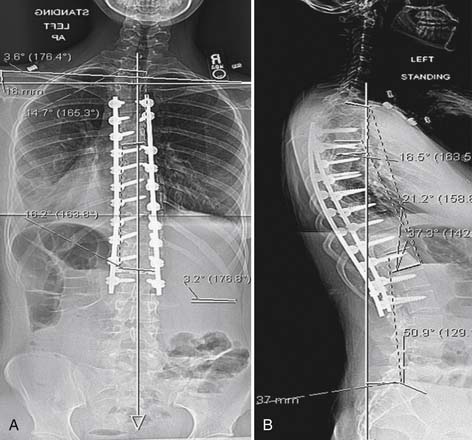
Anterior release would aid deformity correction by release of the anterior longitudinal ligament and an adequate diskectomy. Also, the addition of interbody structural grafts after diskectomy could improve the sagittal alignment. The addition of anterior release could also provide a 360° fusion. These benefits come at the cost of an additional thoracolumbar procedure or a retroperitoneal procedure, which has its own set of complications in this patient population, as has been reported recently.52 This has led to questioning the necessity of anterior release in all patients with adult scoliosis and the suitability of using a posterior-only procedure in well-selected cases based on flexibility of the curves and sagittal balance. With successful reports of use of posterior-only procedures in larger curves in adolescents, there are also reports of the use of segmental third-generation instrumentation to correct adult deformities in posterior-only procedures. Earlier reports indicate use of posterior-only procedure in flexible adult curves.53 More recently, Kim et al reported a retrospective, comparative study of radiographic and functional outcomes with and without an anterior apical release of the lumbar curve in adult scoliosis patients. On comparing the two groups, it was found that the surgeons chose to do an anterior procedure in curves with larger Cobb angles and less flexibility. At follow-up, there was no significant difference in the two groups in terms of correction achieved, lumbar lordosis, thoracic kyphosis, coronal balance, and sagittal balance. The clinical outcome as measured by SRS-22 scores was better in the posterior-only group.54 Use of minimally invasive techniques like extreme lateral interbody fusion55 may reduce the morbidity of a multilevel anterior procedure and may increase the acceptability of an anterior procedure in this patient population. Even though this procedure has been performed in some institutes for anterior diskectomy fusion in adult scoliosis, as yet there are no reports in the literature (Figure 52-4).
Another option in these patients with flexible double major or thoracolumbar curves can be a hybrid fusion where partially overlapping anterior and posterior instrumentation is used. This has been tried in our institute in recent years. In this procedure, anterior instrumentation is placed in the form of vertebral body screws with either one or two rods extending from the lower thoracic spine to either the L3 or L4 level. Anterior diskectomy is performed and structural grafts or cages are used in the lumbar region. Following this, the thoracolumbar portion of the curve is corrected using a rod rotation maneuver while at the same time putting the rod into lordosis. The anterior procedure is completed by segmental compression, going away from the apex proximally and distally. The posterior procedure involves only a posterior fusion extending from either L3 or L4 to S1, so as to overlap the levels of the anterior fusion. This instrumentation design may spare the proximal spinal fusion levels and does not require instrumentation or fusion to the pelvis. In an initial cohort of 10 patients, it has been shown to provide similar correction with similar complication rates to a posterior-only or a traditional anterior and posterior procedure.56
Extent of Fusion
In case of lumbar or thoracolumbar curves, the ideal construct length remains unclear. However, there are a few well-recognized rules. It is useful preoperatively to identify which segments contribute to the patient’s pain. The apex of the deformity with any areas of lateral listhesis should be included. There is no general consensus about where the construct should end rostrally. Usually, the upper instrumented vertebra should be a stable one. The construct should not terminate at the apex of a kyphosis or apex of a curve in the coronal plane. Some earlier studies had recommended avoiding L1 or L2 as proximal fusion levels and considering extension to the thoracic spine, to avoid termination of fusion at the thoracolumbar junction with possible junctional failure.57,58 However, more recently, Kim et al. reported a retrospective study comparing the prevalence of revision surgeries and proximal junctional change after instrumented fusion from T9, T11, or L1 to L5 or S1. They reported a significantly high incidence of proximal junctional kyphosis; however, there was no significant difference in the proximal junctional angulation or revision rates in the three groups based on the proximal extent of fusion.59 They opined that a more distal proximal fusion level at a neutral and stable vertebra, regardless of whether the construct ends at the distal thoracic spine or proximal lumbar spine should be used as the radiographic outcome, and revision rates are similar.
It has been suggested before that in selected cases of lumbar degenerative scoliosis, fusion can be performed within the scoliotic curve restricted to the levels that are decompressed instead of fusing to the end vertebrae proximally. Kyu et al reported that such short fusion within the curve might be sufficient for curves with a smaller Cobb angle and good spinal balance. They reported a significantly lower value for average Cobb correction and average correction of coronal imbalance and a higher incidence of proximal junctional failure in the patients with short fusion. The rate of early complications and distal junctional failure was higher in patients with longer fusions. They reported that the clinical outcome as measured by improvement in the ODI was similar between the two groups.60
Extension of Fusion to the Sacrum
The distal extent of fusion in adult deformity is most commonly near the lumbosacral junction. The surgeon needs to answer the question of whether the need for fusion to sacrum is worth the risk of complications that have been found to be associated with ending a long fusion at S1. The current literature does not provide any definitive answers. It is generally recommended that fusion to S1 should be considered when there is significant degeneration at L5-S1, obliquity of the L5-S1 disc (greater than 15°), stenosis at L5-S1 requiring decompression, previous decompression at L5-S1, and spondylolisthesis at L5-S1.61 However, long fusions to the sacrum may require longer time, involve more blood loss, and have been found more likely to develop complications and require more additional surgical procedures.62,63 Especially, the risk of pseudarthrosis at L5-S1 in long fusions has been reported to be as high as 24%.64,65 Kim et al. reported that factors that increased the risk of pseudarthrosis at L5-S1 were thoracolumbar kyphosis (T10-L2 > 20° vs. < 20°), osteoarthritis of hip joints, thoracoabdominal approach, positive sagittal balance greater than or equal to 5 cm postoperatively, age at surgery older than 55 years, and incomplete sacropelvic fixation.64 Additionally, there is a small but real risk of development of sacral insufficiency fractures after long fusions to the sacrum.66
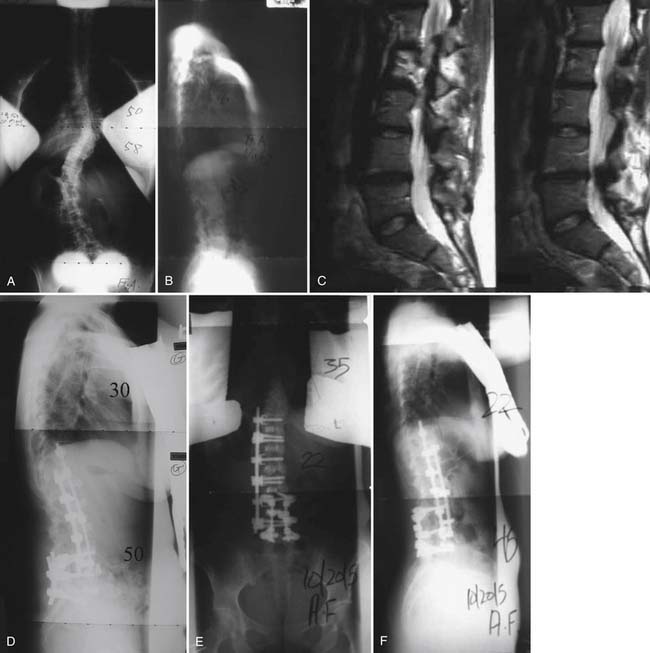
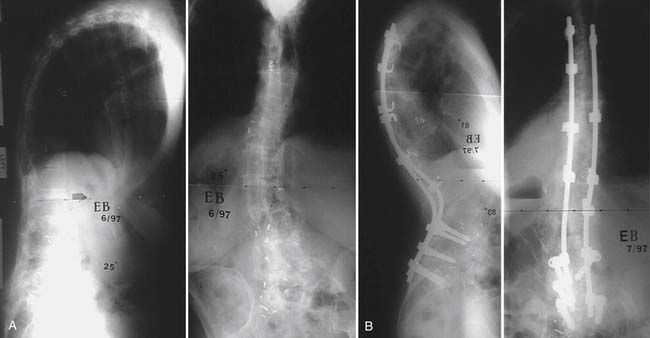
Recently, there have been reports comparing the complications and outcome in adult deformity patients with fusion to L5 to those with fusion to S1. Edwards et al compared complications, radiographic parameters, and functional outcomes in matched cohorts of patients with adult deformity that underwent long fusions from the thoracic spine to either L5 or the sacrum at a minimum 2-year follow-up. They found that the correction of sagittal imbalance was superior for patients fused to the sacrum (C7 plumb line: L5 0.9 cm, sacrum 3.2 cm, P = 0.03), and, on follow-up, they tend to maintain sagittal balance better than those with fusion to L5. At latest follow-up, 67% of patients with fusion to L5 had radiographic evidence of advanced L5-S1 disc degeneration, which may explain the worsening of sagittal balance in these patients. The sacrum cohort, however, required more surgical procedures and experienced a greater frequency of major complications (L5 22%, sacrum 75%, P = 0.02), including nonunion (L5 4%, sacrum 42%, P = 0.006) and medical morbidity (L5 0%, sacrum 33%, P = 0.001). SRS-24 scores reflected a similar patient assessment of outcome and function for the two cohorts.67 Cho et al compared the results of fusion to L5 to those for fusion to the sacrum in patients with adult degenerative scoliosis. They found that the duration of surgery and blood loss was not significantly different in the two groups. The correction of lumbar lordosis was better in patients fused to the sacrum; however, the ultimate change in sagittal and coronal balance was similar in both groups. On follow-up, 58% of the patients with fusion to L5 developed advanced disc degeneration at L5-S1. They found that patients with preoperative sagittal imbalance (C7 plumb line greater than 5 cm) and lumbar hypolordosis (lordosis less than 30°) are more likely to develop symptomatic L5-S1 disc degeneration when fusion to L5 is performed. 68 Kuhns et al specifically evaluated the fate of the L5-S1 disc at a minimum follow-up of 5 years in patients with long deformity fusions to L5. They found that advanced disc degeneration developed in 69% of the patients who had healthy L5-S1 discs before surgery, with 23% requiring extension of fusion to the sacrum later, while a further 19% had indications for extension of fusion to the sacrum but either had comorbidities precluding surgery or declined further surgery. They reported that the risk factors of development of advanced disc degeneration at L5-S1 were long fusion extending to the upper thoracic spine and having a circumferential lumbar fusion 69 (Figures 52-5, 52-6).
The Role of Osteotomies and Spinal Column Shortening in Adult Deformity Patients
Osteotomies are required to achieve sagittal and coronal balance in severe adult deformities when the flexibility of the deformity would not allow acceptable correction with instrumentation alone. More commonly, osteotomies are used to correct sagittal imbalance. The osteotomies utilized commonly are the Smith-Peterson osteotomy (SPO) and the pedicle subtraction osteotomy (PSO). Smith-Peterson described the osteotomy in which a chevron-shaped wedge of bone is removed from the posterior elements.70 Correction is achieved by closing this wedge and opening the disc space anteriorly. The axis of rotation is located at the posterior disc space. Sagittal correction up to 15 degrees per level can be achieved with SPO. However, the lengthening of the anterior column is associated with the risk of vascular and neurologic complications.71–73 Also, it may create an anterior bony defect that may make arthrodesis difficult.
PSO is a V-shaped wedge resection of the vertebral body along with the pedicles and posterior elements. It was described by Thomasen for treating kyphotic deformities in ankylosing spondylitis.74 This osteotomy hinges about an axis at the anterior vertebral body. It enables shortening of the vertebral column posteriorly and causes no lengthening anteriorly, reducing the risk of vascular injuries. It provides a more stable correction, as closure of the osteotomy closes the gap posteriorly. This osteotomy can achieve an average correction of 30 to 40 degrees at a single segment and is useful for correcting high-grade fixed sagittal deformities.75–77 Kim et al reported on the outcome of 35 consecutive patients who underwent pedicle subtraction osteotomies at a minimum 5-year follow-up. They reported 76% improvement in self-image scores, 66% improvement in pain scores, and 69% improvement in function scores at ultimate follow-up. Patients who maintained a sagittal vertical axis of less than 8 cm continued to have good SRS scores, while those with a sagittal vertical axis greater than or equal to 8 cm had worsening of self-image and function scores.78 Cho et al compared the clinical and radiographic outcome in patients who underwent SPO to those who underwent a PSO. They reported that the mean correction of the kyphotic angle at the osteotomy site after an SPO was 10.7 degrees. They compared the radiographic outcome after three or more SPOs to that after a single-level PSO to evaluate whether they were comparable. They found that even though the average correction in both groups was close to 30 degrees, the improvement in sagittal balance was, statistically, significantly less with three or more SPOs (5.5 ± 4.5 cm) than with a single-level PSO (11.2 ± 7.2 cm). Also, patients with multiple SPOs showed significantly more decompensation toward concavity. The mean estimated blood loss was significantly higher in patients with a PSO than with multiple SPOs.79 Rose et al analyzed the role of pelvic incidence (PI) and thoracic kyphosis (TK) in predicting the ideal lumbar lordosis (LL) required to achieve sagittal balance in patients undergoing a PSO. They found that the formula PI + LL + TK ≤ 45° showed 91% sensitivity in predicting ideal sagittal balance. They also reported that patients with fusion to the upper thoracic spine after a PSO preserved correction better than those with fusion to the thoracolumbar region.80 (Figure 52-7).
Summary
Patients with adult scoliosis more commonly present with pain and worsening balance as major issues, unlike adolescent scoliosis patients who present with cosmesis as the major concern. Conservative treatment has not been shown to be of any reliable long-term benefit in adult patients with symptomatic scoliosis. There are multiple surgical options for these patients; however, surgical planning should be customized to the patient based on clinical presentation, sagittal and coronal profile, curve flexibility, and medical comorbidities. Requirement for anterior release, extent of fusion proximally, inclusion of the sacrum in the construct, and the requirement for osteotomies are some of the major questions that need to be answered during surgical planning. Based on the current literature, restoration of sagittal and coronal balance is the most important factor for predicting a good surgical outcome in these patients.
1. Schwab F.J., Smith V.A., Biserni M., Gamez L., Farcy J.P., Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002;27(4):387-392.
2. Chuah S.L., Kareem B.A., Selvakumar K., Oh K.S., Borhan Tan A., Harwant S. The natural history of scoliosis: curve progression of untreated curves of different aetiology, with early (mean 2 year) follow up in surgically treated curves. Med. J. Malaysia. 2001;56(Suppl C):37-40.
3. Ascani E., Bartolozzi P., Logroscino C.A., et al. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine. 1986;11(8):784-789.
4. Weinstein S.L., Ponseti I.V. Curve progression in idiopathic scoliosis. J. Bone Joint Surg. Am.. 1983;65(4):447-455.
5. Pritchett J.W., Bortel D.T. Degenerative symptomatic lumbar scoliosis. Spine. 1993;18(6):700-703.
6. Korovessis P., Piperos G., Sidiropoulos P., Dimas A. Adult idiopathic lumbar scoliosis. A formula for prediction of progression and review of the literature,. Spine. 1994;19(17):1926-1932.
7. Perennou D., Marcelli C., Herisson C., Simon L. Adult lumbar scoliosis. Epidemiologic aspects in a low-back pain population. Spine. 1994;19(2):123-128.
8. Luk K.D., Cheung K.M., Lu D.S., Leong J.C. Assessment of scoliosis correction in relation to flexibility using the fulcrum bending correction index. Spine. 1998;23(21):2303-2307.
9. Everett C.R., Patel R.K. A systematic literature review of nonsurgical treatment in adult scoliosis,. Spine. 2007;32(Suppl. 19):S130-S134.
10. Kim Y., Bridwell K., Lenke L., Boachie-Adjei O., Marawar S. What radiographic sagittal parameters correlate with improved SRS self-image scores postoperatively in patients with sagittal imbalance? Analysis of 102 lumbar pedicle subtraction osteotomy patients. Spine J.. 2008;8(5), (Suppl. 1):29S-30S.
11. Klein J.D., Hey L.A., Yu C.S., et al. Perioperative nutrition and postoperative complications in patients undergoing spinal surgery. Spine. 1996;21(22):2676-2682.
12. Smetana G.W. Preoperative pulmonary evaluation [see comment]. N. Engl. J. Med.. 1999;340(12):937-944.
13. Moitra V.K., Meiler S.E. The diabetic surgical patient,. Curr. Opin. Anaesthesiol.. 2006;19(3):339-345.
14. Warner M.A., Offord K.P., Warner M.E., Lennon R.L., Conover M.A., Jansson-Schumacher U. Role of preoperative cessation of smoking and other factors in postoperative pulmonary complications: a blinded prospective study of coronary artery bypass patients. Mayo. Clin. Proc.. 1989;64(6):609-616.
15. Mok J.M., Cloyd J.M., Bradford D.S., Hu S.S., Deviren V.S., Jason A., Tay B.B., Sigurd H. Reoperation after primary fusion for adult spinal deformity: rate, reason, and timing. Spine. 2009;34(8):832-839.
16. Lin J.T., Lane J.M: Osteoporosis: a review, Clin Orthop, 425:2004, 126-134.
17. O’Loughlin P.F., Cunningham M.E., Bukata S.V., et al. Parathyroid hormone (1-34) augments spinal fusion, fusion mass volume, and fusion mass quality in a rabbit spinal fusion model. Spine. 2009;34(2):121-130.
18. Abe Y., Takahata M., Ito M., Irie K., Abumi K., Minami A. Enhancement of graft bone healing by intermittent administration of human parathyroid hormone (1-34) in a rat spinal arthrodesis model. Bone. 2007;41(5):775-785.
19. Lenke L.G., Bridwell K.H., Blanke K., Baldus C. Prospective analysis of nutritional status normalization after spinal reconstructive surgery. Spine. 1995;20(12):1359-1367.
20. Hu S.S., Fontaine F., Kelly B., Bradford D.S. Nutritional depletion in staged spinal reconstructive surgery. The effect of total parenteral nutrition,. Spine. 1998;23(12):1401-1405.
21. Frazier D.D., Lipson S.J., Fossel A.H., Katz J.N. Associations between spinal deformity and outcomes after decompression for spinal stenosis. Spine. 1997;22(17):2025-2029.
22. Kostuik J.P., Bentivoglio J. The incidence of low-back pain in adult scoliosis,. Spine. 1981;6(3):268-273.
23. Briard J.L., Jegou D., Cauchoix J. Adult lumbar scoliosis. Spine. 1979;4(6):526-532.
24. Weinstein S.L., Dolan L.A., Spratt K.F., Peterson K.K., Spoonamore M.J., Ponseti I.V. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289(5):559-567.
25. Jackson R.P., Simmons E.H., Stripinis D. Coronal and sagittal plane spinal deformities correlating with back pain and pulmonary function in adult idiopathic scoliosis. Spine. 1989;14(12):1391-1397.
26. Buttermann G.R., Mullin W.J. Pain and disability correlated with disc degeneration via magnetic resonance imaging in scoliosis patients. Eur. Spine J.. 2008;17(2):240-249.
27. Glassman S.D., Berven S., Bridwell K., Horton W., Dimar J.R. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine. 2005;30(6):682-688.
28. Glassman S.D., Bridwell K., Dimar J.R., Horton W., Berven S., Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine. 2005;30(18):2024-2029.
29. Ploumis A., Liu H., Mehbod A.A., Transfeldt E.E., Winter R.B. A correlation of radiographic and functional measurements in adult degenerative scoliosis. Spine. 2009;34(15):1581-1584.
30. Mac-Thiong J.T., Ensor E., Mehbod A.A., Perra J.H., et al. Can C7 plumbline and gravity line predict health related quality of life in adult scoliosis?[miscellaneous article]. Spine. 2009;34(15):E519-E527.
31. Rumsey N., Harcourt D. Body image and disfigurement: issues and interventions. Body Image. 2004;1:83-97.
32. Asher M.A., Burton D.C. Adolescent idiopathic scoliosis: natural history and long term treatment effects. Scoliosis. 2006;1(1):2.
33. Weinstein S.L., Dolan L.A., Spratt K.F., Peterson K.K., Spoonamore M.J., Ponseti I.V. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289(5):559-567.
34. Danielsson A.J., Nachemson A.L. Childbearing, curve progression, and sexual function in women 22 years after treatment for adolescent idiopathic scoliosis: a case-control study. Spine. 2001;26(13):1449-1456.
35. Danielsson A.J., Wiklund I., Pehrsson K., Nachemson A.L. Health-related quality of life in patients with adolescent idiopathic scoliosis: a matched follow-up at least 20 years after treatment with brace or surgery. Eur. Spine J.. 2001;10(4):278-288.
36. Tones M., Moss N. The impact of patient self assessment of deformity on HRQL in adults with scoliosis. Scoliosis. 2007;2:14.
37. Bridwell K.H., Berven S., Glassman S., et al. Is the SRS-22 instrument responsive to change in adult scoliosis patients having primary spinal deformity surgery? Spine. 2007;32(20):2220-2225.
38. Bradford D.S., Tay B.K., Hu S.S. Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine. 1999;24(24):2617-2629.
39. Karatoprak O., Unay K., Tezer M., Ozturk C., Aydogan M., Mirzanli C. Comparative analysis of pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery. Int. Orthop.. 2008;32(4):523-528.
40. Cheng I., Kim Y., Gupta M.C., et al. Apical sublaminar wires versus pedicle screws–which provides better results for surgical correction of adolescent idiopathic scoliosis? Spine. 2005;30(18):2104-2112.
41. Kim Y.J., Lenke L.G., Cho S.K., Bridwell K.H., Sides B., Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29(18):2040-2048.
42. Kim Y.J., Lenke L.G., Kim J., et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006;31(3):291-298.
43. Hitchon P.W., Brenton M.D., Black A.G., et al. In vitro biomechanical comparison of pedicle screws, sublaminar hooks, and sublaminar cables. J Neurosurg. 2003;99(Suppl. 1):104-109.
44. Smith J.A. Adult deformity:management of sagittal plane deformity in revision adult spine surgery. Curr. Opin. Orthop.. 2001;12(3):206-215.
45. Luhmann S.J., Lenke L.G., Kim Y.J., Bridwell K.H., Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine. 2005;30(18):2061-2067.
46. Burton D.C., Sama A.A., Asher M.A., et al. The treatment of large (>70 degrees) thoracic idiopathic scoliosis curves with posterior instrumentation and arthrodesis: when is anterior release indicated? Spine. 2005;30(17):1979-1984.
47. Arlet V., Jiang L., Ouellet J. Is there a need for anterior release for 70-90 degrees masculine thoracic curves in adolescent scoliosis? Eur. Spine J.. 2004;13(8):740-745.
48. Byrd J.A.3rd, Scoles P.V., Winter R.B., Bradford D.S., Lonstein J.E., Moe J.H. Adult idiopathic scoliosis treated by anterior and posterior spinal fusion. J. Bone Joint Surg. Am.. 1987;69(6):843-850.
49. Dick J., Boachie-Adjei O., Wilson M. One-stage versus two-stage anterior and posterior spinal reconstruction in adults. Comparison of outcomes including nutritional status, complications rates, hospital costs, and other factors. Spine. 1992;17(Suppl. 8):S310-6.
50. Swank S., Lonstein J.E., Moe J.H., Winter R.B., Bradford D.S. Surgical treatment of adult scoliosis. A review of two hundred and twenty-two cases,. J. Bone Joint Surg. Am.. 1981;63(2):268-287.
51. Shapiro G.S., Taira G.B., Boachie-Adjei O. Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical radiographic outcomes. Spine. 2003;28(4):358-363.
52. Kim Y.B., Lenke L.G., Kim Y.J., Kim Y.W., Blanke K., Stobbs G., Bridwell K.H. The morbidity of an anterior thoracolumbar approach: adult spinal deformity patients with greater than five-year follow-up,. Spine. 2009;34(8):822-826.
53. Ali R.M., Boachie-Adjei O., Rawlins B.A. Functional and radiographic outcomes after surgery for adult scoliosis using third-generation instrumentation techniques. Spine. 2003;28(11):1163-1169.
54. Kim Y.B., Lenke L.G., Kim Y.J., Kim Y.W., Bridwell K.H., Stobbs G. Surgical treatment of adult scoliosis: is anterior apical release and fusion necessary for the lumbar curve? Spine. 2008;33(10):1125-1132.
55. Ozgur B.M., Aryan H.E., Pimenta L., Taylor W.R. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J.. 2006;6(4):435-443.
56. Boachie-Adjei O., Charles G., Cunningham M.E. Partially overlapping limited anterior and posterior instrumentation for adult thoracolumbar and lumbar scoliosis: a description of novel spinal instrumentation, “the hybrid technique,”. HSS J. 2007;1:93-98.
57. Swank ML: Adjacent segment failure above lumbosacral fusions instrumented to L1 or L2.
58. Suk SI, Kim JH, Lee SM: Incidence of proximal adjacent failure in adult lumbar deformity correction.
59. Kim Y.J., Bridwell K.H., Lenke L.G., Rhim S., Kim Y.W. Is the T9, T11, or L1 the more reliable proximal level after adult lumbar or lumbosacral instrumented fusion to L5 or S1? Spine. 2007;32(24):2653-2661.
60. Cho K.J., Suk S.I., Park S.R., et al. Short fusion versus long fusion for degenerative lumbar scoliosis. Eur Spine J. 2008;17(5):650-656.
61. Bridwell K.H., Edwards C.C.2nd, Lenke L.G. The pros and cons to saving the L5-S1 motion segment in a long scoliosis fusion construct,. Spine. 2003;28(20):S234-42.
62. Schwab F.J., Lafage V., Farcy J.P., Bridwell K.H., Glassman S., Shainline M.R. Predicting outcome and complications in the surgical treatment of adult scoliosis. Spine. 2008;33(20):2243-2247.
63. Kostuik J.P., Hall B.B. Spinal fusions to the sacrum in adults with scoliosis. Spine. 1983;8(5):489-500.
64. Kim Y.J., Bridwell K.H., Lenke L.G., Rhim S., Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine. 2006;31(20):2329-2336.
65. Weistroffer J.K., Perra J.H., Lonstein J.E., et al. Complications in long fusions to the sacrum for adult scoliosis: minimum five-year analysis of fifty patients. Spine. 2008;33(13):1478-1483.
66. Vavken P., Krepler P. Sacral fractures after multi-segmental lumbosacral fusion: a series of four cases and systematic review of literature. Eur. Spine J.. 2008;17(Suppl. 2):S285-90.
67. Edwards C.C.2nd, Bridwell K.H., Patel A., Rinella A.S., Berra A., Lenke L.G. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine. 2004;29(18):1996-2005.
68. Cho K.J., Suk S.I., Park S.R., et al. Arthrodesis to L5 versus S1 in long instrumentation and fusion for degenerative lumbar scoliosis. Eur. Spine J.. 2009;18(4):531-537.
69. Kuhns C.A., Bridwell K.H., Lenke L.G., et al. Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5-S1 disc, minimum 5-year follow-up. Spine. 2007;32(24):2771-2776.
70. Smith-Petersen M.N., Larson C.B., Aufranc O.E. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J. Bone Joint Surg. Am.. 1945;27:1-11.
71. Adams J.C. Technique, dangers and safeguards in osteotomy of the spine. J Bone Joint Surg Br. 1952;34-B(2):226-232.
72. Weatherley C., Jaffray D., Terry A. Vascular complications associated with osteotomy in ankylosing spondylitis: a report of two cases. Spine. 1988;13(1):43-46.
73. Li F., Sagi H.C., Liu B., Yuan H.A. Comparative evaluation of single-level closing-wedge vertebral osteotomies for the correction of fixed kyphotic deformity of the lumbar spine: a cadaveric study. Spine. 2001;26(21):2385-2391.
74. Thomasen E: Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis, Clin. Orthop., 194:1985, 142-152.
75. Bridwell K.H., Lewis S.J., Lenke L.G., Baldus C., Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J. Bone Joint Surg. Am.. 2003;85-A(3):454-463.
76. Thiranont N., Netrawichien P. Transpedicular decancellation closed wedge vertebral osteotomy for treatment of fixed flexion deformity of spine in ankylosing spondylitis. Spine. 1993;18(16):2517-2522.
77. van Royen B.J., Slot G.H. Closing-wedge posterior osteotomy for ankylosing spondylitis. Partial corporectomy and transpedicular fixation in 22 cases. J. Bone Joint Surg. Br.. 1995;77(1):117-121.
78. Kim Y.J., Bridwell K.H., Lenke L.G., Cheh G., Baldus C. Results of lumbar pedicle subtraction osteotomies for fixed sagittal imbalance: a minimum 5-year follow-up study. Spine. 2007;32(20):2189-2197.
79. Cho K.J., Bridwell K.H., Lenke L.G., Berra A., Baldus C. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine. 2005;30(18):2030-2037.
80. Rose P.S., Bridwell K.H., Lenke L.G., et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine. 2009;34(8):785-791.