Pin Site Care: Cervical Tongs and Halo Pins
PREREQUISITE NURSING KNOWLEDGE
• The nurse needs to be knowledgeable about the anatomy and physiology of the spinal column, the special anatomy of the cervical vertebrae, the spinal cord, the cervical spinal nerves, and their areas of peripheral innervation. In addition, the nurse must understand the pathophysiology and manifestations of spinal cord injury, including the concepts of primary and secondary spinal cord injury and spinal shock.
• The nurse needs to be knowledgeable of the signs and symptoms of new spinal cord injury or extension of recent spinal cord injury, including impairment of motor and sensory function, respiratory function, and autonomic nervous system function that results in loss of vasomotor tone.
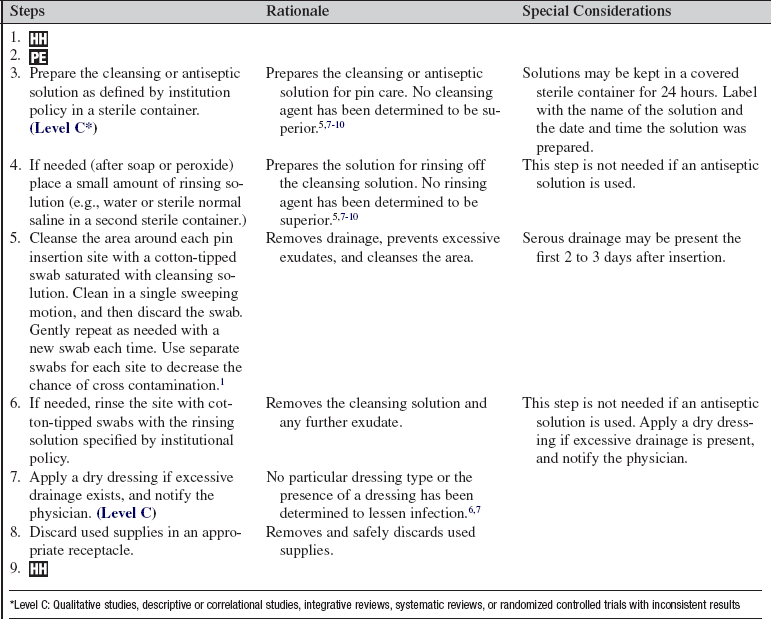
• The nurse needs to be knowledgeable of treatment options available to manage cervical injuries, including cervical spine traction with tongs or a halo ring. Tongs consist of a body with one pin attached at each end (see Fig. 97-2). Tong pins are applied to the outer table of the cranium on both sides of the skull.3 A halo ring device is also used for management of cervical injuries. This device is a graphite ring that is attached to the skull with four stabilizing pins (two anterior and two posterolateral; see Fig. 98-1). The pins are threaded through holes in the ring, screwed into the outer table of the skull, and locked into place. This device can be attached to traction or vest struts/posts.2
• Once inserted, the cervical device (tongs or halo ring) requires special care of the skin at the pin insertion sites (pin site care) to prevent and monitor for infection. Because the pins are inserted through the skin and into the bone, local infections can develop and proliferate and may result in cranial osteomyelitis. Loosening of the pins may also occur.3–6
• Various cleansing agents for pin site care have been used, including, but not limited to, 2% chlorehexidene solution, hydrogen peroxide, sterile normal saline solution, antibacterial soap and water, alcohol, and povidone-iodine. None have been found superior.5,7–10
• Generally, pin sites do not require a dressing unless excessive drainage occurs at the site.
• Pin sites should be inspected for infection, although the frequency of this inspection has not been clearly identified. Definitive guidelines for the frequency of pin site care, cleansing agents, removal of crust, and the application of dressings have not been established and depend on institutional policies.7,8
EQUIPMENT
• Approximately eight cotton-tipped applicators
• Cleansing or antiseptic solution
• Sterile container for cleansing solution
Additional equipment, to have available as needed, includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the procedure and the reason for pin care.  Rationale: Patient and family anxiety may be decreased.
Rationale: Patient and family anxiety may be decreased.
• Explain the patient’s role in assisting with the procedure.  Rationale: Explanation elicits patient cooperation and facilitates the procedure.
Rationale: Explanation elicits patient cooperation and facilitates the procedure.
• Teach the family if they will perform pin site care for the patient after discharge.  Rationale: Education elicits family cooperation and comfort in performing the procedure.
Rationale: Education elicits family cooperation and comfort in performing the procedure.
• Teach the family to notify the physician if the pins are loose. Teach the family not to adjust the pins.  Rationale: Safe and appropriate action is elicited.
Rationale: Safe and appropriate action is elicited.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s scalp for signs and symptoms of skin irritation; carefully inspect the pin sites for signs and symptoms of infection (e.g., redness, edema, or purulent drainage).  Rationale: Assessment identifies skin breakdown, irritation, or pin-site infection.
Rationale: Assessment identifies skin breakdown, irritation, or pin-site infection.
• Assess the patient’s pain and anxiety levels.  Rationale: Interventions may be needed before the procedure to promote patient comfort and decrease anxiety.
Rationale: Interventions may be needed before the procedure to promote patient comfort and decrease anxiety.
Patient Preparation
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Assist the patient to a supine position. The patient in a halo vest may be sitting up in a position of comfort.  Rationale: Access to the pins is facilitated for care.
Rationale: Access to the pins is facilitated for care.
References
1. Bell, A, Leader, M, Lloyd, H. Care of pin sites. Nurs Stand. 2008; 22:44–48.
2. Bono, CM. The halo fixator. J Am Acad Orthop Surg. 2007; 15:728–737.
3. Canale, ST, Beaty, JH. Campbell’s operative orthopaedics,. In: Canale ST, Beaty JH, eds. Cervical spine injuries. ed 11. Philadelphia: Mosby; 2008:1776–1777.
Hayes, VM, Silber, JS, Siddiqi, FN, et al. Complications of halo fixation of the cervical spine. Am J Orthop. 2005; 34:271–276.
5. Holmes, SB, Brown, SJ, Skeletal pin site care. National Association of Orthopaedic Nurses guidelines for orthopaedic nursing. Orthop Nurs 2005; 24:99–107.
Kang, M, Vives, MJ, Vaccaro, AR, The halo vest. principles of application and management of complications. J Spinal Cord Med 2003; 26:186–192.
7. Lethaby, A, Temple, J, Santy, J. Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database Syst Rev. 4, 2008. [CD004551].
Patterson, MM. Multicenter pin care study. Orthop Nurs. 2005; 24:349–360.
9. Saeed, MU, Dacuycuy, MA, Kennedy, DJ, Halo pin insertion-associated brain abscess. case report and review of the literature. Spine 2007; 32:E271–E274.
10. Wu, SC, Crews, RT, Zelen, Cet al. Use of chlorhexidine-impregnated patch at pin site to reduce local morbidity. the ChiPPS pilot trial,. Int Wound J 2008; 5:416–422.
Bernardo, LM. Evidence-based practice for pin site care in injured children. Orthop Nurs. 2001; 20:29–34.
Davis, P, Lee-Smith J, Booth, J, et al, Pin site management . towards a consensuspart 2. J Orthop Nurs 2001; 5:125–130.
Lee-Smith J, Santy, J, Davis, P, et al, Pin site management . towards a consensuspart 1. J Orthop Nurs. 2001; 5:37–42.
McKenzie, LL. In search of a standard for pin site care. Orthop Nurs. 1999; 18:73–78.