Halo Ring and Vest Care
A halo ring attached to a halo vest (commonly referred to as a halo) is designed to immobilize and stabilize the cervical spine. A halo ring and vest may be used alone or in conjunction with surgery for the patient with an unstable cervical spine, as a result of spinal fracture or dislocation; degenerative processes, such as C1-C2 changes from rheumatoid arthritis; or spinal surgery. With the use of the halo ring and vest, vertebral column movement is prevented and subsequent risk of the injury to the spinal cord is reduced.2 The halo ring and vest may be used as a primary definitive treatment to stabilize the cervical spine, before surgery to reduce spine deformity, or after surgery as an adjunct to interval cervical fixation. This procedure focuses on the management of the patient who needs immobilization with a halo ring and vest.
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of neuroanatomy and physiology is necessary.
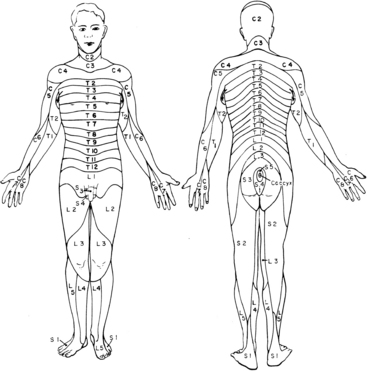
• The nurse needs to be knowledgeable about the anatomy and physiology of the spinal column, the special anatomy of the cervical vertebrae, the spinal cord, and the cervical spinal nerves and their areas of peripheral innervation. In addition, the nurse must understand the pathophysiology and manifestations of spinal cord trauma, including spinal shock, ascending edema, and related impairment of respiratory function, vasomotor tone, and autonomic nervous system function.
• The nurse must be knowledgeable about the signs and symptoms of new injury or extension of spinal cord injury and the needed interventions.
• Immobilization assists in maintenance of vertebral alignment. In the case of an unstable vertebral column, it also reduces the risk for new injury to the spinal cord.
• A number of treatment options are available to manage cervical injuries. The specific treatment for a particular patient depends on the type of injury, the level of injury (e.g., C2 as compared with C6), the specific classification of the injury, and patient characteristics.
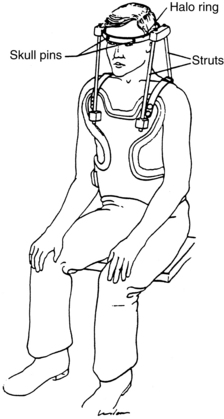
• A halo ring device is a graphite ring attached to the skull with four stabilizing pins (two anterior and two posterolateral; see Fig. 97-3). The pins are threaded through holes in the ring, screwed into the outer table of the skull, and locked into place.
• Direct traction may be applied to the halo ring device with a rope and pulley or cable and bracket alignment system and weights (see Procedures 97 and 100). Patients with a halo ring, pins, and traction applied with weights are cared for similarly to patients in cervical traction with tongs (see Procedures 97 and 100).
• When alignment of the cervical spine is achieved, long-term immobilization of the spine can be achieved by attaching the ring to a body vest or a custom molded body jacket, which allows for mobility of the patient (Fig. 98-1).2,3
• With the halo ring and pins in place, traction can be discontinued and a halo vest and struts added for long-term immobilization of the cervical neck (see Fig. 98-1). The advantage of this approach is that the patient can sit upright, mobilize out of bed, and ambulate, if able, while the cervical spine remains stable.
• The nurse must be familiar with the components of the halo-vest device, including the halo ring and pins, anterior and posterior posts, vest screws, front and back panels of the vest, and shoulder and side buckles.
• Basic cardiac life support knowledge and skills are essential.
• It is important that the nurse knows how to access the patient’s anterior chest to administer cardiopulmonary resuscitation (CPR) if cardiac arrest occurs. Refer to information from the manufacturer of the halo vest for specific information on emergency access to the chest. Some vests have a hinged closure; the vest can be lifted up at the hinge to allow quick access to the chest. Other vests are not hinged and require a wrench. The wrench must be available at all times and, depending on institution policy, may be maintained on the front of the vest for instant access to the chest. If the patient needs defibrillation, avoid touching the bars of the traction with the defibrillator.
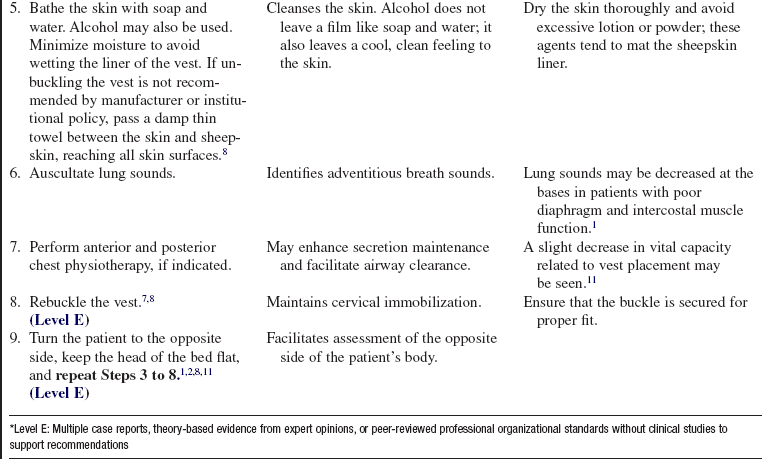
• The halo-vest side panels may be opened only when the patient is flat and supine.2,5,8 Unbuckling of the halo vest may result in loss of spine alignment and neurologic compromise.8 Follow manufacturer’s recommendations and institution policies for opening the vest.
• Because the halo vest limits movement of the head, patients must be taught to scan the environment for objects in their path that could lead to falls.
• The halo vest changes the center of gravity and limits movement, thus requiring adaptations for performing activities of daily living (ADLs).8
EQUIPMENT
Additional equipment to have as needed include the following:
PATIENT AND FAMILY EDUCATION
• Explain that the reason for the halo ring and vest device is to maintain cervical immobilization.  Rationale: Patient and family anxiety is decreased.
Rationale: Patient and family anxiety is decreased.
• Describe turning, positioning, and skin care procedures before performing them.  Rationale: Patient and family anxiety is decreased.
Rationale: Patient and family anxiety is decreased.
• If the patient is ambulatory, explain modifications in meeting basic needs such as bathing, toileting, eating, dressing, ambulation precautions, and safety needs.  Rationale: Self-care skills and awareness of special safety precautions are developed.
Rationale: Self-care skills and awareness of special safety precautions are developed.
• For patients who will be discharged home wearing a halo-vest device, begin a comprehensive teaching program with the patient and family.  Rationale: The patient and family are prepared for care in the home environment.
Rationale: The patient and family are prepared for care in the home environment.
• Explain to the patient and family that the patient cannot be turned with the struts (posts) of the halo-vest device.  Rationale: The patient and family are prepared for care in the home environment.
Rationale: The patient and family are prepared for care in the home environment.
• Explain that precautions must be used when the ambulatory patient with a halo-vest device gets in and out of a car and walks up and down stairs.  Rationale: The patient cannot move the head in the halo-vest device to look down.
Rationale: The patient cannot move the head in the halo-vest device to look down.
• Explain that driving, riding a motorcycle or bicycle, and operating machinery are unsafe with a halo-vest device.  Rationale: Patients recognize that they cannot turn their head.
Rationale: Patients recognize that they cannot turn their head.
• Explain that the pins of the halo transmit vibration and cold sensation to the patient’s skull.  Rationale: The patient and family are alerted to possible sensations during ADLs.
Rationale: The patient and family are alerted to possible sensations during ADLs.
• Explain that if the pins or screws become loose, the patient should contact the physician immediately. Inform the patient and family not to adjust the pins or screws.  Rationale: The patient and family are prepared for care in the home and can identify when emergency care may be needed.
Rationale: The patient and family are prepared for care in the home and can identify when emergency care may be needed.
• Explain that if the patient has any decline in neurologic function (i.e., decreased or abnormal sensory function; decline in motor ability; or increase in pain), the physician should be contacted immediately.  Rationale: Decline in neurologic function may indicate extension of spinal cord injury and the need for immediate interventions.
Rationale: Decline in neurologic function may indicate extension of spinal cord injury and the need for immediate interventions.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
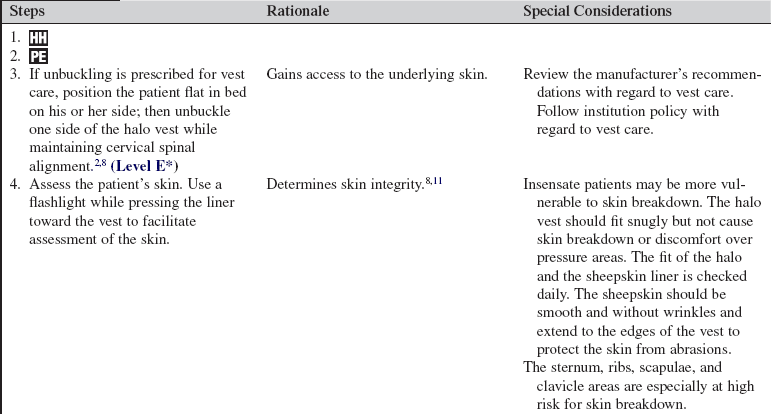
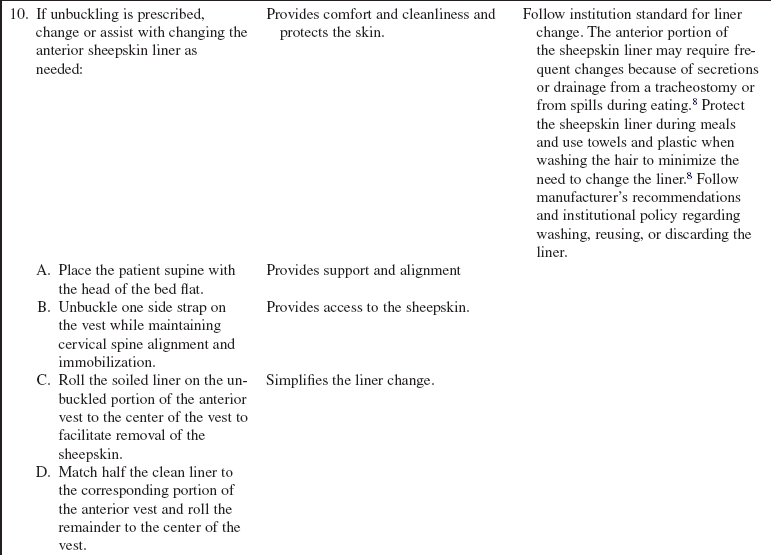
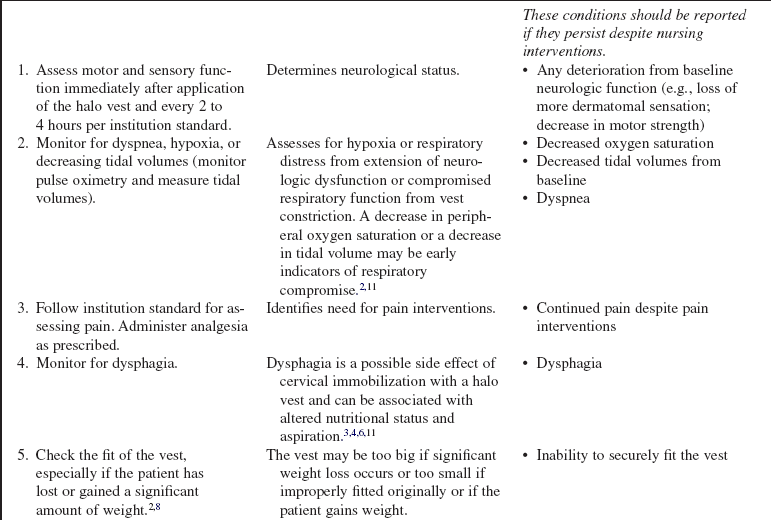
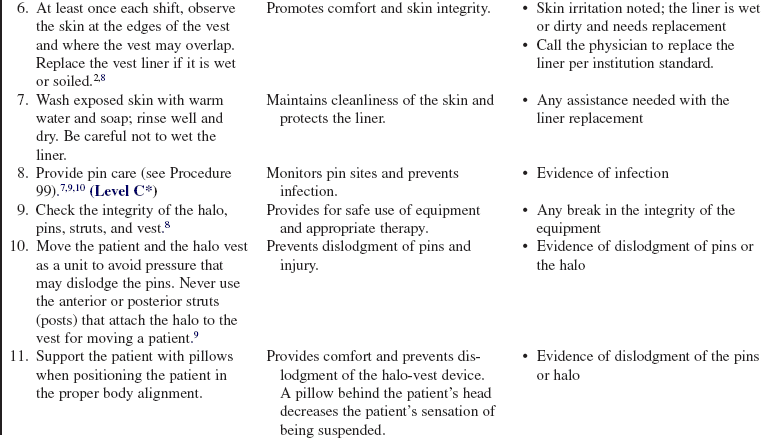
• Perform a complete neurologic assessment, including muscle strength and sensation1 (Figs. 98-2 and 98-3; Table 98-1) before and after halo ring and vest placement and at intervals as prescribed or as designated by institutional protocols thereafter.  Rationale: Baseline data are provided.
Rationale: Baseline data are provided.
Table 98-1
| Motor Score | Indicators |
| 5 | Normal muscle strength; can maintain high degree of function against maximal resistance. |
| 4 | The muscle can go through its normal range of motion, but it can be overcome by increased resistance. |
| 3 | The muscle can go through its normal range of motion against gravity only; it cannot tolerate external resistance. |
| 2 | The muscle contracts weakly; it does not have sufficient strength to overcome gravity. |
| 1 | Visible or palpable muscle contractions may be seen or felt, but no movement is found in the limb. |
| 0 | Complete paralysis; no evidence of motor function. |
(Adapted from Hickey J: The clinical practice of neurological and neurosurgical nursing, ed 4, Philadelphia, 1997, JB Lippincott.)
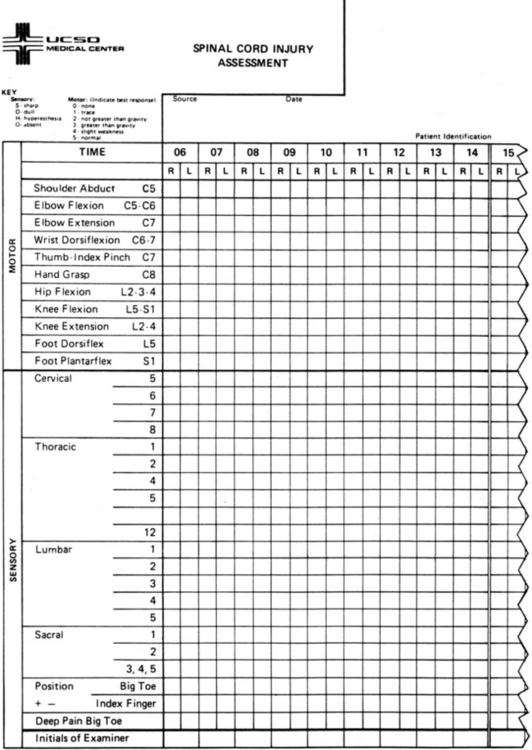
Figure 98-2 Sample of flow sheet documentation form for motor and sensory testing. (From University of California–San Diego Medical Center.)
• Obtain vital signs before halo ring and vest placement.  Rationale: Baseline data are provided.
Rationale: Baseline data are provided.
• Assess for difficulty swallowing and risk for aspiration.4,11  Rationale: Assessment identifies a patient at high risk and the need to modify oral intake.
Rationale: Assessment identifies a patient at high risk and the need to modify oral intake.
• Assess the skin at the edges of the vest and where the vest may overlap for redness or abrasion, especially over bony prominences.8,11  Rationale: Skin irritation related to the halo-vest device is identified.
Rationale: Skin irritation related to the halo-vest device is identified.
• Check the fit of the vest for tightness or looseness.  Rationale: The need for change or modification of the vest is identified. Patient weight loss may contribute to vest looseness.
Rationale: The need for change or modification of the vest is identified. Patient weight loss may contribute to vest looseness.
• Check the halo vest for loose straps or screws, dirt, odor, or evidence of the need to repair the vest.  Rationale: The vest may need to be repaired or the sheepskin liner changed.
Rationale: The vest may need to be repaired or the sheepskin liner changed.
Patient Preparation
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Assist patients as they lie supine in a neutral position with proper body alignment for the purpose of halo vest application, liner change, and routine skin care.  Rationale: Patients are kept safe and accessible for inspection.
Rationale: Patients are kept safe and accessible for inspection.
• Observe the sides and back of the vest and adjacent skin with the patient standing, if possible.  Rationale: Observation provides an opportunity to inspect all areas in which the skin and vest come in contact.
Rationale: Observation provides an opportunity to inspect all areas in which the skin and vest come in contact.
References
1. Blissitt, PA. Spinal cord injury. In: Carlson KK, ed. Advanced critical care nursing. Philadelphia: Saunders; 2009:637–680.
2. Bono, CM. The halo fixator. J Am Acad Orthop Surg. 2007; 15:728–737.
3. Canale, ST, Beaty, JH, Cervical spine injuries Canale ST, Beaty JH, eds.. Campbell’s operative orthopaedics. ed 11. Mosby, Philadelphia, 2008:1776–1777.
![]() 4. Hayes, VM, Silber, JS, Siddiqi, FN, et al. Complications of halo fixation of the cervical spine. Am J Orthop. 2005; 34:271–276.
4. Hayes, VM, Silber, JS, Siddiqi, FN, et al. Complications of halo fixation of the cervical spine. Am J Orthop. 2005; 34:271–276.
![]() 5. Jerome, Medical. Application instructions for Jerome halo traction systems. Moorestown, NJ: Jerome Medical; 2003.
5. Jerome, Medical. Application instructions for Jerome halo traction systems. Moorestown, NJ: Jerome Medical; 2003.
![]() 6. Kang, M, Vives, MJ, Vaccaro, AR, The halo vest. principles of application and management of complications. J Spinal Cord Med 2003; 26:186–192.
6. Kang, M, Vives, MJ, Vaccaro, AR, The halo vest. principles of application and management of complications. J Spinal Cord Med 2003; 26:186–192.
7. Lethaby, A, Temple, J, Santy, J. Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database Syst Rev. 4, 2008. [CD004551].
![]() 8. Patchen, SJ, Timyan, L, Atherton, S. Your life in a halo made easier,. Miami and Moorestown, NJ: University of Miami School of Medicine and Jerome Medical; 2002.
8. Patchen, SJ, Timyan, L, Atherton, S. Your life in a halo made easier,. Miami and Moorestown, NJ: University of Miami School of Medicine and Jerome Medical; 2002.
![]() 9. Patterson, MM. Multicenter pin care study. Orthop Nurs. 2005; 24:349–360.
9. Patterson, MM. Multicenter pin care study. Orthop Nurs. 2005; 24:349–360.
10. Saeed, MU, Dacuycuy, MA, Kennedy, DJ, Halo pin insertion-associated brain abscess. case report and review of the literature. Spine 2007; 32:E271–E274.
11. Taitsman, LA, Altman, DT, Hecht, AC, et al. Complications of cervical halo-vest orthoses in elderly patients. Orthopedics. 2008; 31:446.