Transcranial Doppler Monitoring
Transcranial Doppler Monitoring
Transcranial Doppler scan measures blood flow velocities in the major branches of the circle of Willis through an intact skull. This measurement supports the grading of vasospasm severity, localization of intracranial stenoses or occlusions, detection of cerebral emboli, monitoring of hemodynamic changes with impaired intracranial perfusion, and assessment of the impact of therapeutic interventions on intracranial hemodynamics.7–9,18,24
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of neuroanatomy and physiology is needed.
• Clinical and technical competence related to transcranial Doppler (TCD) ultrasound scan is necessary.
• Noninvasive assessment of the intracranial vasculature is indicated for patients with a subarachnoid hemorrhage, ischemic stroke, sickle cell disease, cerebral emboli, impaired vasomotor reactivity, cerebral circulatory arrest, and other neurovascular disorders.15,21
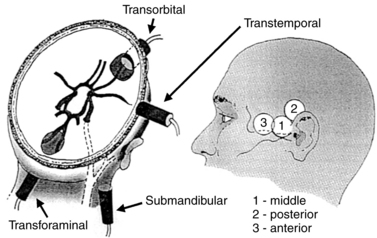
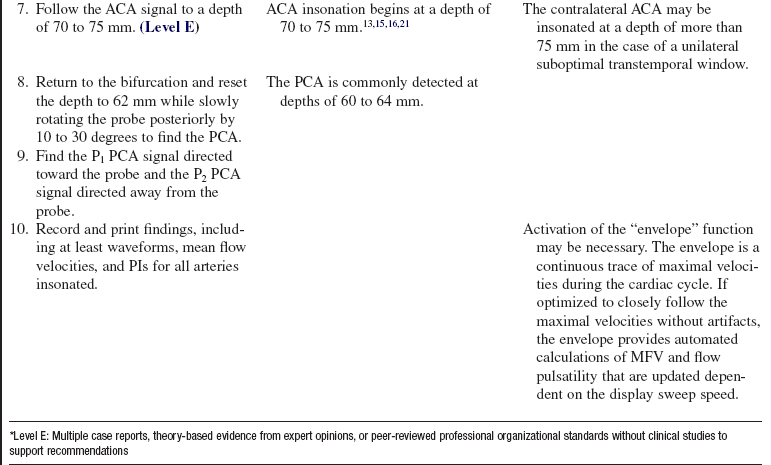
• Successful ultrasound penetration through the skull is possible through intracranial windows, which either lack bone (burr holes, flaps) or consist of thinner bone structure compared with the overall cranial bone thickness. Four windows are available for insonation: temporal, orbital, foraminal, and submandibular (Fig. 93-1).1–4
• The transtemporal window allows insonation of the middle cerebral artery (MCA), the anterior cerebral artery (ACA), the posterior cerebral artery (PCA), and the anterior and posterior communicating arteries (AComA and PComA).1–4
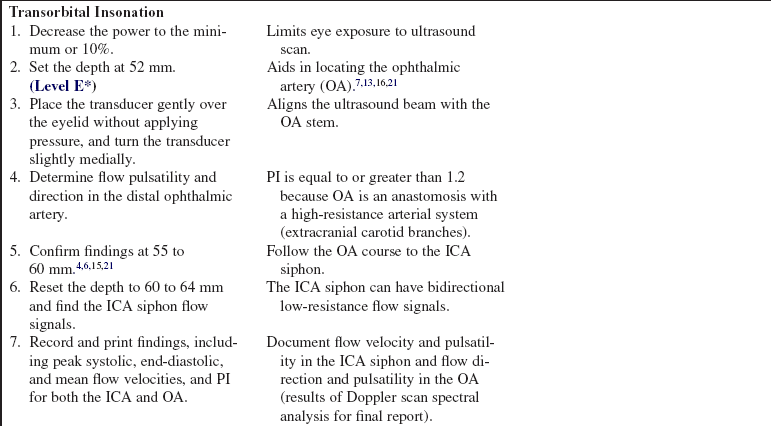
• The transorbital window allows insonation of the ophthalmic artery (OA) and the internal carotid artery (ICA) siphon.1–4
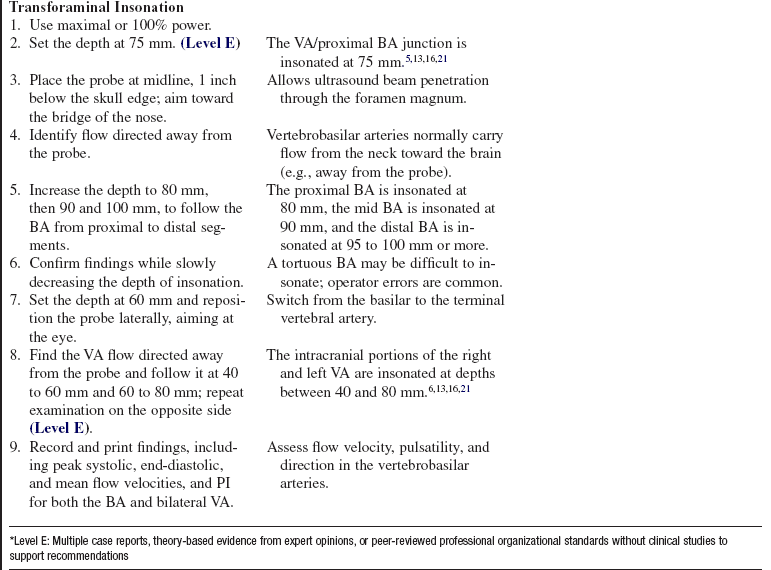
• The transforaminal window allows insonation of the vertebral arteries (VAs) and the basilar artery (BA).1–4
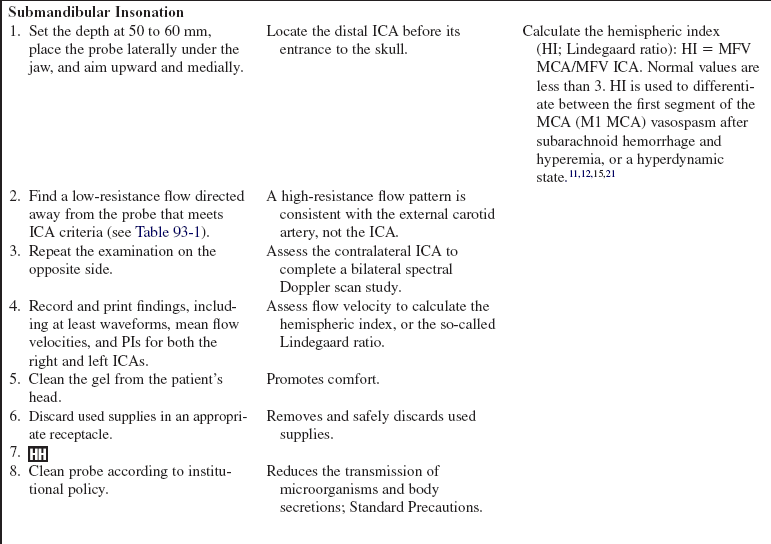
• The submandibular window allows insonation of the ICA as it enters the skull.1–4 TCD scan locates both the depth and direction of arterial blood flow relative to the transducer position and the ultrasonic beam direction. Flow moving toward the transducer is displayed as a waveform with a positive velocity spectrum, whereas flow moving away from the transducer is displayed as a waveform with a negative velocity spectrum.1–4,12,16
• The TCD scan measures cerebral blood flow velocities that should not be equated to cerebral blood flow (CBF) volume. TCD is an indirect reflection of CBF.4,15,21
• The examination should begin with maximal power and gate settings (e.g., power, 100%; gate, 10 to 15 mm) to expedite identification of the temporal window and various arterial segments. Once a good temporal window is established, the power may be reduced to adhere to the U.S. Food and Drug Administration (FDA) principles of (1) “as low as reasonably achievable” (ALARA) and (2) minimization of overall time of patient exposure to ultrasound scan. Transorbital examination should always be performed with minimal power (e.g., 10%) to avoid potential side effects from the heating of orbital structures.1–4
• The highest velocity signals for each arterial segment studied, and any abnormal or unusual waveforms, should be measured and stored in the system’s computer.3
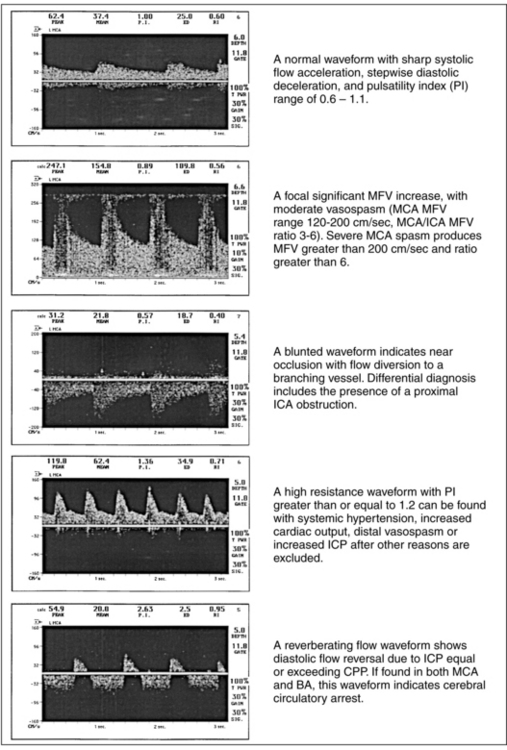
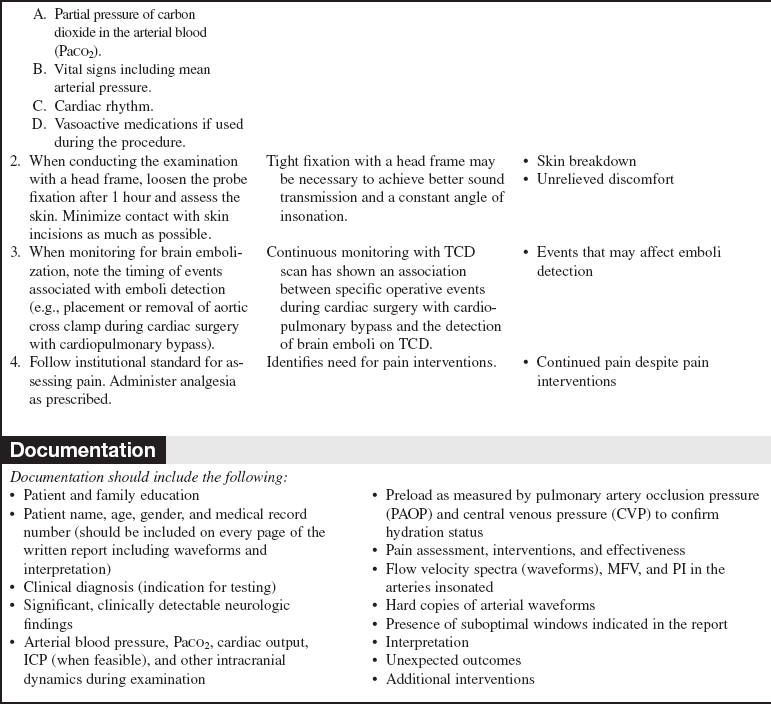
• Criteria for normal insonation depths, flow direction, and mean flow velocities are used for appropriate identification of arteries and diagnosis of abnormalities (Fig. 93-2 and Table 93-1).2,15,18,21
Table 93-1
Depth, Direction, and Mean Flow Velocities for Circle of Willis Arteries*
*Depth and MFV ranges may vary slightly between reference studies.
†Toward the probe indicates a positive (+) waveform; away from the probe indicates a negative (–) waveform.
(Adapted with permission from Alexandrov AV: Transcranial Doppler sonography: principles, examination technique and normal values, Vasc Ultrasound Today 10:141-160, 1998.)
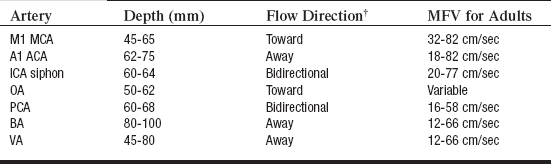
• Criteria for determination of a normal examination are listed in Table 93-2.2,15,18,21
Table 93-2
Criteria for Normal TCD Scan Findings
(Reprinted with permission from Alexandrov AV: Transcranial Doppler sonography: principles, examination technique and normal values, Vasc Ultrasound Today 10:141-160, 1988.)
• Criteria supporting differential diagnosis are listed in Table 93-3.2,15,18,21
Table 93-3
| Problem | Findings | Differential Diagnosis |
| Arterial stenosis | Focal MFV increase above normal values, turbulence, bruits Flow diversion to adjacent arteries Flow alteration distal to site of stenosis (deceleration, low PIs) |
Primary arterial stenosis Compensatory flow increase Adjacent artery occlusion Hyperemia |
| Arterial near occlusion | Blunted waveform Focal decrease in MFV Slow systolic acceleration Slow flow deceleration Flow diversion to adjacent arteries |
Near occlusion at the site of insonation Arterial occlusion proximal to insonation site Incorrect vessel identification |
| Arterial occlusion | No detectable flow Good unilateral window of insonation High-resistance flow proximal to occlusion Flow diversion to adjacent arteries |
Primary arterial occlusion Incorrect vessel identification Mass effect |
| Arterial vasospasm* | Proximal vasospasm: Focal or diffuse elevation of MFV without parallel FV increase in feeding extracranial arteries; HI greater than 3 Distal vasospasm: Focal increase in flow pulsatility (PI greater than or equal to 1.2), indicating increased resistance distal to site of insonation Increase in MFV in the involved and adjacent arteries may not be present |
Vasospasm Hyperemia Vasospasm with hyperemia Altered cerebral autoregulation Increased intracranial pressure |
| Increased intracranial pressure | Decreased EDV or absent end-diastolic flow Rapid flow deceleration PI greater than or equal to 1.2 Note that these findings may be present in patients with increased cardiac output or elevated blood pressure and in elderly individuals |
The presence of PI greater than or equal to 1.2 and positive end-diastolic flow in all arteries may be caused by the following: Hyperventilation Hypertension Increased ICP Unilateral PI greater than or equal to 1.2 may be caused by the following: Compartmental ICP increase Stenoses distal to the site of insonation PI greater than or equal to 2.0 associated with absent end-diastolic flow is caused by extreme elevations in ICP and possible cerebral circulatory arrest |
| Cerebral circulatory arrest | Reversed end-diastolic flow or reverberating flow pattern or Minimal systolic flow acceleration with no end-diastolic flow or Absent flow signals in all intracranial arterial systems |
Possible or probable circulatory arrest; measure both MCA and BA for 30 minutes; then reassess (transient arrest may occur during transient ICP increase or low blood pressure values) |
*Vasospasm criteria have been well established for the proximal MCA.9,14,15 Fewer criteria and validation studies are available for the posterior circulation vessel and the anterior cerebral artery.2,14,15 Institutions may set other ranges for possible vasospasm in these vessels.
• Hemispheric index (HI, also known as the Lindegaard ratio) helps to differentiate vasospasm severity and hyperdynamic blood flow changes (HI = mean flow velocity [MFV] ipsilateral MCA/MFV ipsilateral ICA). Normal values are less than 3.11,15,18,21
• The diameter of the vasospastic artery in aneurysmal subarachnoid hemorrhage is inversely related to the mean flow velocity. MCA vasospasm may be further classified as mild, moderate, severe, or critical.1,12,18,21 Severity of cerebral vasospasm is assessed by MFV value (cm/s) or MCA/ICA ratio10:
 Mild vasospasm has an MFV value of less than 120 or an MCA/ICA ratio of less than 3.
Mild vasospasm has an MFV value of less than 120 or an MCA/ICA ratio of less than 3.
 Moderate vasospasm has an MFV value from 120 to 150 or an MCA/ICA ratio from 3 to 5.
Moderate vasospasm has an MFV value from 120 to 150 or an MCA/ICA ratio from 3 to 5.
 Severe vasospasm has an MFV value from 151 to 200 or an MCA/ICA ratio greater than 6.
Severe vasospasm has an MFV value from 151 to 200 or an MCA/ICA ratio greater than 6.
 Critical vasospasm has an MFV value greater than 200 or an MCA/ICA ratio greater than 6.
Critical vasospasm has an MFV value greater than 200 or an MCA/ICA ratio greater than 6.
• Pulsatility of flow refers to vessel resistance and is measured with the pulsatility index (PI); normal range for PI is 0.6 to 1.1.2,4,15,21 PI (Gosling-King) = [velocity (peak systole) − velocity (end diastole)] ÷ velocity (mean).4,15,21
• Hyperventilation increases the PI and decreases mean flow velocity.4,15,21
• Hypercapnia decreases PI and increases mean flow velocity.4,15,21
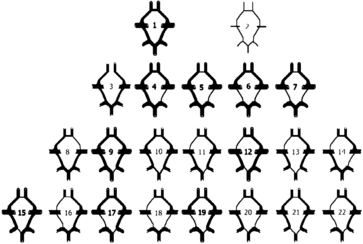
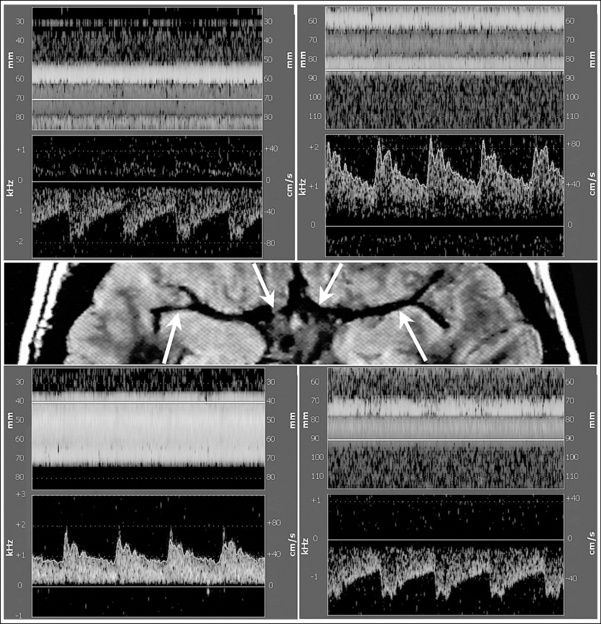
• Anatomic variations in the circle of Willis are common (Fig. 93-3).2,4,15,21 Inability to find an artery with the TCD scan should not be interpreted as arterial occlusion in the absence of other abnormal flow findings (e.g., secondary signs such as high resistance and flow diversion).4,15,21
• Clinical conditions, neurologic findings, and the effects of medications (dehydration or increased blood viscosity, hypertension or hypotension) should correlate with examination findings.2,4,15,21
• Although subjective, differentiation of Doppler sounds assists with identification of arterial segments and altered flow patterns.2,4
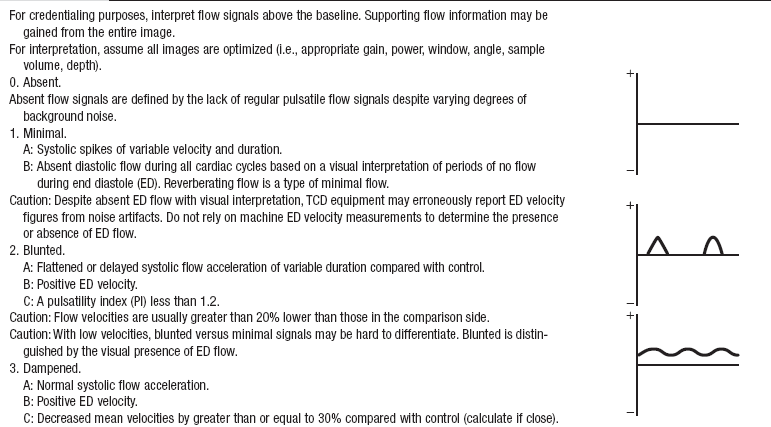
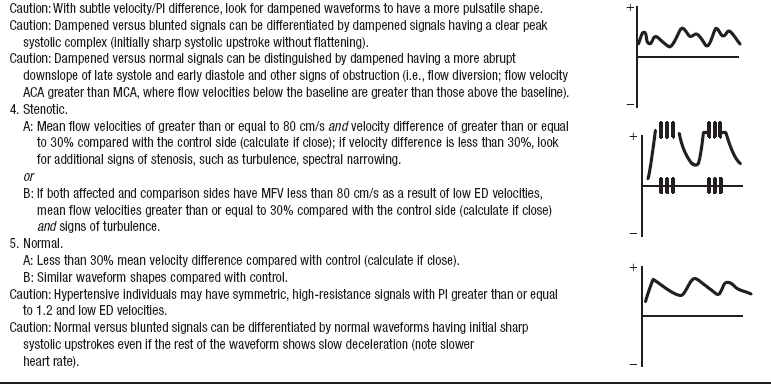
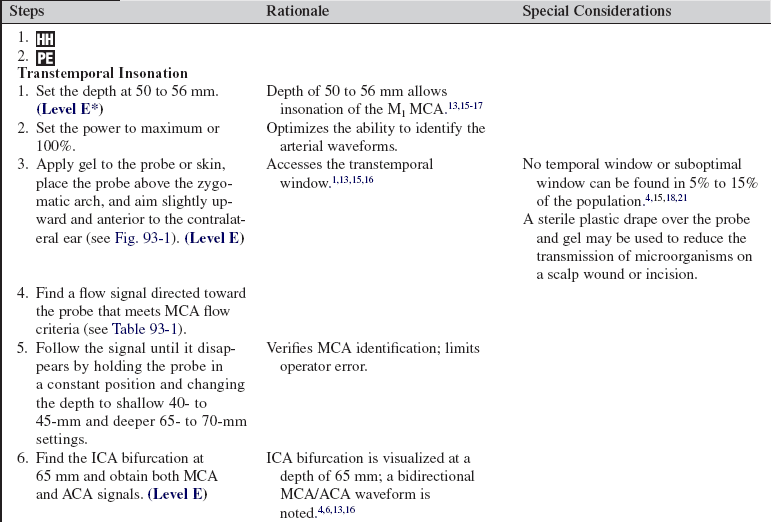
• Proximal extracranial, focal intracranial, and distal circulatory conditions are determinants of waveform patterns.2,4 Waveform classification in patients with ischemic strokes is standardized with use of the Thrombolysis in Brain Ischemia (TIBI) grading scale (Fig. 93-4 and Table 93-4).9 The TIBI grading system was prospectively validated against angiography; it has excellent reproducibility with greater than 90% agreement in waveform interpretation among expert TCD scan users.7,8,22 The TIBI system was implemented in a multicenter randomized clinical trial of ultrasound scan–enhanced thrombolysis for acute ischemic stroke to demonstrate superior recanalization rates when systemic tissue plasminogen activator (TPA) therapy was monitored with TCD scan compared with TPA given without ultrasound scan.5,7–9,18
• New technology using power motion Doppler (PMD or M-mode) scan can be used to facilitate window and vessel identification and guide spectral Doppler sampling and may reduce the time and effort necessary to learn TCD scanning (see Fig. 93-5).14,17,19,20,23
PATIENT AND FAMILY EDUCATION
• Explain the purpose of the diagnostic test and the procedure for testing.  Rationale: Explanation may decrease patient and family anxiety.
Rationale: Explanation may decrease patient and family anxiety.
• Explain the need for the patient to remain still and quiet during the procedure.  Rationale: This explanation may facilitate patient cooperation and completion of the examination.
Rationale: This explanation may facilitate patient cooperation and completion of the examination.
• Explain that the procedure does not cause any discomfort to the patient.  Rationale: This explanation may decrease patient and family anxiety.
Rationale: This explanation may decrease patient and family anxiety.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
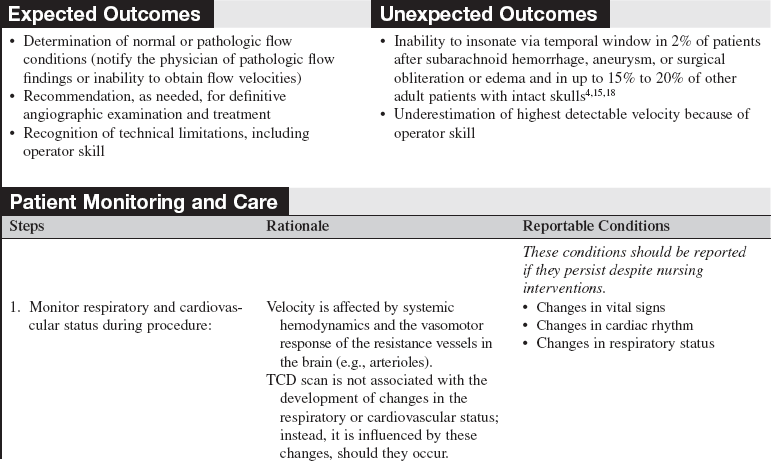
• Review patient history.  Rationale: The TCD scan may be used to assist with the diagnosis and management of a number of intracranial arterial conditions, including vasospasm, hyperemia, stenosis, occlusion, intracranial hypertension, cerebral circulatory arrest, cerebral embolization, and vasomotor testing.
Rationale: The TCD scan may be used to assist with the diagnosis and management of a number of intracranial arterial conditions, including vasospasm, hyperemia, stenosis, occlusion, intracranial hypertension, cerebral circulatory arrest, cerebral embolization, and vasomotor testing.
• Obtain the patient’s blood pressure via arterial line or cuff.  Rationale: The arterial blood pressure may contribute to the flow velocity and waveform pattern.
Rationale: The arterial blood pressure may contribute to the flow velocity and waveform pattern.
• Assess the patient’s heart rate and rhythm.  Rationale: Cardiac dysrhythmias may contribute to the flow velocity and waveform pattern.
Rationale: Cardiac dysrhythmias may contribute to the flow velocity and waveform pattern.
• Assess preload or hydration state.  Rationale: Dehydration may decrease flow velocity because of an increase in blood viscosity and decreased preload pressures.
Rationale: Dehydration may decrease flow velocity because of an increase in blood viscosity and decreased preload pressures.
• Assess for hyperventilation or hypercapnia.  Rationale: The carbon dioxide level may promote vasoconstriction (hyperventilation) or vasodilation (hypercapnia).
Rationale: The carbon dioxide level may promote vasoconstriction (hyperventilation) or vasodilation (hypercapnia).
• Assess for pharmacologic agents that may affect velocity findings (e.g., vasodilators, vasopressors).  Rationale: Vasoconstriction and vasodilation may affect flow velocity.
Rationale: Vasoconstriction and vasodilation may affect flow velocity.
• Assess for other factors that may affect velocity findings (e.g., age, hematocrit [Hct], hemoglobin [Hgb], metabolic demand).  Rationale: Velocities decrease with age; anemia and increased metabolic demand increase velocities.
Rationale: Velocities decrease with age; anemia and increased metabolic demand increase velocities.
• Measure intracranial pressure (ICP) and determine cerebral perfusion pressure (CPP) and other intracranial dynamics available (e.g., arterial oxygen saturation, jugular venous oxygen saturation, and brain tissue oxygenation).  Rationale: These factors may influence the pulsatility of flow and end-diastolic velocities.
Rationale: These factors may influence the pulsatility of flow and end-diastolic velocities.
• Assess the patient’s neurologic status.  Rationale: Provides baseline data.
Rationale: Provides baseline data.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient understands preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Assist the patient with positioning. The supine position is best for insonation via the transtemporal, transorbital, or submandibular windows. If the patient is alert with a hemodynamically and neurologically stable condition, assist the patient to a sitting position for insonation through the transforaminal window. If the patient is unable to sit for transforaminal insonation, assist the patient to turn his or her head laterally; if this is not feasible, examine the patient supine with a smaller transducer with a removable handle or a monitoring probe.  Rationale: The transtemporal, transorbital, and submandibular windows are accessible with the patient in the supine position, whereas the transforaminal window requires a sitting position for proper probe angulation (see Fig. 93-1).
Rationale: The transtemporal, transorbital, and submandibular windows are accessible with the patient in the supine position, whereas the transforaminal window requires a sitting position for proper probe angulation (see Fig. 93-1).
• Ask the patient to close his or her eyes for insonation via the transorbital window.  Rationale: The probe is placed lightly, without pressure, on the eyelid and angled slightly medially to detect OA and ICA siphon flow signals.
Rationale: The probe is placed lightly, without pressure, on the eyelid and angled slightly medially to detect OA and ICA siphon flow signals.
• If necessary, ask the patient to hold his or her breath during insonation via the submandibular window.  Rationale: Breathing may produce audible and visual artifacts, obstructing assessment of the waveform.
Rationale: Breathing may produce audible and visual artifacts, obstructing assessment of the waveform.
References
![]() 1. Aaslid, R, Markwalder, TM, Nornes, H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982; 57:769–774.
1. Aaslid, R, Markwalder, TM, Nornes, H. Noninvasive transcranial Doppler ultrasound recording of flow velocity in basal cerebral arteries. J Neurosurg. 1982; 57:769–774.
![]() 2. Alexandrov, AV, Transcranial Doppler sonography. principles, examination technique and normal values. Vasc -Ultrasound Today 1998; 10:141–160.
2. Alexandrov, AV, Transcranial Doppler sonography. principles, examination technique and normal values. Vasc -Ultrasound Today 1998; 10:141–160.
![]() 3. Alexandrov, AV, Demchuk, AM, Burgin, WS. Insonation method and diagnostic flow signatures for transcranial power motion (M-mode) Doppler. J Neuroimaging. 2002; 12:236–244.
3. Alexandrov, AV, Demchuk, AM, Burgin, WS. Insonation method and diagnostic flow signatures for transcranial power motion (M-mode) Doppler. J Neuroimaging. 2002; 12:236–244.
![]() 4. Alexandrov, AV. Cerebrovascular ultrasound in stroke -prevention and treatment,. Oxford: Blackwell–Futura Publishing; 2004.
4. Alexandrov, AV. Cerebrovascular ultrasound in stroke -prevention and treatment,. Oxford: Blackwell–Futura Publishing; 2004.
![]() 5. Alexandrov, AV, et al. Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med. 2004; 351:2170–2178.
5. Alexandrov, AV, et al. Ultrasound-enhanced systemic thrombolysis for acute ischemic stroke. N Engl J Med. 2004; 351:2170–2178.
6. Alexandrov, AV, et al, Practice standards for transcranial Doppler (TCD) ultrasound. part Itest performance. J Neuroimaging 2007; 17:11–18.
![]() 7. Burgin, WS, et al. Transcranial Doppler criteria for recanalization after thrombolysis for middle cerebral artery stroke. Stroke. 2000; 31:1128–1132.
7. Burgin, WS, et al. Transcranial Doppler criteria for recanalization after thrombolysis for middle cerebral artery stroke. Stroke. 2000; 31:1128–1132.
![]() 8. Burgin, WS, et al. Validity and reliability of the thrombolysis in brain infarction (TIBI) flow grades. Stroke. 2001; 32:324–325.
8. Burgin, WS, et al. Validity and reliability of the thrombolysis in brain infarction (TIBI) flow grades. Stroke. 2001; 32:324–325.
![]() 9. Demchuk, AM, et al. Thrombolysis in brain ischemia (TIBI) Doppler flow grades predict clinical severity, early recovery, and mortality in patients treated with intravenous tissue plasminogen activator. Stroke. 2001; 32:89–93.
9. Demchuk, AM, et al. Thrombolysis in brain ischemia (TIBI) Doppler flow grades predict clinical severity, early recovery, and mortality in patients treated with intravenous tissue plasminogen activator. Stroke. 2001; 32:89–93.
10. Kassah, MY, Majid, A, Farooq, FU, et al, Transcranial Doppler. an introduction for the primary care physician. J Am Board Fam Med 2007; 20:65–71.
![]() 11. Lindegaard, KF, et al. Cerebral vasospasm diagnosis by means of angiography and blood velocity measurements. Acta Neurochir (Wien). 1989; 100:12–24.
11. Lindegaard, KF, et al. Cerebral vasospasm diagnosis by means of angiography and blood velocity measurements. Acta Neurochir (Wien). 1989; 100:12–24.
![]() 12. Lindegaard, KF, The role of transcranial Doppler in the management of patients with subarachnoid haemorrhage. a review. Acta Neurochir. 1999; 72(Suppl):59–71.
12. Lindegaard, KF, The role of transcranial Doppler in the management of patients with subarachnoid haemorrhage. a review. Acta Neurochir. 1999; 72(Suppl):59–71.
![]() 13. Lupetin, AR, et al, Transcranial Doppler sonography . part 1principles, technique, and normal appearances. Radiographics 1995; 15:179–191.
13. Lupetin, AR, et al, Transcranial Doppler sonography . part 1principles, technique, and normal appearances. Radiographics 1995; 15:179–191.
![]() 14. McCartney, JP, Thomas-Lukes, KM, Gomez, CR. Handbook of transcranial Doppler. New York: Springer; 1997.
14. McCartney, JP, Thomas-Lukes, KM, Gomez, CR. Handbook of transcranial Doppler. New York: Springer; 1997.
![]() 15. Moehring, MA, Spencer, MP. Power M-mode Doppler (PMD) for observing cerebral blood flow and tracking emboli. Ultrasound Med Biol. 2002; 28:49–57.
15. Moehring, MA, Spencer, MP. Power M-mode Doppler (PMD) for observing cerebral blood flow and tracking emboli. Ultrasound Med Biol. 2002; 28:49–57.
![]() 16. Moppet, IK, Mahajan, RP, Transcranial Doppler ultransonography in anaesthesia and intensive care. Br J Anaesth 2004; 93:710–724.
16. Moppet, IK, Mahajan, RP, Transcranial Doppler ultransonography in anaesthesia and intensive care. Br J Anaesth 2004; 93:710–724.
![]() 17. Ringelstein, EB, et al, Transcranial Doppler sonography. anatomical landmarks and normal velocity values. Ultrasound Med Biol 1990; 16:745–761.
17. Ringelstein, EB, et al, Transcranial Doppler sonography. anatomical landmarks and normal velocity values. Ultrasound Med Biol 1990; 16:745–761.
18. Saqqur, M, et al. Derivation of power M-Mode transcranial Doppler criteria for angiographic proven MCA occlusion. J Neuroimaging. 2006; 16:323–328.
![]() 19. Sloan, MA, Transcranial Doppler monitoring of vasospasm after subarachnoid hemorrhageTegeler CH, Baikian VL, Gomez CR, eds.. Neurosonology. 1996. Mosby: St Louis:156–171.
19. Sloan, MA, Transcranial Doppler monitoring of vasospasm after subarachnoid hemorrhageTegeler CH, Baikian VL, Gomez CR, eds.. Neurosonology. 1996. Mosby: St Louis:156–171.
![]() 20. Sloan, MA, et al, Assessment. transcranial Doppler ultrasonographyreport of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2004; 62:1468–1481.
20. Sloan, MA, et al, Assessment. transcranial Doppler ultrasonographyreport of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology 2004; 62:1468–1481.
![]() 21. Tegeler, CH, Babikian, VL, Gomez, CR. Neurosonology. St Louis: Mosby; 1996.
21. Tegeler, CH, Babikian, VL, Gomez, CR. Neurosonology. St Louis: Mosby; 1996.
22. Tsivgoulis, G, et al. Validation of transcranial Doppler with computed tomography angiography in acute cerebral ischemia. Stroke. 2007; 38:1245–1249.
23. Tsivgoulis, G, et al. Applications and advantages of power motion-mode Doppler in acute posterior circulation cerebral ischemia. Stroke. 2008; 39:1197–1204.
24. White, H, Venkatesh, B, Applications of transcranial Doppler in the ICU. a review. Intensive Care Med. 2006; 32(7):981–994.