Jugular Venous Oxygen Saturation Monitoring: Insertion (Assist), Patient Care, Troubleshooting, and Removal
Jugular venous oxygen saturation (SjVO2) catheters detect the oxygen saturation of hemoglobin in the blood after cerebral perfusion. The direct and derived parameters obtained from jugular venous oxygen saturation catheters reflect global cerebral oxygenation. Inclusion of jugular venous oxygen saturation data in the clinical management of the patient may prevent the secondary brain injury that occurs as a result of an imbalance between cerebral oxygen delivery and cerebral oxygen demand.2,43
PREREQUISITE NURSING KNOWLEDGE
• Fundamental understanding of neuroanatomy and physiology is needed.
• Knowledge of aseptic and sterile technique is necessary.
• The secondary brain injury that occurs as a result of an imbalance in oxygen supply and demand is accompanied by increased intracranial pressure (ICP), potential or actual compromise in cerebral perfusion, or other alterations that lead to cerebral ischemia.4,29,32
• Cerebral ischemia results in poor outcomes in critically ill patients.2,3,5,8,19,35,36
• Normal jugular venous oxygen saturation (SjVO2) values range from 55% to 70%.7,13,33,35,38,40 SjVO2 values less than 45% to 50% indicate relative cerebral ischemia, especially with frequent desaturations.7,9,10,12,13,18,25,39
• SjVO2 values greater than 70% may demonstrate hyperemia.8,21,23,26,28,31,32,40 Hyperemia occurs as the result of an increase in cerebral blood flow or hyperdilation of distal cerebrovascular resistance beds and is frequently accompanied by increases in ICP.20
• SjVO2 monitoring is recommended in patients at risk for global cerebral hypoxia, including those with acute severe traumatic brain injury (Glasgow Coma Scale [GCS] score equal to or less than 8)6,19,26,36,38; aneurysmal subarachnoid hemorrhage, including vasospasm9,24; intraoperative monitoring during craniotomy for tumor, abscess, aneurysm, arteriovenous malformation, spontaneous intracerebral hemorrhage,24 and carotid endarterectomy for carotid stenosis; intraoperative monitoring during cardiac surgery, especially hypothermic cardiopulmonary bypass and rewarming; patients successfully resuscitated; ICP and cerebral perfusion pressure (CPP) management; controlled hyperventilation for increased ICP; and barbiturate coma for refractory increased ICP.4
• Contraindications for SjVO2 monitoring include coagulopathies, cervical spine injury, local neck trauma, and impaired cerebral venous drainage.4
• The SjVO2 catheter is placed retrograde in the dominant internal jugular vein (usually the right internal jugular vein).11,14–17,23,33
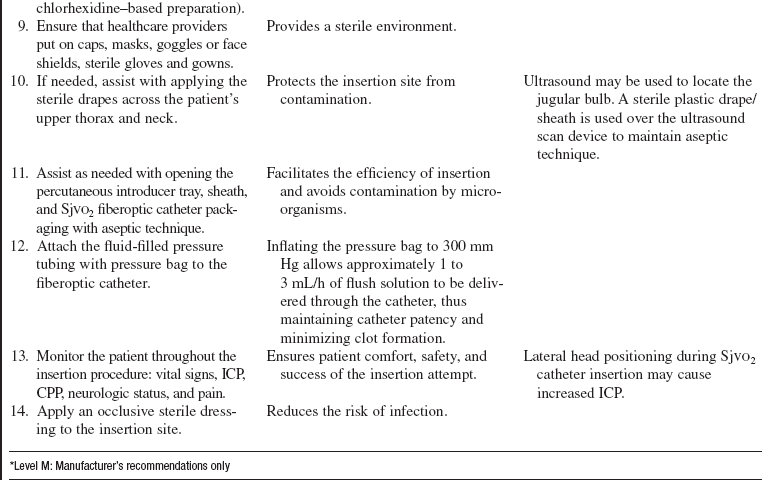
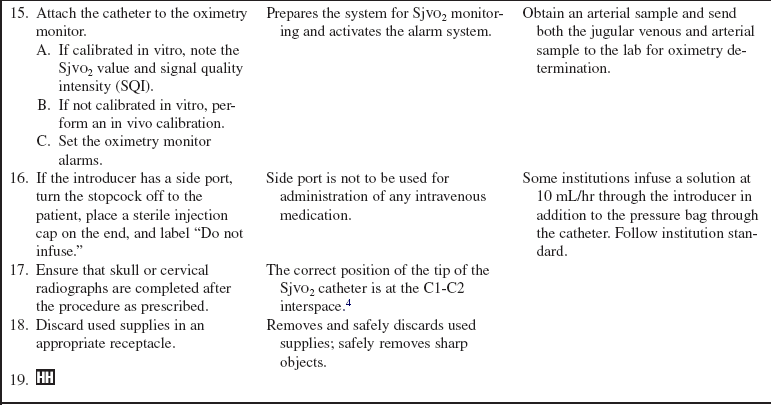
• The SjVO2 catheter tip is positioned at the location of the jugular bulb of the internal jugular vein.20,23 This is at the mastoid process, approximately at the C1-C2 interspace (Fig. 90-1).1 Ultrasound scan devices may be used to locate the jugular bulb to ease bedside placement.
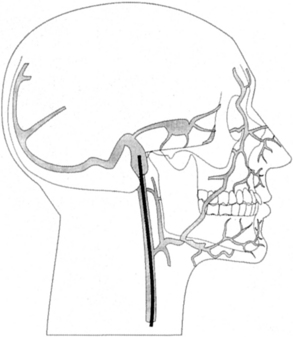
Figure 90-1 Placement of the jugular bulb venous catheter. (From Kidd KC, Criddle L: Using jugular venous catheters in patients with traumatic brain injury, Crit Care Nurse 21:16-22, 2001.)
• A decrease in SjVO2 (55%) may be due to increased demand as a result of pain, hyperthermia, shivering, agitation, or seizures. It may also be due to decreased delivery as a result of hyperventilation (hypocarbia), decreased cardiac output, hypotension, hypovolemia, anemia, hypoxia, and sepsis.4
• An increase in SjVO2 (70%) may be due to decreased demand as the result of hypothermia, anesthesia, paralytics, and sepsis. It may also be due to increased delivery.4
• Derived SjVO2 parameters include arteriovenous jugular oxygen content difference (AvjDO2), the cerebral extraction of oxygen (CEO2), and the cerebral metabolic rate of oxygen consumption (CMRO2).
 AvjDO2 reflects the relationship between cerebral blood flow (CBF) and CMRO2.27,28,35,41,42
AvjDO2 reflects the relationship between cerebral blood flow (CBF) and CMRO2.27,28,35,41,42
 Normal range: 4.0 to 8.0 mL/dL
Normal range: 4.0 to 8.0 mL/dL
 Calculation requires data obtained from both systemic arterial and jugular venous blood gas analysis
Calculation requires data obtained from both systemic arterial and jugular venous blood gas analysis
 CEO2 reflects the influence of cerebral blood volume change (CBV) and its effect on CBF and CMRO2. Blood volume flow is not equal to blood volume.27,35,41,45
CEO2 reflects the influence of cerebral blood volume change (CBV) and its effect on CBF and CMRO2. Blood volume flow is not equal to blood volume.27,35,41,45
 CMRO2 is the energy needed for cellular function.35,41 This parameter includes knowledge of the cerebral blood flow and AvjDO2 and is less frequently calculated in the clinical setting. Normal CMRO2 is 3.2 mL/100 g/min.
CMRO2 is the energy needed for cellular function.35,41 This parameter includes knowledge of the cerebral blood flow and AvjDO2 and is less frequently calculated in the clinical setting. Normal CMRO2 is 3.2 mL/100 g/min.
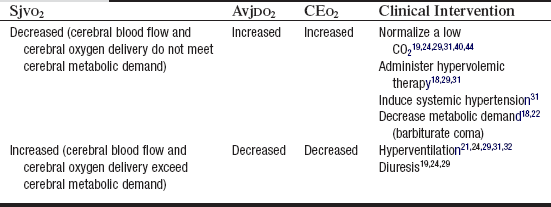
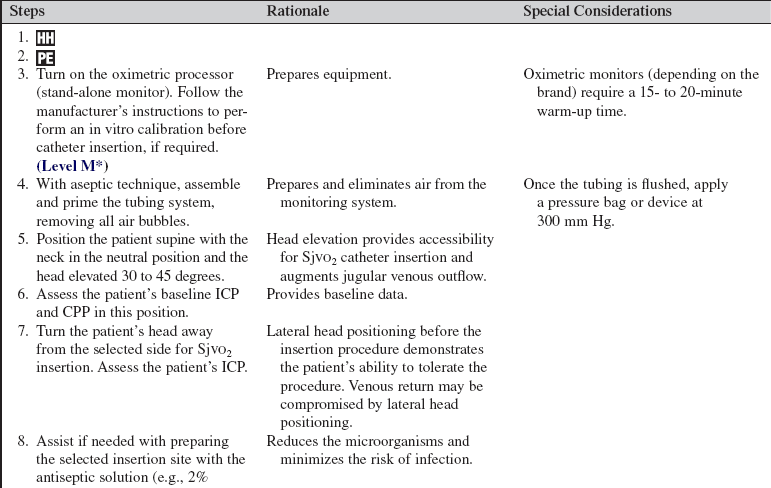
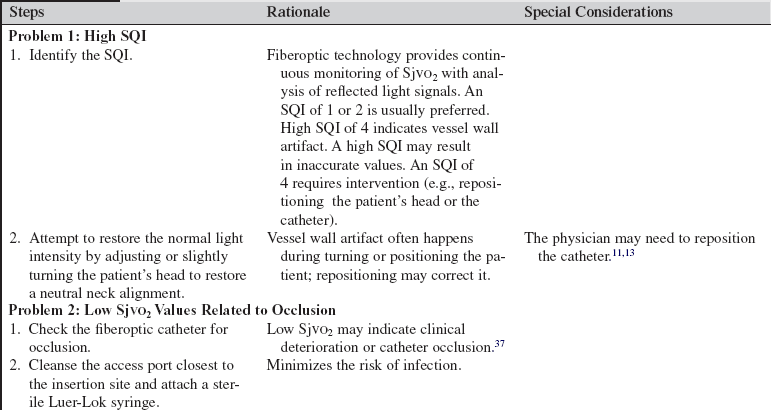
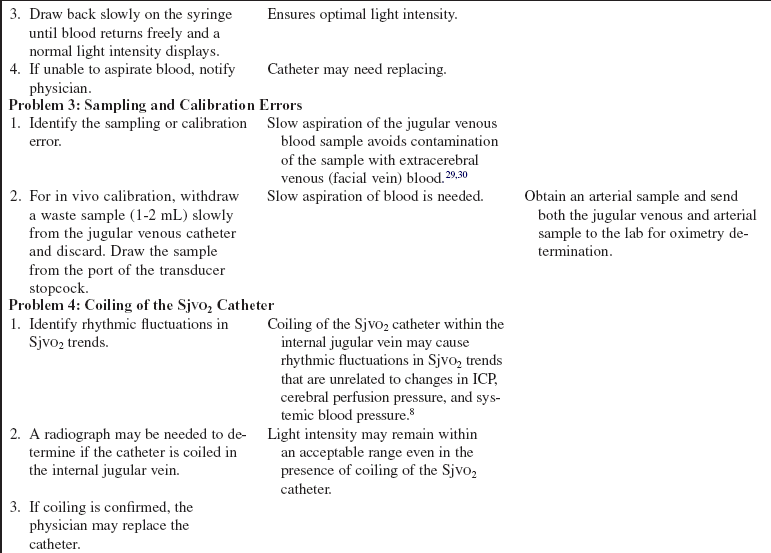
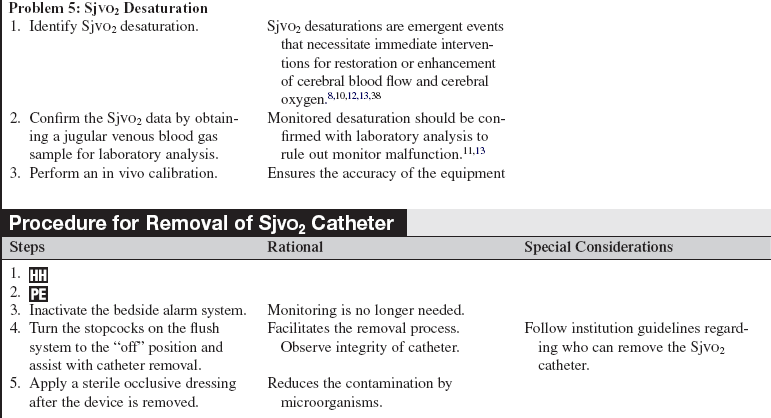
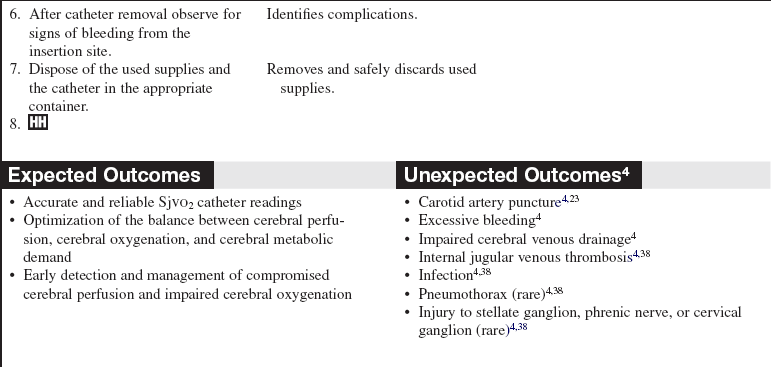
• The technology used for continuous SjVO2 monitoring is oximetry, which is based on the unique light absorption spectrum of oxyhemoglobin.40 Oximetry requires calibration, either in vivo, within the patient’s jugular vein, or in vitro, calibration before insertion, outside the body. Formulas and normal ranges for SjVO2 catheter data and calculations are included in Tables 90-1 and 90-2. Clinical interventions based on SjVO2 data are shown in Table 90-3.
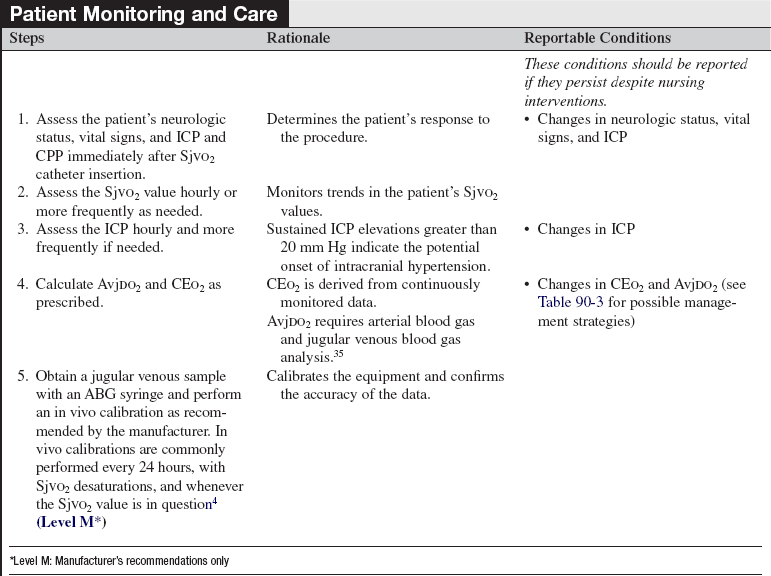
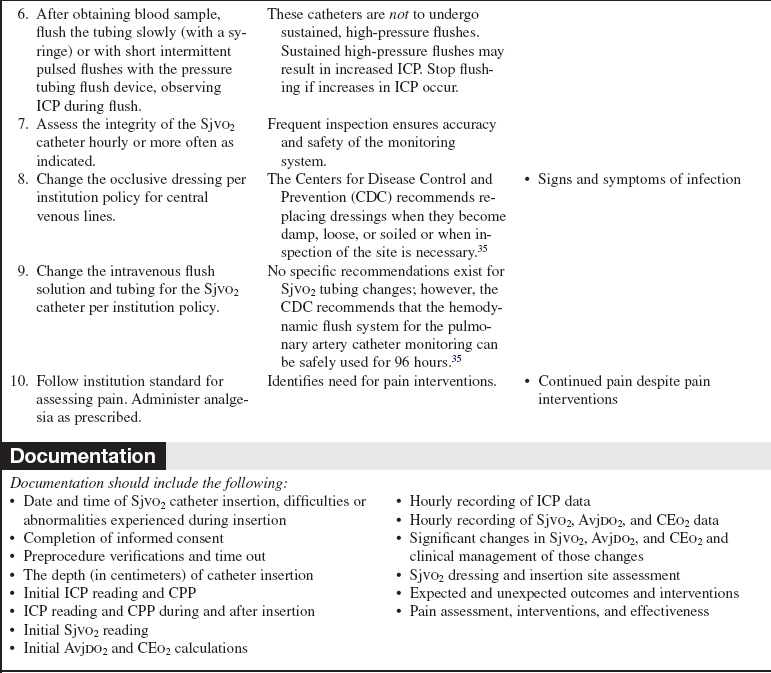
Table 90-1
Formulas for Calculations Using SjVO2 Data
| Calculations | Formula |
| AvjDO2 (mL/dL) | CaO2 (mL/dL) − CjVO2 (mL/dL) |
| CEO2 (%) | SaO2 (%) − SjVO2 (%) |
Table 90-2
Normal Ranges for SjVO2 Data and Calculations
| SjVO2 Data | Normal Ranges |
| SjVO2 | 55% − 70% |
| AvjDO2 | 4.0 to 8.0 mL/dL |
| CEO2 | 24% − 42% |
EQUIPMENT
• Antiseptic solution (e.g., 2% chorhexidine-based preparation)
• Surgical caps, gowns, goggles, sterile gloves, and gowns
• Sterile towels, half-sheets, and drapes
• Local anesthetic (lidocaine 1% or 2% without epinephrine)
• 5- or 10-mL Luer-Lok syringe with an 18-gauge needle (for drawing up of the lidocaine) and a 23-gauge needle (for administration of the lidocaine)
In addition, the following are needed (if they are not included in the kit):
 5 Fr percutaneous transvenous introducer catheter
5 Fr percutaneous transvenous introducer catheter
 4 Fr fiberoptic oximetric SjVO2 catheter
4 Fr fiberoptic oximetric SjVO2 catheter
• Optical module and connecting fiberoptic cable
• Oximetric monitor (typically a stand-alone monitor or module)
 A pressure waveform is not generated from these catheters; therefore, display of a bedside waveform is not necessary. The system provides 3 mL of fluid an hour to prevent clotting of the catheter.
A pressure waveform is not generated from these catheters; therefore, display of a bedside waveform is not necessary. The system provides 3 mL of fluid an hour to prevent clotting of the catheter.
• Pressure module and cable to interface the oximetric monitor to the bedside monitor
PATIENT AND FAMILY EDUCATION
• Assess patient and family understanding of SjVO2 catheter monitoring and its purpose.  Rationale: Knowledge of expectations may allay patient and family fears and anxiety.
Rationale: Knowledge of expectations may allay patient and family fears and anxiety.
• Explain the procedure for insertion, patient monitoring, and patient clinical interventions for the SjVO2 catheter.  Rationale: Clarification and repeated explanations may reinforce understanding and decrease anxiety.
Rationale: Clarification and repeated explanations may reinforce understanding and decrease anxiety.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s neurologic status and vital signs.  Rationale: A baseline neurologic examination provides information necessary for recognition of changes during and after catheter insertion.
Rationale: A baseline neurologic examination provides information necessary for recognition of changes during and after catheter insertion.
• Assess the patient for evidence of a local infection or local neck trauma. Verify that the patient does not have a cervical spine injury.  Rationale: These conditions are contraindications for SjVO2 catheter placement.38
Rationale: These conditions are contraindications for SjVO2 catheter placement.38
• Review current laboratory values such as complete blood count (CBC), prothombin time (PT) partial thromboplastin time (PTT), and international normalized ratio (INR).  Rationale: Abnormal coagulation study results may be a contraindication for SjVO2 catheter placement.38
Rationale: Abnormal coagulation study results may be a contraindication for SjVO2 catheter placement.38
• Assess for allergies.  Rationale: Insertion of the SjVO2 catheter may necessitate local anesthetic, an antiseptic to clean the site, and analgesia and sedation. Assessment minimizes the risk of allergic reaction.
Rationale: Insertion of the SjVO2 catheter may necessitate local anesthetic, an antiseptic to clean the site, and analgesia and sedation. Assessment minimizes the risk of allergic reaction.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Ensure that informed consent is obtained.  Rationale: Informed consent protects the rights of the patient and makes competent decision making possible for the patient; however, in emergency circumstances, time may not allow for the consent form to be signed.
Rationale: Informed consent protects the rights of the patient and makes competent decision making possible for the patient; however, in emergency circumstances, time may not allow for the consent form to be signed.
• Administer preprocedural analgesia or sedation as prescribed.  Rationale: Patients need to remain still during SjVO2 catheter insertion. Usually patients are unconscious and may be receiving continuous intravenous analgesia and sedative medications.
Rationale: Patients need to remain still during SjVO2 catheter insertion. Usually patients are unconscious and may be receiving continuous intravenous analgesia and sedative medications.
References
![]() 1. Bankier, AA, et al, Position of jugular oxygen saturation catheter in patients with head trauma. assessment by use of plain films. Am J Roentgenol 1995; 164:437–441.
1. Bankier, AA, et al, Position of jugular oxygen saturation catheter in patients with head trauma. assessment by use of plain films. Am J Roentgenol 1995; 164:437–441.
![]() 2. Bayir, H, et al. Promising strategies to minimize secondary brain injury after head trauma. Crit Care Med. 2003; 31(Suppl):S112–S117.
2. Bayir, H, et al. Promising strategies to minimize secondary brain injury after head trauma. Crit Care Med. 2003; 31(Suppl):S112–S117.
![]() 3. Bhutra, S, et al. Jugular venous oxygen saturation monitoring in comatose neurosurgical patients. JACP. 1999; 15(2):143–147.
3. Bhutra, S, et al. Jugular venous oxygen saturation monitoring in comatose neurosurgical patients. JACP. 1999; 15(2):143–147.
4. Blissitt, PA. Brain oxygen monitoring. In: Littlejohns LR, Bader MK, eds. AACN-AANN protocols for practice: monitoring technologies in critically ill neuroscience -patients. Sudbury, MA: Jones and Bartlett; 2009:103–144.
![]() 5. Bouma, GJ, et al, Cerebral circulation and metabolism -after severe traumatic brain injury. the elusive role of -ischemia. J Neurosurg 1991; 75:683–685.
5. Bouma, GJ, et al, Cerebral circulation and metabolism -after severe traumatic brain injury. the elusive role of -ischemia. J Neurosurg 1991; 75:683–685.
6. Bratton, SL, Chesnut, RM, Ghajar, J, et al, Brain oxygen monitoring and thresholds. guidelines for the management of -severe traumatic brain injuryA joint project of the Brain Trauma Foundation, American Association of Neurological Surgeons (AANS), Congress of Neurological Surgeons (CNS), AANS/CNS Joint Section on Neurotrauma and -Critical Care. J Neurotrauma. 2007; 24(Suppl 1):S65–S70.
![]() 7. Chan, MT, Re-defining the ischemic threshold for jugular venous oxygen saturation. a microdialysis study in -patient with severe head injury. Acta Neurochir 2005; 95:63–66. [(Suppl)].
7. Chan, MT, Re-defining the ischemic threshold for jugular venous oxygen saturation. a microdialysis study in -patient with severe head injury. Acta Neurochir 2005; 95:63–66. [(Suppl)].
![]() 8. Chieregato, A, et al, Detection of early ischemia in severe head injury by means of arteriovenous lactate differences and jugular bulb oxygen saturation. relationship with CPP, severity indexes and outcomepreliminary analysis. Acta Neurochirurgica. 2002; 81(Suppl):289–293.
8. Chieregato, A, et al, Detection of early ischemia in severe head injury by means of arteriovenous lactate differences and jugular bulb oxygen saturation. relationship with CPP, severity indexes and outcomepreliminary analysis. Acta Neurochirurgica. 2002; 81(Suppl):289–293.
![]() 9. Citerio, G, et al. Jugular saturation (SjVO2) monitoring in subarachnoid hemorrhage (SAH). Acta Neurochirugica. 1998; 71:316–319. [(Suppl)].
9. Citerio, G, et al. Jugular saturation (SjVO2) monitoring in subarachnoid hemorrhage (SAH). Acta Neurochirugica. 1998; 71:316–319. [(Suppl)].
![]() 10. Cormio, MA, et al. Elevated jugular venous oxygen saturation after severe head injury. J Neurosurg. 1999; 90:9–15.
10. Cormio, MA, et al. Elevated jugular venous oxygen saturation after severe head injury. J Neurosurg. 1999; 90:9–15.
![]() 11. Dearden, NM, Midgley, S. Technical considerations in continuous jugular venous oxygen saturation measurement. Acta Neurochirurgica. 1993; 59(Suppl):91–97.
11. Dearden, NM, Midgley, S. Technical considerations in continuous jugular venous oxygen saturation measurement. Acta Neurochirurgica. 1993; 59(Suppl):91–97.
![]() 12. Fandino, J, et al. Cerebral oxygenation and systemic trauma related factors determining neurological outcome after brain injury. J Clin Neurosci. 2000; 7:226–233.
12. Fandino, J, et al. Cerebral oxygenation and systemic trauma related factors determining neurological outcome after brain injury. J Clin Neurosci. 2000; 7:226–233.
![]() 13. Feldman, Z, Robertson, CS. Monitoring of cerebral hemodynamics with jugular bulb catheters. Crit Care Clin. 1997; 13:51–77.
13. Feldman, Z, Robertson, CS. Monitoring of cerebral hemodynamics with jugular bulb catheters. Crit Care Clin. 1997; 13:51–77.
![]() 14. Ferris, EB, et al. The validity of the internal jugular venous blood in studies of cerebral metabolism and blood flow in man. Am J Physiol. 1946; 147:517–521.
14. Ferris, EB, et al. The validity of the internal jugular venous blood in studies of cerebral metabolism and blood flow in man. Am J Physiol. 1946; 147:517–521.
![]() 15. Gibbs, EL, et al. The cross section areas of the vessels that form the torcular and the manner in which flow is distributed to the right and left lateral sinus. Anat Rec. 1934; 59:419–426.
15. Gibbs, EL, et al. The cross section areas of the vessels that form the torcular and the manner in which flow is distributed to the right and left lateral sinus. Anat Rec. 1934; 59:419–426.
![]() 16. Gibbs, EL, et al, Arterial and cerebral venous blood. arterial-venous differences in man. J Biol Chem 1942; 144:325–332.
16. Gibbs, EL, et al, Arterial and cerebral venous blood. arterial-venous differences in man. J Biol Chem 1942; 144:325–332.
![]() 17. Gibbs, FA, et al. Cerebral blood flow preceding and accompanying epileptic seizures in man. Arch Neurol Psychiatry (Chicago). 1934; 32:257–272.
17. Gibbs, FA, et al. Cerebral blood flow preceding and accompanying epileptic seizures in man. Arch Neurol Psychiatry (Chicago). 1934; 32:257–272.
![]() 18. Gopinath, SP. Jugular venous desaturation and outcome after head injury. J Neurol Neurosurg Psychiatry. 1994; 57:717–723.
18. Gopinath, SP. Jugular venous desaturation and outcome after head injury. J Neurol Neurosurg Psychiatry. 1994; 57:717–723.
![]() 19. Graham, D, et al. Brain damage in fatal non-missile head injuries with high intracranial pressure. J Clin Pathol. 1988; 41:34–37.
19. Graham, D, et al. Brain damage in fatal non-missile head injuries with high intracranial pressure. J Clin Pathol. 1988; 41:34–37.
![]() 20. Gupta, AK, et al. Measuring brain tissue oxygenation compared with jugular venous oxygenation after traumatic brain injury. Anesth Analg. 1999; 88:549–553.
20. Gupta, AK, et al. Measuring brain tissue oxygenation compared with jugular venous oxygenation after traumatic brain injury. Anesth Analg. 1999; 88:549–553.
![]() 21. Imberti, R, et al. Cerebral tissue PO2 and SjVO2 changes during moderate hyperventilation in patients with severe traumatic brain injury. J Neurosurg. 2002; 96:91–102.
21. Imberti, R, et al. Cerebral tissue PO2 and SjVO2 changes during moderate hyperventilation in patients with severe traumatic brain injury. J Neurosurg. 2002; 96:91–102.
22. Iwata, M, Kawaguchi, M, Inoue, S, et al. Effects of increasing concentrations of propofol on jugular venous bulb oxygen saturation in neurosurgical patients under normothermic and mildly hypothermic conditions. Anesthesiology. 2006; 104:33–38.
![]() 23. Jakobsen, M, Enevoldsen, E. Retrograde catheterization of the right internal jugular vein for serial measurements of cerebral venous oxygen content. J Cereb Blood Flow Metab. 1989; 9:717–720.
23. Jakobsen, M, Enevoldsen, E. Retrograde catheterization of the right internal jugular vein for serial measurements of cerebral venous oxygen content. J Cereb Blood Flow Metab. 1989; 9:717–720.
![]() 24. Keller, E, et al, Jugular venous oxygen saturation thresholds in trauma patients may not extrapolate to ischemic stroke patients. lessons from a preliminary study. J Neurosurg Anesthesiol 2002; 14:130–136.
24. Keller, E, et al, Jugular venous oxygen saturation thresholds in trauma patients may not extrapolate to ischemic stroke patients. lessons from a preliminary study. J Neurosurg Anesthesiol 2002; 14:130–136.
![]() 25. Kidd, KC, Criddle, L. Using jugular venous catheters in patients with traumatic brain injury. Crit Care Nurse. 2001; 21(6):16–22.
25. Kidd, KC, Criddle, L. Using jugular venous catheters in patients with traumatic brain injury. Crit Care Nurse. 2001; 21(6):16–22.
![]() 26. Kiening, KL, et al, Monitoring of cerebral oxygenation in patients with severe head injuries. brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg 1996; 85:751–757.
26. Kiening, KL, et al, Monitoring of cerebral oxygenation in patients with severe head injuries. brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg 1996; 85:751–757.
![]() 27. Komiyama, M, et al. Marked regional heterogeneity in venous oxygen saturation in severe head injury studied by superselective intracranial venous sampling. Neurosurgery. 1999; 45(6):1469–1472.
27. Komiyama, M, et al. Marked regional heterogeneity in venous oxygen saturation in severe head injury studied by superselective intracranial venous sampling. Neurosurgery. 1999; 45(6):1469–1472.
![]() 28. LeRoux, PD, Cerebral arteriovenous oxygen difference. a predictor of cerebral infarction and outcome in patients with severe head injury. J Neurosurg 1997; 87:1–8.
28. LeRoux, PD, Cerebral arteriovenous oxygen difference. a predictor of cerebral infarction and outcome in patients with severe head injury. J Neurosurg 1997; 87:1–8.
![]() 29. Lubbers, DW, et al. Heterogeneity and stability of local PO2 distribution within the brain tissue. Adv Exp Med Biol. 1994; 345:567–574.
29. Lubbers, DW, et al. Heterogeneity and stability of local PO2 distribution within the brain tissue. Adv Exp Med Biol. 1994; 345:567–574.
![]() 30. March, K, Retrograde jugular catheter. monitoring SjO2. J Neurosci Nurs. 1994; 26(1):48–51.
30. March, K, Retrograde jugular catheter. monitoring SjO2. J Neurosci Nurs. 1994; 26(1):48–51.
![]() 31. Matta, BF, Lam, AM. The rate of blood withdrawal affects the accuracy of jugular venous bulb saturation measurements. Anesthesiology. 1997; 86:806–808.
31. Matta, BF, Lam, AM. The rate of blood withdrawal affects the accuracy of jugular venous bulb saturation measurements. Anesthesiology. 1997; 86:806–808.
![]() 32. Matta, BF, et al. The influence of arterial oxygenation on cerebral venous oxygen saturation during hyperventilation. Can J Anaesth. 1994; 41:1041–1046.
32. Matta, BF, et al. The influence of arterial oxygenation on cerebral venous oxygen saturation during hyperventilation. Can J Anaesth. 1994; 41:1041–1046.
![]() 33. McLeod, AD, et al, Measuring cerebral oxygenation during normobaric hyperoxia. a comparison of tissue microprobes, near-infrared spectroscopy, and jugular venous oximetry in head injury. Anesth Analg 2003; 97:851–856.
33. McLeod, AD, et al, Measuring cerebral oxygenation during normobaric hyperoxia. a comparison of tissue microprobes, near-infrared spectroscopy, and jugular venous oximetry in head injury. Anesth Analg 2003; 97:851–856.
![]() 34. Metz, C, et al, Monitoring of cerebral oxygen metabolism in the jugular bulb. reliability of unilateral measurements in severe head injury. J Cereb Blood Flow Metab 1998; 18:332–343.
34. Metz, C, et al, Monitoring of cerebral oxygen metabolism in the jugular bulb. reliability of unilateral measurements in severe head injury. J Cereb Blood Flow Metab 1998; 18:332–343.
![]() 35. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
35. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
![]() 36. Robertson, CS, et al. Prevention of secondary ischemic insults after severe head injury. Crit Care Med. 1999; 27:2086–2095.
36. Robertson, CS, et al. Prevention of secondary ischemic insults after severe head injury. Crit Care Med. 1999; 27:2086–2095.
![]() 37. Robertson, CS, et al. Cerebral blood flow, arteriovenous oxygen difference, and outcome in head injured patients. J Neurol Neurosurg Psychiatry. 1992; 55:594–603.
37. Robertson, CS, et al. Cerebral blood flow, arteriovenous oxygen difference, and outcome in head injured patients. J Neurol Neurosurg Psychiatry. 1992; 55:594–603.
![]() 38. Ross, DT, et al. Selective loss of neurons from the thalamic reticular nucleus following severe head injury. J Neurotrauma. 1993; 10:151–165.
38. Ross, DT, et al. Selective loss of neurons from the thalamic reticular nucleus following severe head injury. J Neurotrauma. 1993; 10:151–165.
![]() 39. Rossi, S, et al. Brain oxygen tension, oxygen supply, and consumption during arterial hyperoxia in a model of progressive cerebral ischemia. J Neurotrauma. 2001; 18:163–174.
39. Rossi, S, et al. Brain oxygen tension, oxygen supply, and consumption during arterial hyperoxia in a model of progressive cerebral ischemia. J Neurotrauma. 2001; 18:163–174.
![]() 40. Schell, RM, Cole, DJ, Cerebral monitoring. jugular venous oximetry. Anesth Analg 2000; 90:559–566.
40. Schell, RM, Cole, DJ, Cerebral monitoring. jugular venous oximetry. Anesth Analg 2000; 90:559–566.
![]() 41. Sheinberg, M, et al. Continuous monitoring of jugular venous oxygen saturation in head injured patients. J Neurosurg. 1992; 76:212–271.
41. Sheinberg, M, et al. Continuous monitoring of jugular venous oxygen saturation in head injured patients. J Neurosurg. 1992; 76:212–271.
![]() 42. Sikes, PJ, Segal, J. Jugular bulb oxygen saturation monitoring for evaluating cerebral ischemia. Crit Care Nurs Q. 1994; 17(1):9–20.
42. Sikes, PJ, Segal, J. Jugular bulb oxygen saturation monitoring for evaluating cerebral ischemia. Crit Care Nurs Q. 1994; 17(1):9–20.
![]() 43. Stocchetti, N, et al. Cerebral venous oxygen saturation studied with bilateral samples in internal jugular veins. Neurosurgery. 1994; 34:38–43.
43. Stocchetti, N, et al. Cerebral venous oxygen saturation studied with bilateral samples in internal jugular veins. Neurosurgery. 1994; 34:38–43.
![]() 44. Stocchetti, N, et al. Arterio-jugular difference of oxygen content and outcome after head injury. Anesth Analg. 2004; 99:230–234.
44. Stocchetti, N, et al. Arterio-jugular difference of oxygen content and outcome after head injury. Anesth Analg. 2004; 99:230–234.
![]() 45. Struchen, MA, et al. The relation between acute physiological variables and outcomes on the Glasgow Outcomes Scale and Disability Rating Scale following severe traumatic brain injury. J Neurotrauma. 2001; 18:115–125.
45. Struchen, MA, et al. The relation between acute physiological variables and outcomes on the Glasgow Outcomes Scale and Disability Rating Scale following severe traumatic brain injury. J Neurotrauma. 2001; 18:115–125.
![]() 46. van Santbrink, H, et al. Continuous monitoring of partial pressure of brain tissue oxygen in patients with severe head injury. Neurosurgery. 1996; 38:21–31.
46. van Santbrink, H, et al. Continuous monitoring of partial pressure of brain tissue oxygen in patients with severe head injury. Neurosurgery. 1996; 38:21–31.
![]() 47. White, H, Baker, A, Continuous jugular venous oximetry in the neurointensive care unit. a brief review. Can J Anaesth 2002; 49:623–629.
47. White, H, Baker, A, Continuous jugular venous oximetry in the neurointensive care unit. a brief review. Can J Anaesth 2002; 49:623–629.
![]() DeGeorgia, MA, Deogaonkar, A. Multimodal monitoring in the neurological intensive care unit. Neurologist. 2005; 11:45–54.
DeGeorgia, MA, Deogaonkar, A. Multimodal monitoring in the neurological intensive care unit. Neurologist. 2005; 11:45–54.
![]() Kawano, Y, Kawaguchi, M, Inoue, S, et al. Jugular bulb oxygen saturation under propofol or sevoflurane/nitrous oxide -anesthesia during deliberate mild hypothermia in -neurosurgical patients. J Neurosurg Anesthesiol. 2004; 16:6–10.
Kawano, Y, Kawaguchi, M, Inoue, S, et al. Jugular bulb oxygen saturation under propofol or sevoflurane/nitrous oxide -anesthesia during deliberate mild hypothermia in -neurosurgical patients. J Neurosurg Anesthesiol. 2004; 16:6–10.
![]() March, K. Technology. In: Bader MK, Littlejohns LR, eds. Core curriculum for neuroscience nursing. ed 4. Chicago, American Association of Neuroscience Nurses, St Louis: Saunders; 2004:199–226.
March, K. Technology. In: Bader MK, Littlejohns LR, eds. Core curriculum for neuroscience nursing. ed 4. Chicago, American Association of Neuroscience Nurses, St Louis: Saunders; 2004:199–226.
![]() Smythe, PR, Samra, SK. Monitors of cerebral oxygenation. Anesthesiol Clin North Am. 2002; 20:293–313.
Smythe, PR, Samra, SK. Monitors of cerebral oxygenation. Anesthesiol Clin North Am. 2002; 20:293–313.
Wartenberg, KE, Schmidt, JM, Mayer, SA. Multimodality -monitoring in neurocritical care. Crit Care Clin. 2007; 23:507–538.
![]() Yoshitani, K, Kawaguchi, M, Iwata, M, et al. Comparison of changes in jugular venous bulb oxygen saturation and cerebral oxygen saturation during variations of haemoglobin concentration under propofol and sevoflurane anaesthesia. Br J Anaesth. 2005; 94:341–346.
Yoshitani, K, Kawaguchi, M, Iwata, M, et al. Comparison of changes in jugular venous bulb oxygen saturation and cerebral oxygen saturation during variations of haemoglobin concentration under propofol and sevoflurane anaesthesia. Br J Anaesth. 2005; 94:341–346.