Procedure 9 Occipital-Cervical Fusion
Indications
 This procedure is typically performed to treat instability of the occipital-cervical joint—specifically, to ensure stability and protect the neurologic structures, prevent deformity, and reduce or eliminate pain. The presence of occipital-cervical instability increases the risk for compression or trauma to the spinal cord/brainstem by means of pathologic translation, longitudinal displacement, or basilar invagination. The consequences include pain, cranial nerve palsies, respiratory distress, paresis, paralysis, and even sudden death.
This procedure is typically performed to treat instability of the occipital-cervical joint—specifically, to ensure stability and protect the neurologic structures, prevent deformity, and reduce or eliminate pain. The presence of occipital-cervical instability increases the risk for compression or trauma to the spinal cord/brainstem by means of pathologic translation, longitudinal displacement, or basilar invagination. The consequences include pain, cranial nerve palsies, respiratory distress, paresis, paralysis, and even sudden death.
 There are two basic presentations of occipital-cervical instability:
There are two basic presentations of occipital-cervical instability:
Techniques Controversies
• A successful occipital-cervical fusion can provide a favorable outcome in most types of occipital-cervical instability, whether acute or chronic. There are a variety of techniques to obtain a fusion varying from onlay grafts, wiring, plates, and most recent plate/rod constructs. The screw/rod constructs have been shown to provide improved neurologic status postoperatively, decreased instrumentation failure rates, and few postoperative complications.
• However, in patients with neoplasms, posterior wiring and rods have the highest rate of arthrodesis, while screw/rod constructs are associated with a significantly less favorable rate of arthrodesis.
• Still, in patients suffering from inflammatory/autoimmune diseases, screw/rod constructs provide the best outcomes, especially when compared with posterior wiring and inlay in situ bone grafting, which provides poor results postoperatively. Similar results are found in cases of traumatic occipital-cervical instability.
Examination/Imaging
 Anteroposterior (AP) and lateral spine radiographs
Anteroposterior (AP) and lateral spine radiographs
 Cervical spine computed tomography (CT) scan with sagittal and coronal reconstructions
Cervical spine computed tomography (CT) scan with sagittal and coronal reconstructions
 Measurement of reference lines, such as Chamberlain line (posterior of the hard palate to the dorsum of the foramen magnum) and the Wackenheim line (extending the course of the clivus), are of somewhat limited value.
Measurement of reference lines, such as Chamberlain line (posterior of the hard palate to the dorsum of the foramen magnum) and the Wackenheim line (extending the course of the clivus), are of somewhat limited value.
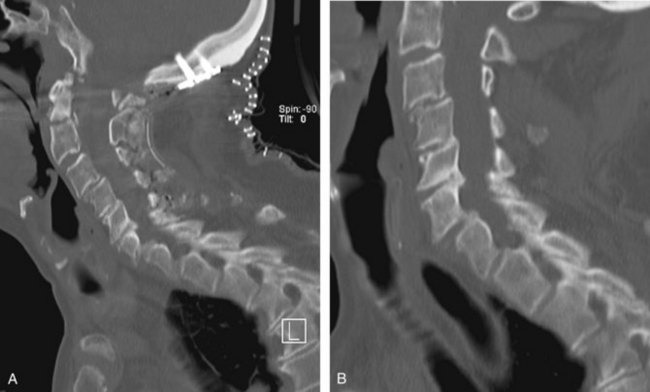
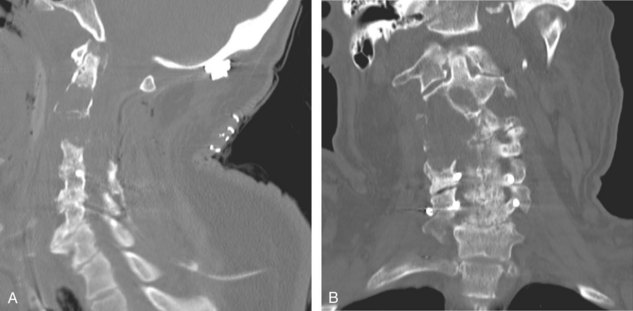
 Obtain magnetic resonance imaging (MRI) of the cervical spine (especially with myelopathy) to determine degree and severity of spinal cord compression (Figure 9-3).
Obtain magnetic resonance imaging (MRI) of the cervical spine (especially with myelopathy) to determine degree and severity of spinal cord compression (Figure 9-3).
 Obtain a myelogram (CT and radiographic) if MRI is not available or is contraindicated (i.e., when the patient has a pacemaker or other MRI-incompatible hardware). Although a myelogram can directly visualize the spinal cord, it also provides valuable information on the degree of compression, or lack of, on the spinal cord.
Obtain a myelogram (CT and radiographic) if MRI is not available or is contraindicated (i.e., when the patient has a pacemaker or other MRI-incompatible hardware). Although a myelogram can directly visualize the spinal cord, it also provides valuable information on the degree of compression, or lack of, on the spinal cord.
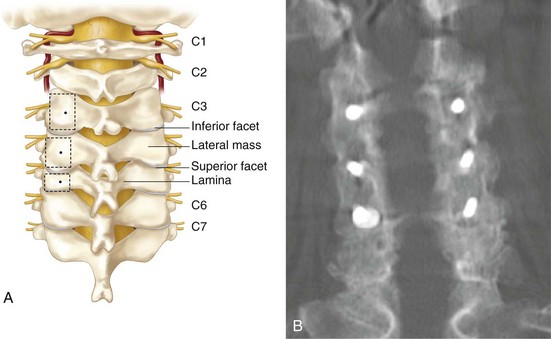
Surgical Anatomy
Positioning
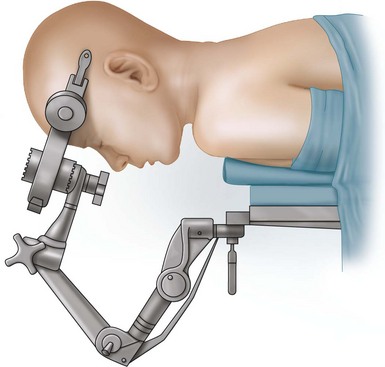
 Place patient in prone position in three-point pin fixation.
Place patient in prone position in three-point pin fixation.
 Alternatively, the patient can be placed in prone position in a halo ring affixed to the table.
Alternatively, the patient can be placed in prone position in a halo ring affixed to the table.
Positioning Pearls
• It is crucial to evaluate the patient’s optimal head position, because with an occipital-cervical fusion, they will be locked in this position.
• The patient must adequately overhang the operating room table.
• The patient’s chest must be supported on gel rolls; a parallel position with respect to the body axis is recommended.
• If the patient is in a hard cervical collar, roll and position him or her with the collar on.
• Include a lower sheet that can be used to support the arms in a sling.
• Place the cervical spine in a neutral position.
• If the patient is in continuous traction, start at 7 lb and increase to 15 lb maximum as necessary.
• Monitor somatosensory evoked potentials (SSEPs) and motor evoked potentials prepositioning and postpositioning.
• Avoid paralytics, because they interfere with neuromonitoring.
Positioning Pitfalls
• Horizontally placed rolls may interfere with chin flexion.
• Proper alignment of cervical spine is critical. Avoid excessive flexion or extension.
• Be aware of chin position during positioning.
• If SSEPs or motor evoked potentials change during positioning, return the patient to the supine position. An option is to administer methylprednisolone per the National Acute Spinal Cord Injury Study (NASCIS II) guidelines.
Portals/Exposures
Portals/Exposures Pearls
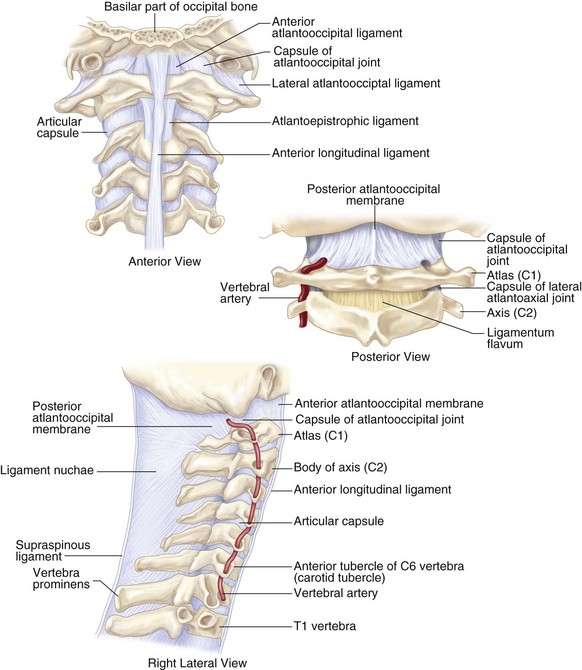
• Care must be taken when exposing the space between the occiput and the C1 interspace. There is a risk of penetrating the dura at this interspace with the Bovie electrocautery or a spinal instrument.
• The vertebral artery lies within the occipital triangle (superior and inferior obliques, rectus capitis). Avoid iatrogenic damage to the artery during lateral dissection.
• Remove soft tissue that could interfere with bony fusion, such as the atlantooccipital membrane, interspinous ligaments, and ligamentum flavum.
Procedure
Step 1
 Position the patient on gel rolls, in pins, in a prone, neutral position (Figure 9-8).
Position the patient on gel rolls, in pins, in a prone, neutral position (Figure 9-8).
 Shave and mark from the inion down the midline to C5.
Shave and mark from the inion down the midline to C5.
Step 1 Pearls
• Avoid excessive flexion/extension; a near-anatomic position is preferred.
• Chin clearance must be obtained.
• Monitoring of SSEPs and motor evoked potentials is recommended.
• If tolerated by the patient, the patient’s neck may be positioned to optimize a surgical approach and then repositioned under fluoroscopic guidance for final fixation.
Step 2: Exposure of Inion to C5
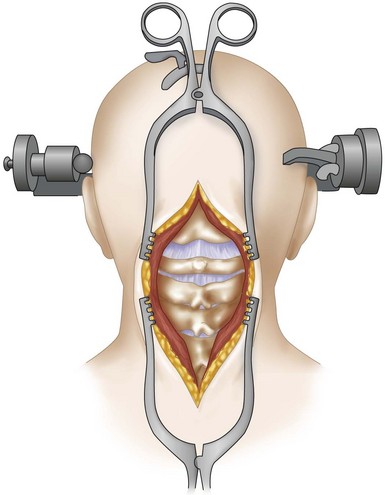
 Dissect using sharp, blunt, and electrocautery dissection down the midline through the following layers (see Figure 9-7):
Dissect using sharp, blunt, and electrocautery dissection down the midline through the following layers (see Figure 9-7):
• Superficial fascia: identify the midline raphe.
• Identify the spinous process and the prevertebral fascia.
• Dissect bilaterally down the spinous processes. Preserve the ligamentum nuchae as much as possible.
• Take care to identify the spinous process of C2 and the ring of C1. Dissection here must be done very cautiously to avoid entering the occipital, C1, or C2 spaces or the C1-2 interspace.
• Expose laterally to identify lateral masses.
• Expose anteriorly to identify the inion.
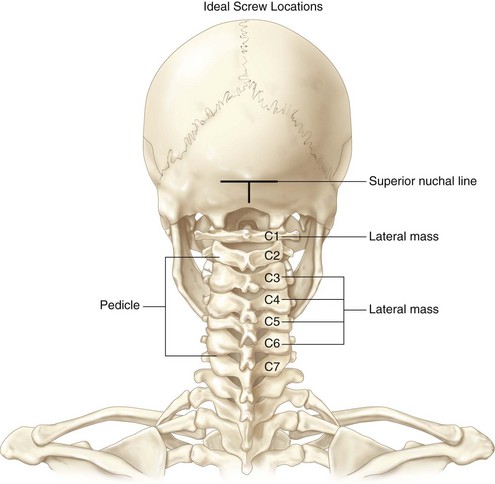
• At a minimum, bony exposure of occiput to C2 lateral masses must be achieved. Expose lower lateral masses as needed.
Step 3: Instrumentation and Fusion
 Place the occipital Kiel plate in the midline (Figure 9-9).
Place the occipital Kiel plate in the midline (Figure 9-9).
 Place an isthmus or pedicle screw at C2. (Expose the lateral masses of distal vertebrae as needed.)
Place an isthmus or pedicle screw at C2. (Expose the lateral masses of distal vertebrae as needed.)
 Contour the rods to the approximate neutral position of the occipital-cervical junction. The rod bend should be approximately a 130-degree angle, but this will vary with each patient.
Contour the rods to the approximate neutral position of the occipital-cervical junction. The rod bend should be approximately a 130-degree angle, but this will vary with each patient.
 Connect the rods to the Kiel plate and screw.
Connect the rods to the Kiel plate and screw.
 Decorticate the occipital-cervical junction.
Decorticate the occipital-cervical junction.
 Pack the construct with autologous/allograft material to encourage fusion.
Pack the construct with autologous/allograft material to encourage fusion.
Step 3 Pearls
• Create the shortest construct possible without sacrificing stability. Longer constructs tend to minimize mobility; on the other hand, to short a construct may be inadequate for creating appropriate stability.
• In traumatic injury, the construct should include the first two levels with normal ligamentous anatomy.
Postoperative Care and Expected Outcomes
 Place the patient in a hard collar for 6 to 12 weeks with radiographic follow-up.
Place the patient in a hard collar for 6 to 12 weeks with radiographic follow-up.
 After 6 to 12 weeks, flexion/extension views should be obtained to determine if fusion is noted radiographically.
After 6 to 12 weeks, flexion/extension views should be obtained to determine if fusion is noted radiographically.
 Approximately 80% fusion rates are expected.
Approximately 80% fusion rates are expected.
 Complications include infection, neurovascular compromise from instrumentation, subdural or subarachnoid hematoma resulting from instrumentation placement, cerebrospinal fluid-flow abnormalities resulting from instrumentation placement, pullout of screws/plate/instrumentation, and fracture/migration of instrumentation.
Complications include infection, neurovascular compromise from instrumentation, subdural or subarachnoid hematoma resulting from instrumentation placement, cerebrospinal fluid-flow abnormalities resulting from instrumentation placement, pullout of screws/plate/instrumentation, and fracture/migration of instrumentation.
Abumi K, Takada T, Shono Y, Kaneda K, Fujiya M. Posterior occipitocervical reconstruction using cervical pedicle screws and plate-rod systems. Spine. 1999;24:1425-1434.
Deutsch H, Haid JrRW, Rodts JrGE, Mummaneni PV. Occipitocervical fixation: long-term results. Spine. 2005;30:530-535.
Dvorak MF, Sekeramayi F, Zhu Q, et al. Anterior occiput to axis screw fixation. Part II: a biomechanical comparison with posterior fixation techniques. Spine. 2003;28:239-245.
Fehlings MG, Cadotte DW. Occipital cervical fusion: an evolution of techniques. J Neurosurg Spine. 2010;13:3-4.
Lee SC, Chen JF, Lee ST. Complications of fixation to the occiput—anatomical and design implications. Br J Neurosurg. 2004;18:590-597.
Menezes AH, Sonntag VKH, editors. Principles of Spinal Surgery. New York: McGraw-Hill;, 1996.
Oda I, Abumi K, Sell LC, et al. Biomechanical evaluation of five different occipito-atlanto-axial fixation techniques. Spine. 1999;24:2377-2382.
Schmidek HH, Sweet WH, editors: Schmidek & Sweet’s Operative Neurosurgical Techniques: Indications, Methods, and Results. Philadelphia;WB Saunders: 2000:1934-1945
Takechi Y, Iizuka H, Sorimachi Y, et al. Non-traumatic posterior atlanto-occipital joint dislocation. Case report. Eur Spine J. 2010;20(Suppl 2):S172-S175.
Vaccaro AR, Betz RR, Zeidman SM, editors: Principles and Practice of Spine Surgery. St Louis;CV Mosby: 2003:723-725
Vender JR, Rekito AJ, Harrison SJ, McDonnell DE. The evolution of posterior cervical and occipitocervical fusion and instrumentation. Neurosurg Focus. 2004;16:e9.
Winegar CD, Lawrence JP, Friel BC, et al. A systematic review of occipital cervical fusion: techniques and outcomes. A review. J Neurosurg Spine. 2010;13:5-16.
Winn HR, Youmans JR, Winn HR, Youmans JR, editors. Youmans Neurological Surgery. Philadelphia: WB Saunders, 2004.