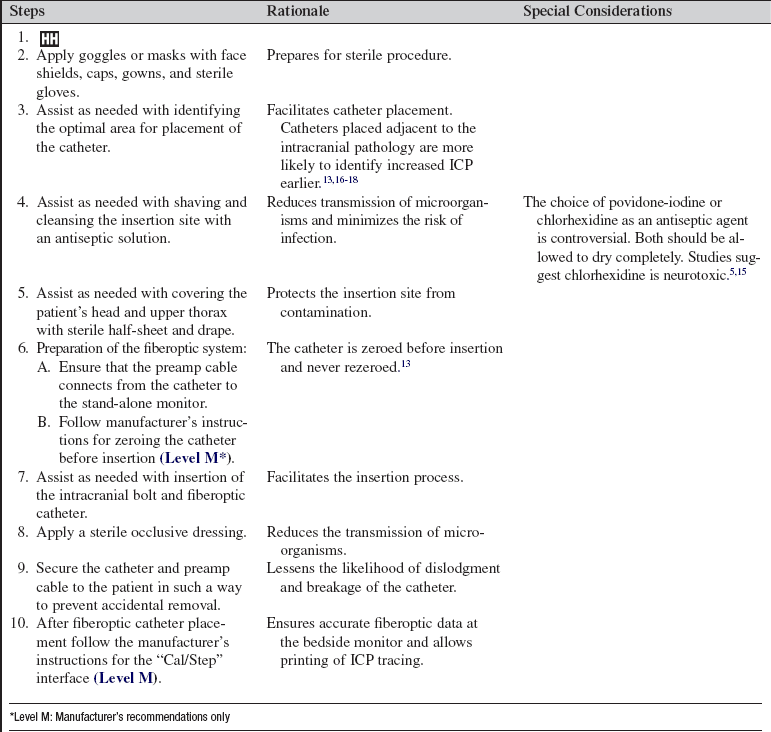
Intracranial Bolt and Fiberoptic Catheter Insertion (Assist), Intracranial Pressure Monitoring, Care, Troubleshooting, and Removal
PREREQUISITE NURSING KNOWLEDGE
• A fundamental understanding of neuroanatomy and physiology is needed.
• Knowledge of aseptic and sterile technique is necessary.
• Proper equipment assembly and setup specific to the fiberoptic intracranial pressure monitoring device must be understood.
• Intracranial pressure (ICP) is the pressure exerted by the intracranial contents, brain tissue, blood and cerebrospinal fluid (CSF). Increased intracranial pressure occurs when the intracranial volume exceeds the brain’s ability to compensate for increased volume.13
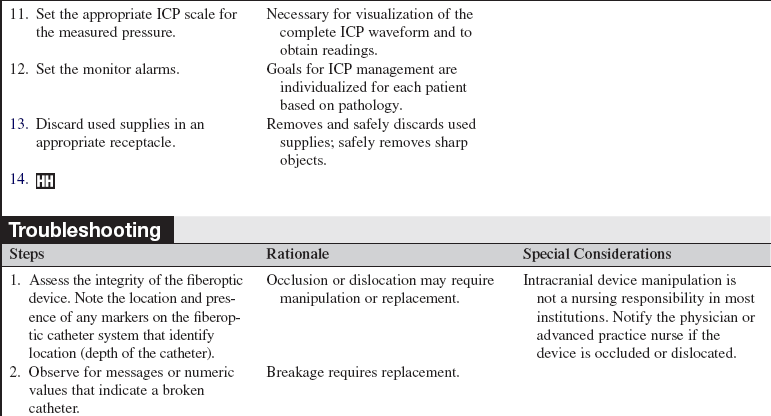
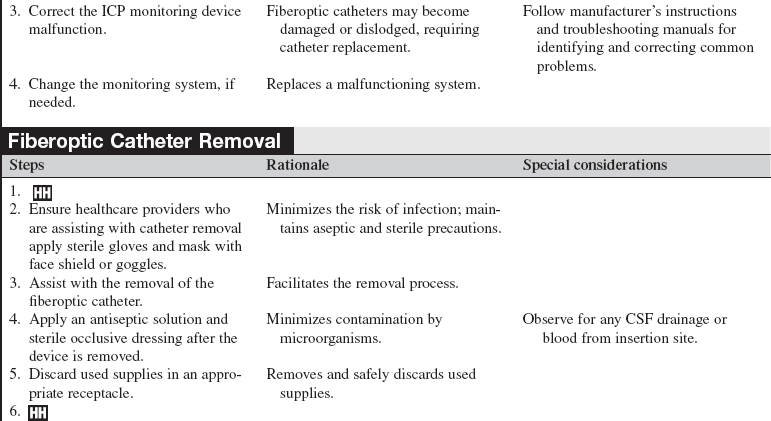
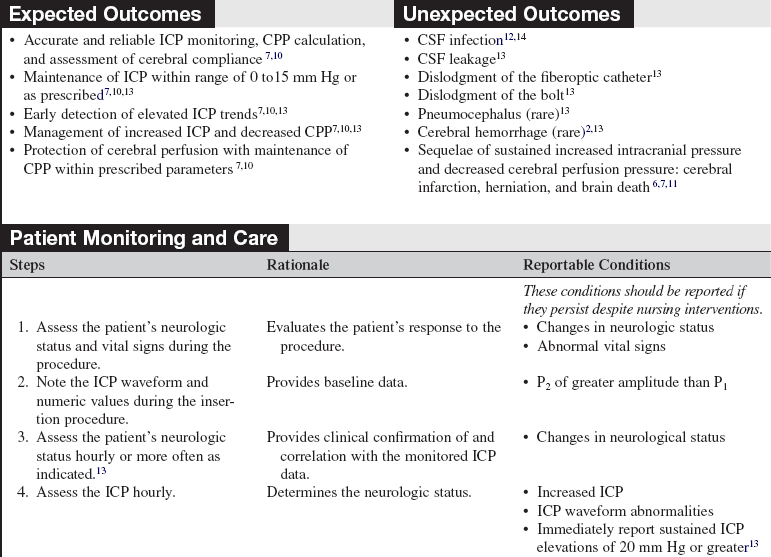
• Normal ICP ranges from 0 to 15 mm Hg; sustained ICPs of greater than 20 mm Hg are generally considered neurologic emergencies.3,10
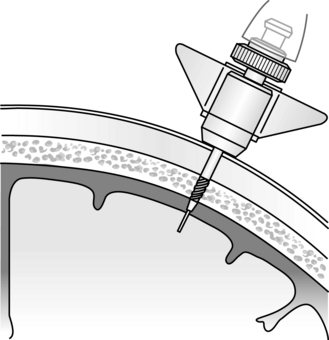
• ICP is measured via a catheter inserted into the brain parenchyma. The catheter is inserted through an intracranial bolt (Fig. 88-1).
• The normal ICP waveform has three or four peaks with P1 of greater amplitude than P2 and P3. P1 is thought to reflect arterial pressure; P2 and P3 and P4 (when present) have been described as choroid plexus or venous in origin (Fig. 88-2).13 The amplitude of P2 may exceed P1 with increased ICP or decreased intracranial compliance (Fig. 88-3).
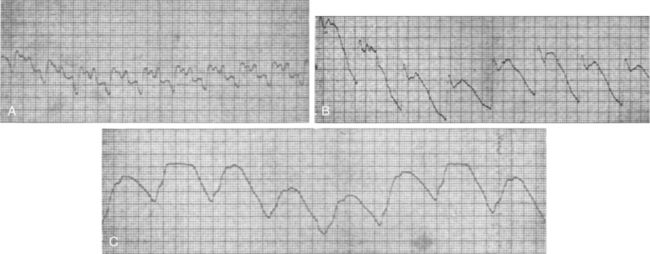
Figure 88-3 Example of intracranial pressure waveforms with P2 elevation indicating decreased cerebral compliance.
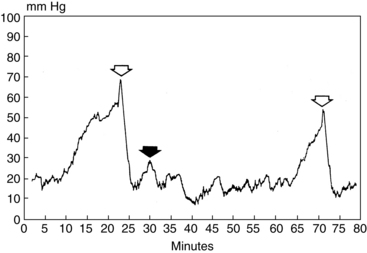
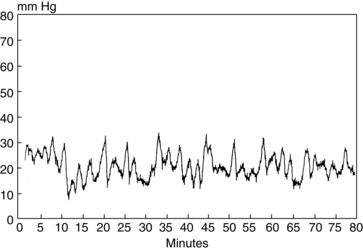
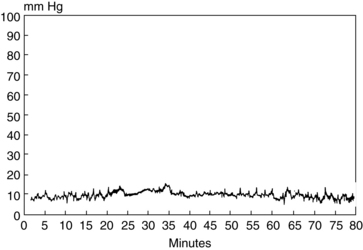
• ICP waveform trends include a, b, and c waves. The a waves, also referred to as plateau waves, are associated with ICP values of 50 to 100 mm Hg and last 5 to 20 minutes. The a waves (Fig. 88-4) are associated with abrupt neurologic deterioration and herniation. The b waves (Fig 88-5), with ICP values of 20 to 50 mm Hg and lasting 30 seconds to 2 minutes, may become a waves. The c waves (Fig. 88-6) may coincide with ICPs as high as 20 mm Hg but are short lasting and without clinical significance.1
• Cerebral perfusion pressure (CPP) is the pressure at which the brain is perfused. CPP is calculated by subtracting the ICP from the mean arterial pressure (MAP). Normal CPP is thought to be approximately 80 mm Hg.11 In severe traumatic brain injury, the CPP for adults should range between 50 and 70 mm Hg.2 Patients with other neurologic injuries may require individualized CPP parameters reflective of the neuropathology and brain perfusion needs. Research continues regarding the relationship between cerebral blood flow and CPP.
• ICP and CPP must be considered together in management of the patient. Cerebral autoregulation is the intrinsic ability of the cerebral vessels to constrict and dilate as needed to maintain adequate cerebral perfusion. Cerebral autoregulation is impaired with brain injury and the cerebral blood flow becomes passively dependent on the systemic blood pressure. The cerebral blood vessels are no longer able to react to maintain CPP in response to a change in blood pressure.3
• Sustained ICP elevations of 20 mm Hg or greater necessitate immediate reporting and intervention. ICP waveform changes that indicate loss of cerebral compliance or cerebral autoregulation should be reported immediately.8,10,13
• ICP monitoring is indicated for the following:
 Traumatic brain injury with a Glasgow Coma Scale score of less than or equal to 8 and abnormal computed tomography (CT) scan results or normal CT scan results with two of the following: hypotension; greater than 40 years of age; and motor posturing2
Traumatic brain injury with a Glasgow Coma Scale score of less than or equal to 8 and abnormal computed tomography (CT) scan results or normal CT scan results with two of the following: hypotension; greater than 40 years of age; and motor posturing2
 Fulminant hepatic failure with encephalopathy13
Fulminant hepatic failure with encephalopathy13
• Contraindications for ICP monitoring include infection and coagulopathies.
• Concerns with accuracy of ICP monitoring values primarily relate to displacement, misplacement, or breakage of the catheter and drift (especially after 5 days).11,13
• Management of the patient with increased ICP and decreased CPP is a multi-tiered approach that includes positioning, maintaining normothermia, administration of pharmacologic agents, and surgical procedures.6,9
EQUIPMENT
• Sterile gloves, surgical caps, masks, goggles or face shields, and sterile surgical gowns
• Sterile towels, half-sheets, and drapes
• Local anesthetic (lidocaine 1% or 2% without epinephrine), 5-ml or 10-mL Luer-Lok syringe with 18-gauge needle (for drawing up lidocaine), and 23-gauge or 25-gauge needle (for administration of lidocaine)
PATIENT AND FAMILY EDUCATION
• Assess patient and family understanding of fiberoptic catheters.  Rationale: Explanations to patient and family specific needs may allay fears.
Rationale: Explanations to patient and family specific needs may allay fears.
• Explain the fiberoptic catheter insertion procedure. Review normal parameters and patient care after insertion. Review the family’s role in maintenance of an optimal ICP with limitation of patient stimulation.  Rationale: Explanation of expected interventions may allay patient and family anxieties, encourage questions, and promote therapeutic family interaction.
Rationale: Explanation of expected interventions may allay patient and family anxieties, encourage questions, and promote therapeutic family interaction.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s neurologic status and vital signs.  Rationale: Performing a baseline neurologic assessment enables the nurse to identify changes that may occur during or as a result of the fiberoptic catheter placement.
Rationale: Performing a baseline neurologic assessment enables the nurse to identify changes that may occur during or as a result of the fiberoptic catheter placement.
• Assess the patient’s current laboratory profile, including complete blood count (CBC) or platelet count, prothrombin time (PT), international normalized ratio (INR), and partial thromboplastin time (PTT).  Rationale: Baseline coagulation study results determine the risk for bleeding during intracranial bolt and catheter insertion.
Rationale: Baseline coagulation study results determine the risk for bleeding during intracranial bolt and catheter insertion.
• Assess for allergies.  Rationale: Assessment minimizes the risk of allergic reaction.
Rationale: Assessment minimizes the risk of allergic reaction.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Ensure that informed consent has been obtained.  Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow for the consent form to be signed.
Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow for the consent form to be signed.
• Administer preprocedural analgesia or sedation as prescribed.  Rationale: The patient needs to remain still during fiberoptic catheter insertion. In an emergency situation, the patient may already be receiving continuous analgesia and sedation.
Rationale: The patient needs to remain still during fiberoptic catheter insertion. In an emergency situation, the patient may already be receiving continuous analgesia and sedation.
• Assist the patient to a supine position with the head of the bed at 30 to 45 degrees and the neck in a midline, neutral position.  Rationale: This position provides access for fiberoptic catheter insertion and enhances jugular venous outflow, contributing to possible reduction in intracranial pressure.
Rationale: This position provides access for fiberoptic catheter insertion and enhances jugular venous outflow, contributing to possible reduction in intracranial pressure.
References
1. Bershad, EM, Humphreis, WE, Suarez, JI. Intracranial hypertension. Semin Neurol. 2008; 28:690–702.
2. Bratton, SL, Chesnut, RM, Ghajar, J, et al, Guidelines for the management of severe traumatic brain injury. a joint project of the Brain Trauma Foundation, American Association of Neurological Surgeons (AANS), Congress of Neurological Surgeons (CNS), AANS/CNS Joint Section on Neurotrauma and Critical Care. J Neurotrauma. 2007; 24(Suppl 1):S1–S106.
![]() 3. Davis, JW, Davis, IC, Bennink, LD, et al, Placement of intracranial pressure monitors. are “normal” coagulation parameters necessary. J Trauma 2004; 57:1173–1177.
3. Davis, JW, Davis, IC, Bennink, LD, et al, Placement of intracranial pressure monitors. are “normal” coagulation parameters necessary. J Trauma 2004; 57:1173–1177.
4. Fan J-Y, Kirkness, C, Vicini, P, et al. Intracranial pressure waveform morphology and intracranial adaptive capacity. Am J Crit Care. 2008; 17:545–554.
5. Hebl, JR. The importance and implications of aseptic techniques during regional anesthesia. Reg Anesth Pain Med. 2006; 31:311–323.
6. Hickey, JV, Olson, DM, Intracranial hypertension. theory and management of increased intracranial pressure Hickey JV, ed.. The clinical practice of neurological and neurosurgical nursing. ed 6. Lippincott Williams & Wilkins, Philadelphia, 2009:270–307.
![]() 7. Josephson, L. Management of increased intracranial pressure. Dimens Crit Care Nurs. 2004; 23:194–207.
7. Josephson, L. Management of increased intracranial pressure. Dimens Crit Care Nurs. 2004; 23:194–207.
![]() 8. Kirkness, CJ, Mitchell, PH, Burr, RL, et al, Intracranial pressure waveform analysis. clinical and research implications. J Neurosci Nurs 2000; 32:271–277.
8. Kirkness, CJ, Mitchell, PH, Burr, RL, et al, Intracranial pressure waveform analysis. clinical and research implications. J Neurosci Nurs 2000; 32:271–277.
![]() 9. March, K. Application of technology in the treatment of traumatic brain injury. Crit Care Nurs Q. 2000; 23:26–37.
9. March, K. Application of technology in the treatment of traumatic brain injury. Crit Care Nurs Q. 2000; 23:26–37.
![]() 10. March, K. Intracranial pressure monitoring and assessing intracranial compliance in brain injury. Crit Care Nurs Clin North Am. 2002; 12:429–436.
10. March, K. Intracranial pressure monitoring and assessing intracranial compliance in brain injury. Crit Care Nurs Clin North Am. 2002; 12:429–436.
![]() 11. March, K. Technology. In: Bader MK, Littlejohns LR, eds. AANN core curriculum for neuroscience nursing. ed 4. St Louis: Saunders; 2004:199–202.
11. March, K. Technology. In: Bader MK, Littlejohns LR, eds. AANN core curriculum for neuroscience nursing. ed 4. St Louis: Saunders; 2004:199–202.
March, K, Intracranial pressure monitoring. why monitor. AACN Clin Issues 2005; 16:456–475.
13. March, K, Madden, L. Intracranial pressure management. In: Littlejohns LR, Bader MK, eds. AACN-AANN protocols for practice: monitoring technologies in critically ill neuroscience patients. Sudbury, MA: Jones and Bartlett; 2009:35–69.
![]() 14. O’Grady, NP, Alexander, M, Dellinger, EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
14. O’Grady, NP, Alexander, M, Dellinger, EP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
15. Reynolds, F. Neurologic infection after neuraxial anesthesia. Anesthesiol Clin. 2008; 26:23–52.
![]() 16. Sahuqillo, J, Poca, M, Arribas, M, et al, Interhemispheric supratentorial intracranial pressure gradients in head-injured patients. are they clinically important. J Neurosurg 1999; 90:16–26.
16. Sahuqillo, J, Poca, M, Arribas, M, et al, Interhemispheric supratentorial intracranial pressure gradients in head-injured patients. are they clinically important. J Neurosurg 1999; 90:16–26.
![]() 17. Slavin, KV, Misra, M, Infratentorial intracranial pressure monitoring in the neurosurgical intensive care unit. Neurol Res 2003; 25:880–884.
17. Slavin, KV, Misra, M, Infratentorial intracranial pressure monitoring in the neurosurgical intensive care unit. Neurol Res 2003; 25:880–884.
![]() 18. Wolfla, CE, Luerssen, TG, Bowman, RM, et al. Brain tissue pressure gradients created by expanding frontal epidural mass lesion. J Neurosurg. 1996; 84:642–647.
18. Wolfla, CE, Luerssen, TG, Bowman, RM, et al. Brain tissue pressure gradients created by expanding frontal epidural mass lesion. J Neurosurg. 1996; 84:642–647.