Central Venous Catheter Insertion (Assist)
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the normal anatomy and physiology of the cardiovascular system is needed.
• Knowledge of the anatomy and physiology of the vasculature and adjacent structures of the neck, groin, and arm is necessary.
• Basic dysrhythmia interpretation should be understood.
• Understanding of aseptic technique is necessary. Prevention of infection is a significant concern for patients with indwelling catheters.
• Advanced cardiac life support knowledge and skills are needed.
• Indications for a central venous catheter include the following4,7:
 Hypotension after major surgery
Hypotension after major surgery
 Right ventricular ischemia or infarction
Right ventricular ischemia or infarction
 Administration of total parenteral nutrition or other hyperosmolar solutions
Administration of total parenteral nutrition or other hyperosmolar solutions
 Lack of peripheral venous access
Lack of peripheral venous access
 Assessment of hypovolemia or hypervolemia
Assessment of hypovolemia or hypervolemia
 Monitoring of central venous catheter (CVC) pressure
Monitoring of central venous catheter (CVC) pressure
 Long-term infusion of medications
Long-term infusion of medications
• Relative contraindications of CVC insertion include the following4,7:
 Presence of a permanent pacemaker
Presence of a permanent pacemaker
 Obstruction of the superior or inferior vena cava, innominate vein, subclavian veins, or internal jugular veins
Obstruction of the superior or inferior vena cava, innominate vein, subclavian veins, or internal jugular veins
• The central venous pressure (CVP) provides information regarding right heart filling pressures and right ventricular function and volume.
• The CVP historically was measured with a water manometer system but now is measured with a single-pressure transducer system (see Procedures 70 and 76).
• The CVP waveform is identical to the right atrial pressure (RAP) waveform.
• The normal CVP value is 2 to 6 mm Hg.
• Electrocardiographic (ECG) monitoring is essential in determination of accurate interpretation of the CVP value.
• Understanding of a, c, and v waves is necessary. The a wave reflects right atrial contraction, the c wave reflects closure of the tricuspid valve, and the v wave reflects right atrial filling during ventricular systole (see Figs. 70-1 and 73-7).
• Dysrhythmias may alter CVP or RAP waveforms.
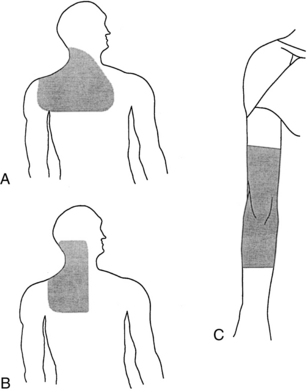
• The risk for a pneumothorax is minimized with use of an internal jugular vein. The preferred site for catheter insertion is the right internal jugular vein. The right internal jugular vein is a “straight shot” to the right atrium.
• The right and left subclavian veins are also sites for central catheter placement. Placement of a central catheter through the right subclavian vein is a shorter and more direct route than through the left subclavian vein because it does not cross the midline of the thorax.
• Femoral veins may be accessed but have the disadvantage of forcing the patient to be on bed rest with immobilization of that leg and of an increased risk for infection.
• The presence of a pacemaker may alter the choice of placement of a CVC because of a risk for dislodging pacemaker leads with insertion of a CVC.
• Complications may occur during or after insertion of a CVC (see Table 81-1).
EQUIPMENT
• CVC of choice (single, dual, or triple lumen) usually supplied with insertion needle, dilator, syringe, and guidewire
• Large sterile drapes or towels
• 1% lidocaine without epinephrine
• Large package of 4 × 4 gauze sponges
• Suture kit (hemostat, scissors, needle holder)
• 3-0 or 4-0 nylon suture with curved needle
• Syringes: One 10-mL to 12-mL syringe; two 3- to 5-mL syringes; two 22-gauge, 1½-inch needles
• Face masks, head coverings, goggles (shield and mask combination may be used), sterile gloves, and sterile gowns
• Skin protectant pads or swab sticks
• Chlorhexidine-impregnated sponge
• Antiseptic solution (e.g., 2% chlorhexidine–based preparation)
Additional equipment as needed includes the following:
• Hemodynamic monitoring system (see Procedure 76)
• Intravenous (IV) solution with Luer-Lok administration set for IV infusion
• Sutureless catheter securement device
• Bedside monitor and oscilloscope with pulse oximetry
• Supplemental oxygen supplies
• Package of alcohol pads or swab sticks
PATIENT AND FAMILY EDUCATION
• Explain the need for the CVC insertion and assess patient and family understanding.  Rationale: Clarification and understanding of information decrease patient and family anxiety levels.
Rationale: Clarification and understanding of information decrease patient and family anxiety levels.
• Explain the required positioning for the procedure and the importance of the patient not moving during the insertion.  Rationale: This explanation encourages cooperation and reduces anxiety.
Rationale: This explanation encourages cooperation and reduces anxiety.
• Explain the need for sterile technique and that the patient’s face may be covered.  Rationale: The explanation decreases patient anxiety and elicits cooperation.
Rationale: The explanation decreases patient anxiety and elicits cooperation.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s vital signs and pulse oximetry.  Rationale: Baseline data are provided.
Rationale: Baseline data are provided.
• Assess the patient’s cardiac and pulmonary status.  Rationale: Some patients may not tolerate a supine or Trendelenburg’s position for extended periods.
Rationale: Some patients may not tolerate a supine or Trendelenburg’s position for extended periods.
• Assess electrolyte levels (e.g., potassium, magnesium, calcium).  Rationale: Electrolyte abnormalities may increase cardiac irritability.
Rationale: Electrolyte abnormalities may increase cardiac irritability.
• Assess the patient’s coagulopathic status and determine whether the patient has recently received anticoagulant or thrombolytic therapy.  Rationale: These patients are more likely to have complications related to bleeding and may need interventions before insertion of the CVC.
Rationale: These patients are more likely to have complications related to bleeding and may need interventions before insertion of the CVC.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Ensure that informed consent was obtained.  Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow for this form to be signed.
Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow for this form to be signed.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Administer prescribed sedation or analgesics as needed.  Rationale: The patient may need sedation or analgesia to ensure adequate cooperation and appropriate placement. During the procedure, restlessness and an altered level of consciousness may represent a pneumothorax, hypoxia, or placement in the carotid artery.
Rationale: The patient may need sedation or analgesia to ensure adequate cooperation and appropriate placement. During the procedure, restlessness and an altered level of consciousness may represent a pneumothorax, hypoxia, or placement in the carotid artery.
• If the patient is obese or muscular and the preferred site is the internal jugular vein or subclavian vein, assist with placing a towel posteriorly between the shoulder blades.  Rationale: This placement helps extend the neck and provides better access to the subclavian and internal jugular veins.
Rationale: This placement helps extend the neck and provides better access to the subclavian and internal jugular veins.
References
![]() 1. Eyer, S, et al, Catheter-related sepsis. prospective, randomized study of three methods of long-term catheter maintenance. Crit Care Med 1990; 18:1073–1079.
1. Eyer, S, et al, Catheter-related sepsis. prospective, randomized study of three methods of long-term catheter maintenance. Crit Care Med 1990; 18:1073–1079.
2. Infusion Nurses Society. (2006). Policies and procedures for infusion nursing.,, ed 3. Norwood, MA: AuthorINS; 2006.
![]() 3. Intravenous Nurses Society. Infusion nursing standards of practice. J Infus Nurs. 2006; 29(1S):S1–S90. [(2006)].
3. Intravenous Nurses Society. Infusion nursing standards of practice. J Infus Nurs. 2006; 29(1S):S1–S90. [(2006)].
4. Kumar, A, Darovic, GO. Establishment of cardiovascular access. In: Darovic, GO, eds. Hemodynamic monitoring invasive and noninvasive clinical application. Philadelphia: Saunders, 2000.
![]() 5. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
5. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
![]() 6. Safdar, N, Klugar, DM, Maki, DG, A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters. implications for preventive strategies. Medicine 2002; 81:466–472.
6. Safdar, N, Klugar, DM, Maki, DG, A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters. implications for preventive strategies. Medicine 2002; 81:466–472.
7. Venus, G, Mallory, DL. Vascular cannulation. In Civetta J, Taylor W. &, Kirby R, eds. : Critical Care, ed 5, Philadelphia: Lippincott, Williams & Wilkins, 2009.
Dailey, EK, Schroeder, JS. Techniques in bedside hemodynamic monitoring, ed 5. St Louis: Mosby; 1994.
Darovic, GO. Hemodynamic monitoring invasive and noninvasive clinical application. Philadelphia: Saunders; 2000.
Eggimann, P, et al. Impact of a prevention strategy targeted at vascular-access care on incidence of infections acquired in intensive care. Lancet. 2000; 355:1864–1868.
Friesinger, GC, Williams, SV, ACP/AHA Task Force on Clinical Privileges in Cardiology. Clinical competence in hemodynamic monitoring. J Am Coll Cardiol 1990; 15:1460.
Lorente, L, Henry, C, Martin, M, et al. Central venous catheter-related infection in a prospective and observational study of 2,595 catheters. Crit Care. 2005; 9:R631–R635.