History
Current Medications
Current Symptoms
Comments
Physical Examination
Comments
Laboratory Data
Electrocardiogram
Findings
Comments
Chest Radiograph
Comments
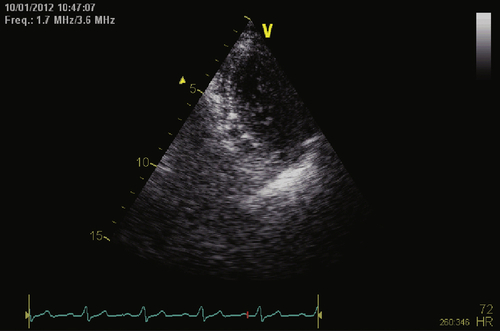
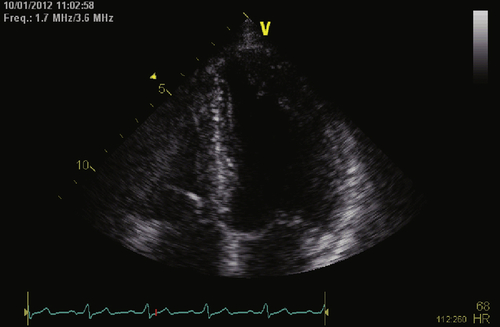
Echocardiogram
Findings
Findings
Magnetic Resonance Imaging
Catheterization
Hemodynamics
Findings
Comments
Focused Clinical Questions and Discussion Points
Question
Discussion
Question
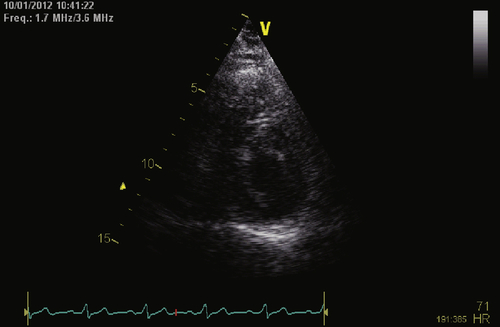
FIGURE 8-3 Short axis view. See expertconsult.com for video. ![]()
Discussion
Question
Discussion
Question
Discussion
Final Diagnosis
Plan of Action
Intervention
Outcome
Comments
Selected References
1. Chan J.Y., Fang F., Zhang Q. et al. Biventricular pacing is superior to right ventricular pacing in bradycardia patients with preserved systolic function: 2-year results of the PACE trial. Eur Heart J. 2011;32:2533–2540.
2. Epstein A.E., DiMarco J.P., Ellenbogen K.A. et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices); American Association for Thoracic Surgery; Society of Thoracic Surgeons. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. J Am Coll Cardiol. 2008;51:e1–e62.
3. Vardas P.E., Auricchio A., Blanc J.J. et al. European Society of Cardiology; European Heart Rhythm Association. Guidelines for cardiac pacing and cardiac resynchronization therapy: The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Eur Heart J. 2007;28:2256–2295.
4. Wilkoff B.L., Cook J.R., Epstein A.E. et al. Dual-chamber pacing or ventricular backup pacing in patients with an implantable defibrillator: the Dual Chamber and VVI Implantable Defibrillator (DAVID) Trial. JAMA. 2002;288:3115–3123.
5. Yu C.M., Chan J.Y., Zhang Q. et al. Biventricular pacing in patients with bradycardia and normal ejection fraction. N Engl J Med. 2009;361:2123–2134.